Translate this page into:
Herniation of Packing Material into a Bronchopleural Fistula after Right Pneumonectomy and Clagett Window
Address for correspondence: Dr. Iclal Ocak, University of Pittsburgh Medical Center, Radiology Suite 200 East Wing, 200 Lothrop Street, Pittsburgh, PA 15213, USA. E-mail: ocaki@upmc.edu
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Diagnosis of a bronchopleural fistula (BPF) can be challenging in patients after pneumonectomy and Clagett window. Herein, we present a case of pneumonectomy for advanced lung cancer complicated by a BPF. Herniation of packing material from the open-chest cavity into the fistula and airways on computed tomography was an important clue to making the diagnosis.
Keywords
Bronchopleural fistula
clagett
pneumonectomy

INTRODUCTION
A bronchopleural fistula (BPF) is a direct communication between the bronchial stump and the pleural space by an opening in the bronchial stump following lobectomy or pneumonectomy. BPFs typically occur due to dehiscence and necrosis of the bronchial stump and manifest as a persistent air leak.[1] BPFs may be an early complication of lobectomy or pneumonectomy and vary in size. A large BPF is a dreaded surgical complication, often with life-threatening consequences. The reported prevalence of large BPFs is 1%–4%, with an associated mortality rate of 16%–23%.[23] Traditional surgical treatment is stump closure with chest wall muscle or omental flap transposition.[4]
In this case report, we present a patient with locally advanced squamous cell carcinoma (SCCA) of the lung who ultimately underwent pneumonectomy and Clagett window complicated by delayed development of a BPF. Herniation of packing material into the fistula was an important imaging clue to the diagnosis of a BPF.
CASE REPORT
A 71-year-old man was diagnosed with locally advanced right upper lobe (RUL) T3N1M0, stage IIIA, SCCA in 2014 [Figure 1], which occluded the origin of the RUL bronchus and extended into the right mainstem bronchus. He underwent neoadjuvant chemotherapy with carboplatin and taxol as well as radiation therapy (46 Gy). Three months after completion of therapy, he underwent right thoracotomy and right bronchial sleeve upper lobectomy with complete surgical resection of the residual tumor. An omental flap was harvested and applied to the anastomosis of the bronchus intermedius and right mainstem bronchus. Two months later, he developed an episode of large-volume hemoptysis at an outside hospital and was transferred to our facility. Following a 2nd episode of massive hemoptysis, he was taken into the operating room for emergency thoracotomy. Computed tomography (CT) of the chest was not performed at that time. Surgical exploration revealed a right hilar abscess with necrosis and dehiscence of the right main bronchial anastomosis and omental flap, as well as erosion into the pulmonary artery resulting in a bronchoarterial fistula. Completion pneumonectomy was then performed. The bronchial stump was closed with a right pectoralis muscle flap which was placed over the stump through the 3rd intercostal space. A Clagett window was constructed anteriorly with resection of the 5th through 8th ribs to facilitate treatment and drainage of the infection [Figure 2].
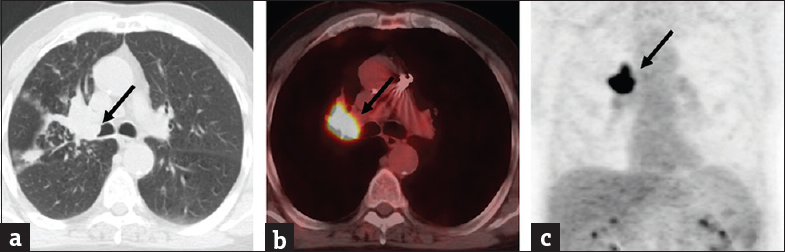
- A 71-year-old man with right upper lobe T3N1M0 squamous cell carcinoma. (a) Axial computed tomography images in lung and soft-tissue windows showing an obstructive right hilar mass lesion with an endobronchial component at the origin of the right upper lobe bronchus (arrow). (b and c) Axial and coronal positron emission tomography/computed tomography images showing avid F-18 fluorodeoxyglucose uptake with the mass (arrow).
