Translate this page into:
Imaging Techniques in Endodontics: An Overview
Address for correspondence: Dr. Deepak B.S, #376-2, 4th Main, 8th Cross, P.J. Extension, Davangere-577002, Karnataka State, India. deepakdvg@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
This review provides an overview of the relevance of imaging techniques such as, computed tomography, cone beam computed tomography, and ultrasound, to endodontic practice. Many limitations of the conventional radiographic techniques have been overcome by the newer methods. Advantages and disadvantages of various imaging techniques in endodontic practice are also discussed.
Keywords
Computed tomography
cone beam computed tomography
cone beam volumetric tomography
endodontics
radiovisiography
ultrasound
INTRODUCTION

Radiographs are the most accurate and least subjective diagnostic aids available to endodontists for diagnosis of diseases affecting the maxilla and mandible. Conventional X-rays using an analog film or digital receptor produce two-dimensional (2D) image of a three-dimensional (3D) object. The anatomical structures surrounding the tooth, superimpose and make it difficult to interpret the conventional X-ray image.[1– 3] Radiographs are an important part of root canal therapy, especially for diagnosis, treatment, and follow-up. However, routine radiographic procedures do not accurately demonstrate the presence of every lesion, the real size of the lesion or its spatial relationship with the anatomical structures.[4] Newer imaging techniques in use include: Digital imaging systems (Direct, Indirect, Optically scanned), Computed tomography (CT), Tuned aperture computed tomography (TACT), Localized computed tomography (micro-computed tomography), Ultrasonography, Magnetic resonance Imaging (MRI), Radioisotope imaging, Single photon emission computed tomography (SPECT), Positron emission tomography (PET), Cone beam volumetric tomography (CBVT), Radio visiography (RVG), and Denta scan.[5–7]
Imaging plays an important role in endodontics and is routinely utilized for the following diagnosis[Table 1].
The improvements in imaging technology have helped in obtaining a near perfect image for accurate diagnosis. Advantages and disadvantages of various imaging techniques in endodontic are presented.
Ultrasound in endodontics
Ultrasound (US) and Magnetic resonance imaging do not expose patients to any radiation. Ultrasound uses sound waves with a frequency outside the range of human hearing (20 kHz) and can be used to view normal and pathological conditions involving the bones and soft tissues of the oral and maxillofacial regions.[8] US is a valuable technique that can be used in place of conventional X-rays as it has a greater ability to differentiate between cystic and non-cystic lesions.[9] The alveolar bone appears as a total reflecting surface (white), if healthy; the root contours of the teeth are even whiter (hyperechoic). A fluid-filled cavity in the bone appears as a hypo-reflecting surface (dark). The degree of reflection depends on the clarity of the fluid (hypoechoic). A simple serous filled cavity has no reflection (anechoic or transonic). Solid lesions in the bone have a mixed echogenic appearance, which means their echoes are reflected with various intensities (shades of gray). If the bone is irregular or resorbed in the proximity of the lesion, the scan is seen as an inhomogeneous echo. If the bony contour limiting a lesion is reinforced, then it is very bright.[10]
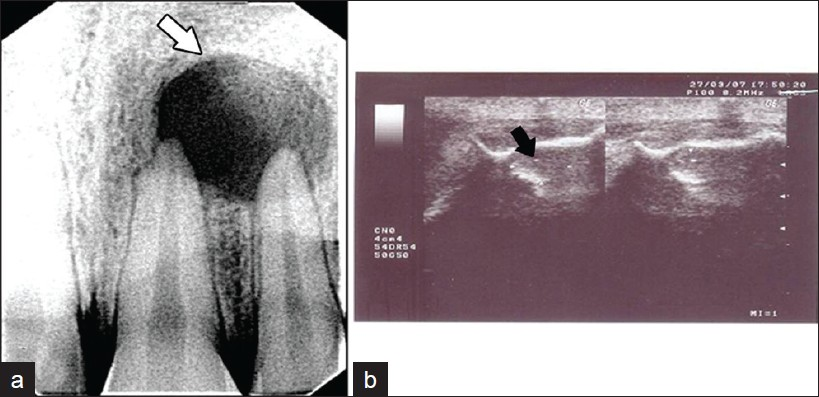
Ultrasound in dentistry is used for the detection of fractures in the facial region, to detect parotid lesions during fine needle aspiration cytology, to assess the content of the lesions before surgery[Figure 1].[11] However, US is difficult to use in the posterior region of the oral cavity, because the thick cortical plate in the posterior region prevents ultrasound waves from traversing easily. Results of selected ultrasound studies are summarized in Table 2.
