Translate this page into:
Imaging features and surgical management of giant parathyroid adenoma with autoinfarction

*Corresponding author: Daniel Thomas Ginat, Department of Radiology, University of Chicago, Pritzker School of Medicine, Chicago, United States. dtg1@uchicago.edu
-
Received: ,
Accepted: ,
How to cite this article: Patel T, Wolk R, Cipriani NA, Blair E, Ginat TD. Imaging features and surgical management of giant parathyroid adenoma with autoinfarction. J Clin Imaging Sci. 2024;14:9. doi: 10.25259/JCIS_133_2023
Abstract
Autoinfarction of a parathyroid adenoma can have an atypical clinicoradiologic features that can mimic an inflammatory process or malignancy. In addition, the associated fibrosis makes surgical resection more challenging than for regular parathyroid adenomas. The implications of these findings are that while autoinfarction of parathyroid adenomas is a rare phenomenon, this entity should be considered when there are heterogeneous and cystic components on imaging in patients without hypercalcemia. Ultimately, histopathology is necessary for definitive diagnosis.
Keywords
Imaging
Surgery
Giant parathyroid adenoma
Autoinfarction
INTRODUCTION
Parathyroid adenomas are benign neoplasms associated with hyperparathyroidism, which can lead to hypercalcemia. Patients can present with asymptomatic hypercalcemia that is incidentally discovered or can present with symptoms of hypercalcemia, including bone pain, fatigue, polyuria, nephrolithiasis, constipation, and neuropsychiatric disturbance. More severe cases can cause cardiac arrhythmias, coma, and death.[1] This case demonstrates an unusual acute presentation of parathyroid adenoma secondary to autoinfarction, which leads to the atypical imaging and clinical features. In particular, the associated edema and paucity of internal vascularity potentially mimic an infectious process, such as abscess, or hemorrhagic transformation of a tumor. Typically, parathyroid tumors display hyperenhancement on CT and hypervascularity on ultrasound. In contrast, while giant parathyroid adenomas have a tendency to be cystic,[2] there is limited information regarding the imaging features of parathyroid adenomas with autoinfarction beyond this case.
CASE REPORT
An 82-year-old male presented with the chief complaint of a mass on the left side of his neck and associated complaints of sore throat, weight loss, and dysphagia. The patient had a medical history of hypertension, type 2 diabetes, benign prostatic hyperplasia, gastroesophageal reflux disease, end-stage renal disease managed by hemodialysis, coronary artery disease, and recurrent urinary tract infections caused by Methicillin-resistant Staphylococcus aureus. There were no significant abnormalities in his biochemical and hematological profiles. This article reviews the clinicoradiologic features of giant adenoma with autoinfarction.
Computed tomography (CT) of the neck showed a large heterogeneous mass in the left visceral space adjacent to the thyroid gland, with surrounding edema [Figure 1]. Ultrasound also showed a heterogeneous mass without significant internal vascularity [Figure 2]. CT of the chest was suggestive of lesions of the ribs and left supraclavicular lymphadenopathy. These features created a diagnostic dilemma with differential considerations that might include lymph node metastasis, exophytic thyroid tumor, and parathyroid extracapsular hemorrhage adenoma, or cancer.
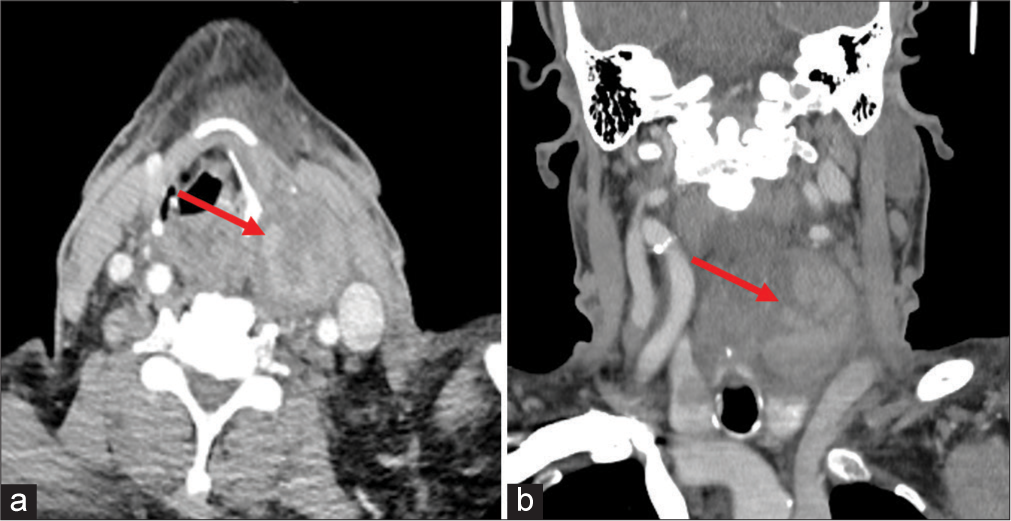
- A 82-year-old male presented with the chief complaint of a mass on the left side of his neck and associated complaints of sore throat, weight loss, and dysphagia. Axial (a) and coronal (b) computed tomography imaged show a large heterogeneous left neck mass adjacent to the thyroid with surrounding edema (red arrows).