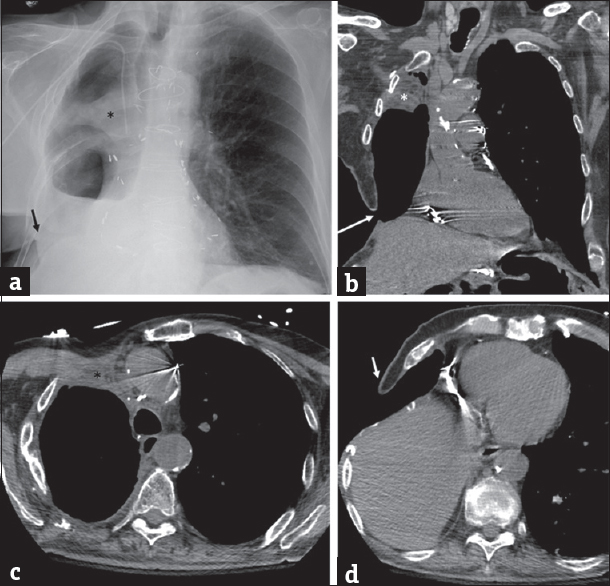
- (a and b) Chest X-ray and coronal computed tomography reformation demonstrating the right pectoralis muscle flap (*) and Clagett window (arrow). (c and d) Axial computed tomography images again showing the right pectoralis muscle flap (*) and Clagett window.
Six months later, on a routine clinical visit, the patient was noted to be short of breath, tachycardic, and febrile. He was sent to the emergency department for further evaluation and a chest CT revealed herniation of dressing material through a fistula into the trachea and left mainstem bronchus [Figures 3 and 4]. Bronchoscopy revealed a small BPF due to breakdown of the bronchial stump. Packing material within the airway was removed at that time without complication. Surgical management was deferred and the patient was prescribed antibiotics with frequent dressing changes of the Clagett window. He was eventually discharged home in June 2015 and his BPF closed by secondary intention without further complication.
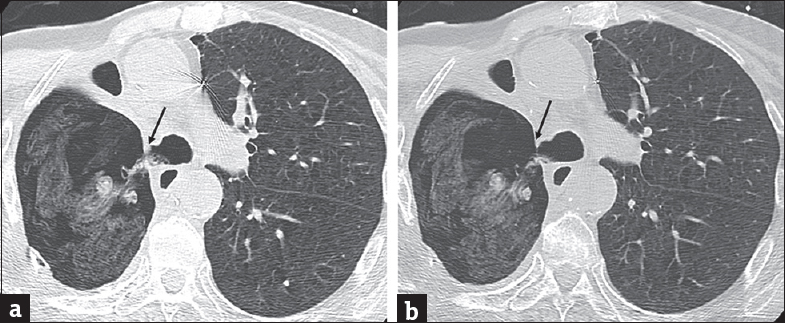
- Bronchopleural fistula in a 71-year-old man after right pneumonectomy and Clagett window. (a and b) Axial computed tomography images in lung window demonstrating a fistula between the bronchial stump and pneumonectomy space with herniation of dressing material from the right pneumonectomy space through a fistula into the trachea and left mainstem bronchus (arrow).
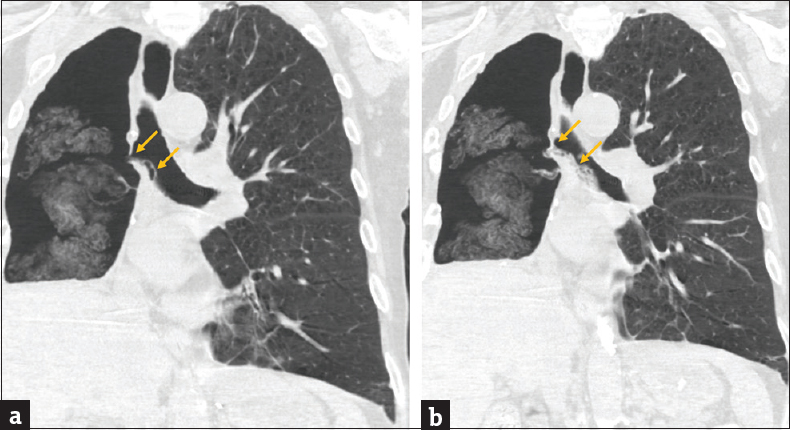
- (a and b) Coronal computed tomography images showing a bronchopleural fistula and herniation of dressing material thorough the defect into the carina and left mainstem bronchus (arrows) from the right pneumonectomy space.