- (a-b) Radiovisio graphic (RVG) and Ultrasound (US) images of a periapical lesion (1a) RVG image shows a well-circumscribed, radiolucent, periapical lesion with a sclerotic border, measuring about 2 – 1 cm in diameter (white arrow) (1b) USG shows a hypoechoic, well-contoured cavity, with no evidence of internal vasculature (Black arrow).
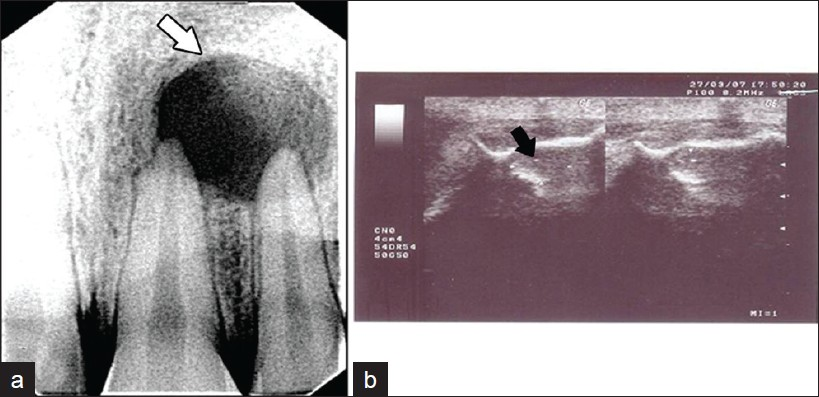
- Various RVG images (a) Pseudo color RVG image shows obturation
in the apical third of the root canal and resorption of the root apex. (b) 3D RVG
image of a periapical lesion and root canal obturation. (c) Normal RVG image
of a periapical lesion and root canal obturation.
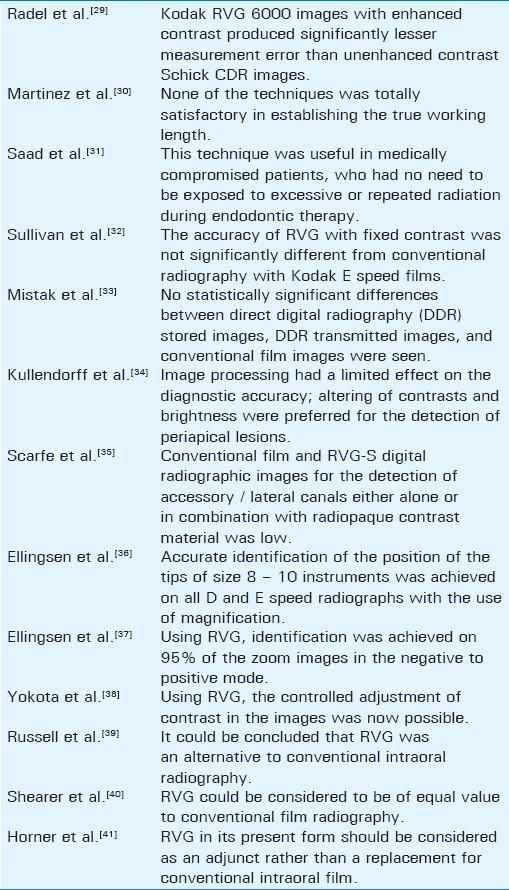
Radio visiography
One of the direct digital radiographic techniques used in dentistry is radio visiography (RVG). This system is based on digital image capture with a charged coupled device (CCD) capable of image enhancement using up to 256 shades of gray. RVG was first commercially used in the United Kingdom in 1989; since then it has undergone several changes.[25]
Radio visiography comprises of four basic components, an x0 -ray unit, an electronic timer, an intraoral sensor, a display processing unit (DPU), and a printer.
Applications of radio visiography in endodontics
Radio visiography is used for diagnosing carious lesions, measuring root lengths, and in detecting periapical pathology and root fractures.[26]
Features of radio visiography
Image enhancement: The gray window effect, known as the x function, allows the operator to select and expand on a specific 60 levels of gray from the 256 available, which may aid in the diagnosis of accessory root canals.[27] The millimeter grid incorporated in the system helps in measuring the length of the root canal. The use of pseudo color assigns different colors to certain gray levels, which can help to visualize particular features that are unclear on images [Figures 2a–c]
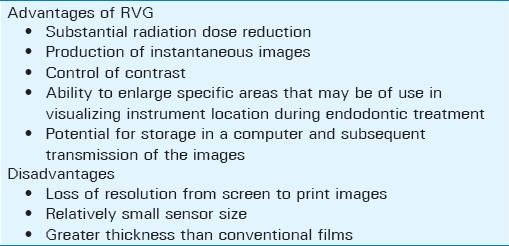
RVG requires 23% of the radiation dose when compared to the conventional radiograph.[28] Resolution of RVG is nine line pairs/mm, which is inferior to conventional X-ray films, but it is adequate for most diagnostic tasks. Advantages and disadvantages of RVG are summarized in Table 3. Results of selected RVG studies are summarized in Table 4.