- A 82-year-old male presented with the chief complaint of a mass on the left side of his neck and associated complaints of sore throat, weight loss, and dysphagia. Color Doppler ultrasound obtained during biopsy shows absent flow and heterogeneous echogenicity of the encapsulated mass (red arrow).
The patient underwent resection of the mass, along with the left neck dissection. The specimens were sent for histologic examination, which revealed that the central component of the mass was entirely necrotic, but there was a rim of viable cells at the periphery [Figure 3], with associated fibrosis causing adherence to the thyroid lobe. These cells were morphologically and immunophenotypically compatible with the parathyroid chief and clear cells (positive for GATA3 and PTH with focal weak polyclonal PAX8 expression). Parafibromin was retained by immunohistochemical stain. Overall, these features were most compatible with an infarcted parathyroid adenoma. Biopsy of the rib lesion showed bone and marrow with focal hemosiderin deposition and resected left neck lymph nodes were benign.

- A 82-year-old male underwent resection of the left neck mass. Hematoxylin and eosin-stained histopathology image at ×40 magnification shows areas of hypercellular parathyroid glandular tissue (asterisk) adjacent to areas of necrosis and hemorrhage (black arrows).
DISCUSSION
Parathyroid adenomas are benign neoplasms associated with hyperparathyroidism, which can lead to hypercalcemia. Patients can present with asymptomatic hypercalcemia that is incidentally discovered or can present with symptoms of hypercalcemia, including bone pain, fatigue, polyuria, nephrolithiasis, constipation, and neuropsychiatric disturbance. More severe cases can cause cardiac arrhythmias, coma, and death.[1] This case demonstrates an unusual acute presentation of parathyroid adenoma secondary to autoinfarction, which leads to the atypical imaging and clinical features. In particular, the associated edema and paucity of internal vascularity potentially mimic an infectious process, such as abscess, or hemorrhagic transformation of a tumor. Typically, parathyroid tumors display hyperenhancement on CT and hypervascularity on ultrasound. In contrast, while giant parathyroid adenomas have a tendency to be cystic,[2] there is limited information regarding the imaging features of parathyroid adenomas with autoinfarction beyond this case.
The term “atypical parathyroid adenoma” was substituted with “atypical parathyroid tumor” in 2022 under the World Health Organization classification and is considered to be a neoplasm of uncertain malignant potential.[3] Atypical parathyroid tumors include giant adenomas, which are very rare with only 65 cases reported in the literature and account for about 1% of primary hyperparathyroidism.[4,5] Parathyroid adenomas weighing more than 3.5 g or more than 2 cm in diameter are considered giant adenomas.[6] Most parathyroid adenomas are diagnosed after abnormal calcium profiles in patients in developed countries. Although very rare, these adenomas can undergo autoinfarction and may also lead to transient remission of hyperparathyroidism. The normal calcium status of our patient may be explained by either this phenomenon or due to hemodialysis. Autoinfarction of parathyroid adenoma is a very uncommon phenomenon that has been described in only a few cases. This phenomenon could be due to the fragility of the tumor vascularization. Giant adenomas can be particularly vulnerable to necrosis due to the sensitivity of solid components of the mass to compromised vascular supply.[4] This is especially seen around the periphery of the mass. The center of the mass usually undergoes cystic degeneration.[6]
Although there was no calcium imbalance in this patient, surgical intervention was warranted to rule out malignancy and alleviate symptoms related to the mass effect of the tumor. The usage of fine-needle aspiration can pose a risk of seeding in case of malignancy or even simulate the features of malignancy.[7] Hence, thorough intraoperative evaluation as well as a meticulous histological examination of the resected mass are crucial. Resection of the parathyroid tumor with ipsilateral lobectomy of the thyroid and ipsilateral level VI lymphadenectomy is usually the operative plan. However, limited resection can be performed if there is no clear invasion of adjacent tissues.[4] There have been cases when there is a transient remission of hyperparathyroidism and normalization of calcium levels after the autoinfarction of the adenoma. However, surgical intervention is still justified based on previous research that showed recurrent hyperparathyroidism after non-surgical surveillance of an autoinfarcted adenoma.[8,9]
CONCLUSION
This case demonstrates the potential atypical imaging features of giant adenoma with autoinfarction, which can be associated with challenges for surgical management. The characteristic features on histopathology ultimately help establish the diagnosis.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The patient’s consent is not required as the patient’s identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Parathyroid adenoma In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507870 [Last accessed on 2023 Jun 12]
- [Google Scholar]
- Giant cystic parathyroid adenoma: Two case reports and a literature review. J Int Med Res. 2022;50:3000605221106419.
- [CrossRef] [PubMed] [Google Scholar]
- Giant parathyroid tumours in primary hyperparathyroidism: A systematic review. Langenbecks Arch Surg. 2022;407:501-16.
- [CrossRef] [PubMed] [Google Scholar]
- Do giant parathyroid adenomas represent a distinct clinical entity? Surgery. 2013;154:714-8.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical parathyroid adenoma: Clinical and anatomical pathologic features. World J Surg Oncol. 2021;19:19.
- [CrossRef] [PubMed] [Google Scholar]
- Autoinfarction of giant parathyroid adenoma after preoperative withdrawal of anticoagulants. Case Rep Surg. 2018;2018:9261749.
- [CrossRef] [PubMed] [Google Scholar]
- Parathyroid carcinoma. Curr Opin Otolaryngol Head Neck Surg. 2016;24:155-62.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous short-term remission of primary hyperparathyroidism from infarction of a parathyroid adenoma. J Endocrinol Invest. 2004;27:687-90.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrence of primary hyperparathyroidism following spontaneous remission with intracapsular hemorrhage of a parathyroid adenoma. J Bone Miner Metab. 2008;26:295-7.
- [CrossRef] [PubMed] [Google Scholar]