DISCUSSION
BPFs are a rare but serious complication after pneumonectomy. Following pneumonectomy, immediate postoperative chest radiographs typically reveal that the trachea is midline and the pneumonectomy space is filled with air. Within 24 h, the ipsilateral hemidiaphragm becomes slightly elevated, the mediastinum shifts slightly toward the pneumonectomy space, and fluid starts accumulating at a rate of one to two intercostal spaces per day. After 2 weeks, 90% of the pneumonectomy space is filled with fluid. In the case of a BPF, the chest radiographs demonstrate new or progressive pneumothorax despite adequate tube drainage, increase in subcutaneous or mediastinal emphysema, and a decrease in the air–fluid level with a contralateral shift of the heart and mediastinum.[3]
Early BPFs typically occur within 7 days after pneumonectomy due to difficult technical closure, incomplete closure, devascularization by extensive mediastinal dissection, and/or prior radiation. Late BPFs occur more than 1 week after the operation due to failure of bronchial stump healing, recurrence of cancer at the bronchial margin, or infection.[5] BPFs are therefore more common following right pneumonectomy, mediastinal lymph node dissection, high-dose radiotherapy, prolonged mechanical ventilation, empyema, and/or residual or recurrent carcinoma at the bronchial stump.[4]
In our case, the BPF was observed 6 months after pneumonectomy due to failed healing of the bronchial stump, likely in part due to a combination of risk factors such as a right pneumonectomy, mediastinal lymph node dissection, prior chemoradiation, infection, and prolonged ventilation. Due to air and packing material in the pneumonectomy space and absence of pleural fluid, the only CT finding of a BPF was a subtle defect in the right mainstem bronchus stump with herniated dressing material through the stump into the trachea and left mainstem bronchus. Careful manipulation of the window settings helped to differentiate herniated dressing material from aspirated mucus and debris within the airway. Otherwise, the fistula tract and dehiscence of the bronchial stump could have been easily missed.
CONCLUSION
In our case, a small BPF developed 6 months after completion pneumonectomy and Clagett window, diagnosed by herniation of the packing material into the defect, trachea, and left mainstem bronchus. The BPF ultimately healed by secondary intention. To the best of our knowledge, this is the first case report of a diagnosis of BPF after pneumonectomy and Clagett window, made by identifying herniated packing material into the airways. It is important to know the surgical techniques and potential complications involved in a pneumonectomy or Clagett window procedure for timely diagnosis and management of important complications such as BPFs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/17/230279
REFERENCES
- Lung cancer: Posttherapy imaging and complications. J Thoracic Imaging. 2017;32:276-87.
- [Google Scholar]
- Bronchial closure methods and risks for bronchopleural fistula in pulmonary resections: How a surgeon may choose the optimum method? Interact Cardiovasc Thorac Surg. 2011;12:558-62.
- [Google Scholar]
- Radiographic and CT findings of thoracic complications after pneumonectomy. Radiographics. 2006;26:1449-68.
- [Google Scholar]
- Bronchopleural fistula after pneumonectomy: Interdisciplinary surgical closure by an ipsilateral pedicled latissimus dorsi flap supported by video-assisted thoracoscopy. J Plast Reconstr Aesthet Surg. 2013;66:1600-3.
- [Google Scholar]
- Focus on treatment complications and optimal management surgery. Transl Lung Cancer Res. 2014;3:181-6.
- [Google Scholar]