Computed tomography
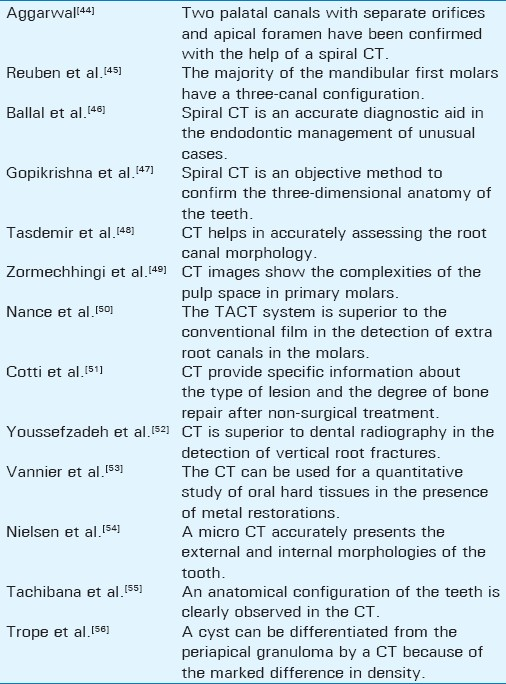
Computed tomography ( CT) produces 3D images of an object by using a series of 2D image data, to mathematically reconstruct a cross-section of the object. It is unique in that it provides images of a combination of soft tissues, bone, and blood vessels.[42] The technique of Dental CT also known as Dentascan was developed by Schwartz et al,[43] The Dental CT can be performed with a conventional CT, a spiral CT, or a multislice CT scanner.
Application of computed tomography in endodontics
Identification of anatomical structures
The alveolar process is the portion of the mandibular bone and maxillary bone that holds the roots of the teeth, the periodontal ligament, the periapical tissues, and the lamina dura. It is, therefore, the area of major interest in the field of endodontics, as most pathological changes, which involve the condition of the roots of the teeth, the possible presence of foreign bodies, and the osteolytic or condensing inflammatory reactions in the bone, occur in this area. The alveolar process is easily visualized and the periodontal space can be imaged, especially if there are pathological conditions.
The extension of the maxillary sinus and the floor of the nose and their relationship with the roots of the teeth are of great importance in the study of the origin and dimension of endodontic lesions. The dental CT offers excellent visualization of maxillary sinus and adjacent teeth.
Chronic apical periodontitis
Chronic apical periodontitis can be seen with the CT scan, both in the early and established stages. It is seen as an enlargement of the periodontal space, which is seen as a small osteolytic reaction around the root tips. Further expansion of the pathological reaction in the cancellous and cortical bone may easily be seen both on the axial scans and on the reconstructed images, including a detailed visualization of the involvement or erosion of the cortical plates.
Vertical root fracture
CT scan is excellent in detecting vertical root fractures or split teeth as periapical radiograph can rarely detect them. CT can also be used to localize foreign bodies in the jaws.
Diagnosis of multiple extra root canals
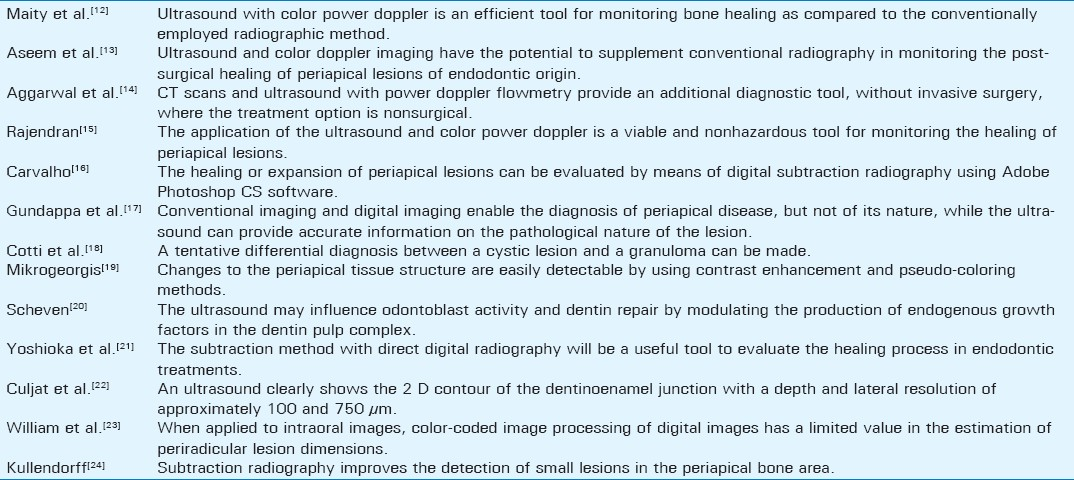
Extra root canals are common phenomena and missing these canals in the routine treatment can lead to endodontic treatment failure. X-rays do not give a 3D view of the anatomy. As root canals tend to lie behind each other in the buccolingual plane, they get superimposed onto each other on the periapical panoramic radiographs and easily go undetected. The software used along with the spiral / helical CT allows assessment in all three dimensions. It provides axial, panoramic, paraxial, and 3D volume rendering, which helps in diagnostic purposes [Figure 3]. Results of selected Computed tomography studies are summarized in Table 5.

- CT image shows root canal obturation and extrusion of the root canal sealer in the periapical area of the maxillary central incisor (Black arrows).
Cone beam computed tomography or cone beam volumetric tomography
Digital radiography offers the benefit of less radiation exposure, faster image acquisition, no chemical usage, and a number of image enhancement tools, such as, increasing magnification. Conventional radiography has numerous disadvantages: Inability to manipulate images, higher radiation dosage required, inability to archive images, and increased time between exposure and image interpretation.[57]
Cone-beam volumetric tomography (CBVT) or cone-beam computed tomography (CBCT) has been specifically designed to produce undistorted three-dimensional information of the maxillofacial skeleton as well as three-dimensional images of the teeth and their surrounding tissues. This is usually achieved with a substantially lower radiation dose that is very effective, compared to conventional computed tomography (CT).[58]
Cone-beam computed tomography (CBCT) uses a cone-shaped beam instead of the fan-shaped one used by the regular CT scanners.[59] Simon et al., reported that CBCT might provide more accurate diagnostic information than a biopsy and histology, when evaluating large periapical lesions.[60]
Applications of cone beam computed tomography in the management of endodontic problems
Endodontic applications of CBCT are less known and not as thoroughly studied.
Specific endodontic applications of CBCT are being identified as the technology becomes more prevalent. Potential endodontic applications include diagnosis of endodontic pathosis and canal morphology, assessment of pathosis of the non-endodontic origin, evaluation of root fractures and trauma, analysis of external, internal root resorption, and invasive cervical resorption, and pre-surgical planning.[61]
Periapical disease may be detected early using CBCT compared to the periapical views, and the true size, extent, nature, and position of periapical and resorptive lesions can be assessed. Root fractures, root canal anatomy, and the true nature of the alveolar bone topography around the teeth may be assessed. The CBCT scans are desirable to assess posterior teeth prior to periapical surgery, as the thickness of the cortical and cancellous bone can be accurately determined, as can the inclination of roots in relation to the surrounding jaw. The relationship of anatomical structures such as the maxillary sinus and inferior dental nerve to the root apices may also be clearly visualized.[58]
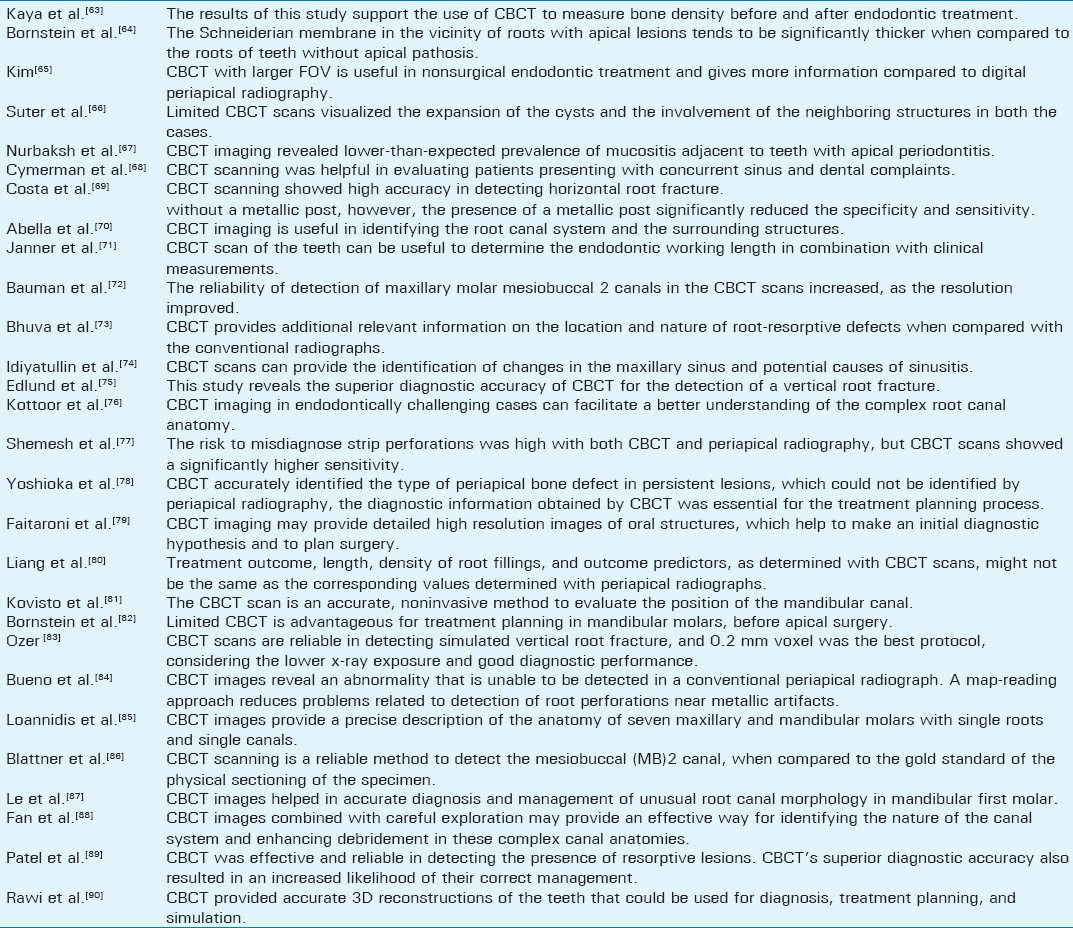
Uses of CBCT are summarized in Table 6.
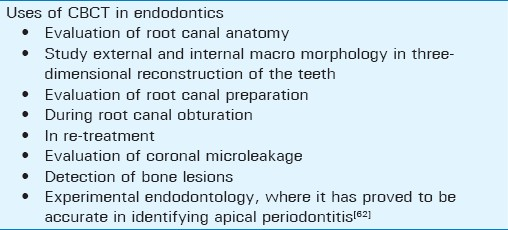
Cone beam computed tomography can determine the difference in density between the cystic cavity content and the granulomatous tissue, and is preferred as a choice for noninvasive diagnosis.[62]
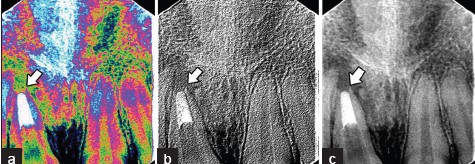
Cone beam computed tomography allows each root and its surrounding structures to be evaluated. Regions of interest can be compared over time. The pre-surgical application of CBCT is an asset in locating lesions, mandibular canals, and the maxillary antrum [Figure 4].[61]

- Cone beam CT image shows a sagittal view of impacted maxillary canine with severe dilaceration (arrow)
Advantages
The advantages include increased accuracy, higher resolution, scan time reduction, and lower radiation dose. Elimination of anatomic noise, facilitates the assessment of a number of important features on endodontic diagnosis, treatment, and long-term management.[61]
Disadvantages
With regard to CBCT images, the presence of an intracanal metallic post might lead to equivocated interpretations as a result of artifact formation. When metallic objects are present in either the tooth of interest or an adjacent one, artifacts can pose difficulties in the analysis of images. In these cases, periapical radiographs are helpful to complement the diagnosis. Distortion of metallic structures due to differential absorption is known as a cupping artifact.[62]
Although CBCT technology is efficient in imaging hard tissue, it is not very reliable in the imaging of soft tissue, as a result of the lack of dynamic range of the x0 -ray detector.
Availability of Cone beam computed tomography is limited to major metropolitan areas at present. Limitations also include medico-legal issues pertaining to the acquisition and interpretation of CBCT data. Various dental applications of CBCT (e.g., oral and maxillofacial surgery) require a large field of view (FOV) to capture all maxillofacial structures within the volume. There is a growing concern among oral and maxillofacial radiologists that dentists without proper training should not perform or interpret CBCT images. Results of selected CBCTs studies are summarized in Table 7.
CONCLUSION
Imaging technology aids in the diagnosis of endodontic pathosis and canal morphology, assessing root and alveolar fractures, in the analysis of resorptive lesions, identification of the pathosis of non-endodontic origin, and pre-surgical assessment before root-end surgery. When compared with CT, CBCT has increased accuracy, higher resolution, reduced scan time, a reduction in radiation dose, and reduced cost for the patient. As compared with conventional periapical radiography, CBCT eliminates the superimposition of the surrounding structures, providing additional, clinically relevant information. The drawbacks of CBCT include limited availability, significant capital investment, and medico-legal considerations. As the CBCT technology evolves, clinicians will be able to adopt 3-D imaging into their diagnostic repertoire. As accurate diagnostic information leads to better clinical outcomes, CBCT might prove to be an invaluable tool in the modern dental practice.[90]
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/13/94227
REFERENCES
- Endodontic success-who's reading the radiograph? Oral Surg Oral Med Oral Pathol. 1972;33:432-7.
- [Google Scholar]
- Radiographic manifestations of periapical inflammatory lesions. Endod Topics. 2004;8:55-67.
- [Google Scholar]
- Reliability of radiographic interpretations. Oral Surg Oral Med Oral Pathol. 1974;38:287-93.
- [Google Scholar]
- A new technique for the study of periapical bone lesions: Ultra sound real time imaging. IntEndod J. 2002;35:148-52.
- [Google Scholar]
- Essentials of Dental radiography and radiology. Netherlands:Elsevier Health Sciences; 2007
- [Google Scholar]
- Ultrasound in dentistry: A review. Journal of Indian Academy of Dental Specialists. 2010;1:44-5.
- [Google Scholar]
- Ultrasound real time imaging in the differential diagnosis of peripaical lesions. IntEndod J. 2003;36:556-63.
- [Google Scholar]
- Advanced radiographic techniques for the detection of lesions in bone. Endod Topics. 2004;7:52-72.
- [Google Scholar]
- Ultrasonic observation of facial bone fractures: Report of cases. J Oral MaxillofacSurg. 1996;54:776-9.
- [Google Scholar]
- Monitoring of healing by ultrasound with color power doppler after root canal treatment of maxillary anterior teeth with periapical lesions. J Conserv Dent. 2011;14:252-7.
- [Google Scholar]
- Use of ultrasound, colordoppler imaging and radiography to monitor periapical healing after endodontic surgery. J Oral Sci. 2010;52:411-6.
- [Google Scholar]
- The Evaluation of computed tomography scans and ultrasounds in the differential diagnosis of periapical lesion. J Endod. 2008;34:1312-5.
- [Google Scholar]
- Efficacy of ultrasound and color power doppler as a monitoring tool in the healing of endodontic periapical lesions. J Endod. 2007;33:181-6.
- [Google Scholar]
- Evaluation of chronic periapical lesions by digital subtraction radiography by using Adobe Photoshop CS: A technical report. J Endod. 2007;33:493-7.
- [Google Scholar]
- Comparison of ultrasound, digital and conventional radiography in differentiating periapical lesions. DentomaxillofacRadiol. 2006;35:326-33.
- [Google Scholar]
- Echographic evaluation of bone lesions of endodontic origin: Report of two cases in the same patient. . 2006;32:901-5.
- [Google Scholar]
- Digital radiograph registration and subtraction: A useful tool for the evaluation of the progress of chronic apical periodontitis. J Endod. 2004;30:513-6.
- [Google Scholar]
- VEGF and odontoblast like cells: Stimulation by low frequency ultrasound. Arch Oral Biol. 2009;54:185-91.
- [Google Scholar]
- An observation of the healing process of periapical lesions by digital subtraction radiography. J Endod. 2002;28:589-91.
- [Google Scholar]
- In vivo accuracy and reliability of color-coded image enhancements for the assessment of periradicular lesion dimensions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:603-11.
- [Google Scholar]
- Subtraction radiography for the diagnosis of periapical bone lesions. Dent Traumatol. 1988;4:253-9.
- [Google Scholar]
- Better imaging: The advantages of digital radiography. J Am Dent Assoc. 2008;139(Suppl):7S-13S.
- [Google Scholar]
- Comparision of radio visiography with radiographic film in root length determination. IntEndod J. 1995;28:25-9.
- [Google Scholar]
- Invitro radiographic determination of distances from working length files to root ends comparing kodak RVG 6000, Schick CDR, and kodak insight film. J Endod. 2006;32:566-8.
- [Google Scholar]
- Methodological considerations in the determination of working length. IntEndod J. 2001;34:371-6.
- [Google Scholar]
- Radiation dose reduction during endodontic therapy: A new technique combining an apex locator (Root ZX) and a digital imaging system (Radiovisiography) J Endod. 2000;26:144-7.
- [Google Scholar]
- Interpretation of periapical lesions comparing conventional, direct digital and telephonically transmitted radiographic images. J Endod. 1998;24:262.
- [Google Scholar]
- Diagnostic accuracy of direct digital dental radiography for detection of periapical bone lesions. Oral Surg Oral Med Oral Patho Oral Radiol Endod. 1996;82:585-9.
- [Google Scholar]
- Radiographic detection of accessory/lateral canals: Use of radio visiography and hypaque. J Endod. 1995;21:185-90.
- [Google Scholar]
- Radiovisiography versus conventional radiography for detection of small instruments in endodontic length determination.Part 1. In vitro evaluation. J Endod. 1995;21:326-31.
- [Google Scholar]
- Radio visiography versus conventional radiography for detection of small instruments in endodontic length determination.In vivo evaluation. J Endod. 1995;21:516-20.
- [Google Scholar]
- Interpretation of periapical lesions using Radio visiography. J Endod. 1994;20:490-4.
- [Google Scholar]
- Radio visiography: A preliminary subjective assessment in a hospital paediatric dentistry department. Int J Paed Dent. 1993;3:77-82.
- [Google Scholar]
- Radio visiography for imaging root canals: An in vitro comparison with conventional radiography. Quint Int. 1990;21:789-94.
- [Google Scholar]
- The role of cone beam computed tomography in the planning and placement of implants. J Am Dent Assoc. 2010;141:19S-24S.
- [Google Scholar]
- Computed tomography.Part I: Preoperative assessment of the mandible for endosseous implant surgery. Int J Oral Maxillofac Implants. 1987;2:134-41.
- [Google Scholar]
- Endodontic management of a maxillary first molar with two palatal canals with the aid of spiral computed tomography: A case report. J Endod. 2009;35:137-9.
- [Google Scholar]
- The evaluation of root canal morphology of the mandibular first molar in an indian population using spiral computed tomography scan: An in vitro study. J Endod. 2008;34:212-5.
- [Google Scholar]
- Endodontic management of a fused mandibular second molar and paramolar with the aid of spiral computed tomography: A case report. J Endod. 2007;33:1247-51.
- [Google Scholar]
- Endodontic management of a maxillary first molar with a single root and a single canal diagnosed with the aid of spiral CT: A case report. J Endod. 2006;32:687-91.
- [Google Scholar]
- Canal preparation with Hero 642 rotary Ni-Ti instruments compared with stainless steel hand K-file assessed using computed tomography. IntEndod J. 2005;38:402-8.
- [Google Scholar]
- A study of root canal morphology of human primary molars using computerised tomography: An in vitro study. J Indian Soc Pedod Prev Dent. 2005;23:7-12.
- [Google Scholar]
- Identification of root canals in molars by tuned-aperture computed tomography. IntEndod J. 2000;33:392-6.
- [Google Scholar]
- Computerized tomography in the management and follow-up of extensive periapical lesion. Dent Traumatol. 1999;15:186-9.
- [Google Scholar]
- Dental vertical root fractures: Value of CT in detection. Radiology. 1999;21:545-9.
- [Google Scholar]
- Three-dimensional dental imaging by spiral CT: A progress report. Oral Surg Oral Med Oral Patho Oral Radiol Endod. 1997;84:561-70.
- [Google Scholar]
- Microcomputed tomography: An advanced system for detailed endodontic research. J Endod. 1995;21:561-8.
- [Google Scholar]
- Applicability of X-ray computerized tomography in endodontics. Dent Traumatol. 1990;6:16-20.
- [Google Scholar]
- Differentiation of radicular cyst and granulomas using computerized tomography. Dent Traumatol. 1989;5:69-72.
- [Google Scholar]
- Cone beam computed tomography-assisted treatment planning concept. Dent Clin N Am. 2011;55:515-36.
- [Google Scholar]
- The potential application of cone beam computed tomography in the management of endodontic problems. IntEndod J. 2007;40:818-30.
- [Google Scholar]
- Use of cone beam computed tomography to identify root canal systems in vitro. J Endod. 2008;34:87-9.
- [Google Scholar]
- Differential diagnosis of large periapical lesions using cone beam computed tomography measurements and biopsy. J Endod. 2006;32:833-7.
- [Google Scholar]
- Accuracy of cone beam computed tomography and panoramic and periapical radiography for detection of apical periodontitis. J Endod. 2008;34:273-9.
- [Google Scholar]
- Measuring bone density in healing periapical lesionsusing cone beam computed tomography: A clinical investigation. J Endod. 2012;38:28-31.
- [Google Scholar]
- Characteristics and dimensions of the schneiderian membrane and apical bone in maxillary molars referred for apical surgery: A comparative radiographic analysis using limited cone beam computed tomography. J Endod. 2012;38:51-7.
- [Google Scholar]
- Endodontic application of Cone beam computed tomography in South Korea. J Endod. 2012;38:153-7.
- [Google Scholar]
- Expansive nasopalatine duct cysts with nasal involvement mimicking apical lesion of endodontic origin: A report of 2 cases. J Endod. 2011;37:1320-6.
- [Google Scholar]
- Resolution of maxillary sinus mucositis after endodontic treatment of maxillary teeth with apical periodontitis: A cone-beam computed tomography pilot study. J Endod. 2011;37:1504-11.
- [Google Scholar]
- Evaluation of odontogenic maxillary sinusitis using cone-beam computed tomography: Three case reports. J Endod. 2011;37:1465-9.
- [Google Scholar]
- Detection of horizontal root fracture with small-volume cone-beam computed tomography in the presence and absence of intracanal metallic post. J Endod. 2011;37:1456-9.
- [Google Scholar]
- Managing severe curvature of radix entomolaris: Three-dimensional analysis with cone beam computed tomography. IntEndod J. 2011;44:876-85.
- [Google Scholar]
- Precision of endodontic working length measurements: A pilot investigation comparing cone-beam computed tomography scanning with standard measurement techniques. J Endod. 2011;37:1046-51.
- [Google Scholar]
- Ex vivo detection of mesiobuccal canals in maxillary molars using CBCT at four different isotropic voxel dimensions. IntEndod J. 2011;44:752-8.
- [Google Scholar]
- The use of limited cone beam computed tomography in the diagnosis and management of a case of perforating internal root resorption. IntEndodJ. 2011;44:777-86.
- [Google Scholar]
- Dental magnetic resonance imaging: Making the invisible visible. J Endod. 2011;37:745-52.
- [Google Scholar]
- Detection of vertical root fractures by using cone-beam computed tomography: A clinical study. J Endod. 2011;37:768-72.
- [Google Scholar]
- Endodontic Management of a maxillary first molar with eight root canal systems evaluated using cone-beam computed tomography scanning: A case report. J Endod. 2011;37:715-9.
- [Google Scholar]
- The use of cone-beam computed tomography and digital periapical radiographs to diagnose root perforations. J Endod. 2011;37:513-6.
- [Google Scholar]
- Periapical bone defects of root filled teeth with persistent lesions evaluated by cone-beam computed tomography. IntEndod J. 2011;44:245-52.
- [Google Scholar]
- Differential diagnosis of apical periodontitis and nasopalatine duct cyst. J Endod. 2011;37:403-10.
- [Google Scholar]
- Endodontic outcome predictors identified with periapical radiographs and cone-beam computed tomography scans. J Endod. 2011;37:326-31.
- [Google Scholar]
- Comparison of periapical radiography and limited cone-beam computed tomography in mandibular molars for analysis of anatomical landmarks before apical surgery. J Endod. 2011;37:151-7.
- [Google Scholar]
- Detection of vertical root fractures by using cone beam computed tomography with variable voxel sizes in an in vitro model. J Endod. 2011;37:75-9.
- [Google Scholar]
- Map-reading strategy to diagnose root perforations near metallic intracanal posts by using cone beam computed tomography. J Endod. 2011;37:75-9.
- [Google Scholar]
- Endodontic management and cone-beam computed tomography evaluation of seven maxillary and mandibular molars with single roots and single canals in a patient. J Endod. 2011;37:103-9.
- [Google Scholar]
- Efficacy of cone-beam computed tomography as a modality to accurately identify the presence of second mesiobuccal canals in maxillary first and second molars: A pilot study. J Endod. 2010;36:867-70.
- [Google Scholar]
- Identification of independent middle mesial canal in mandibular 1st molar using cone beam computed tomography imaging. J Endod. 2010;36:542-5.
- [Google Scholar]
- Negotiation of C-shaped canal systems in mandibular second molars. J Endod. 2009;35:1003-8.
- [Google Scholar]
- The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography - an in vivo investigation. IntEndod J. 2009;42:831-8.
- [Google Scholar]
- Accuracy assessment of three-dimensional surface reconstructions of teeth from cone beam computed tomography scans. J Oral Rehabil. 2010;37:352-8.
- [Google Scholar]






