Translate this page into:
Focal Lipoatrophy of Face: A Rare Esthetic Complaint
Address for correspondence: Dr. K. Anbarasi, Division of Oral Medicine and Radiology, Faculty of Dental Sciences, Sri Ramachandra University, Porur, Chennai - 600 116, India. anbarasi815@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A well-proportioned face combines features that are balanced and symmetrical. Any structural alteration that leads to facial asymmetry causes esthetical and psychological disturbances. Lipoatrophy is one such condition, which results in loss of subcutaneous fat layer and manifests as a depression. Although many subtypes with varying clinical and etiological backgrounds exist, the idiopathic form is rare and facial involvement is the rarest. Computed tomography is one of the accepted diagnostic tools to determine the atrophic layer of facial anatomy. This report presents the clinical types, diagnosis, and management of a case of facial lipoatrophy.
Keywords
Computed tomography
lipodystrophy
lipoatrophy
ultrasound
autologous
INTRODUCTION

Lipodystrophy broadly refers to a disturbance in the production, utilization, and storage of fat. These changes are specifically subdivided into lipoatrophy and hyperadiposity. Lipoatrophy is a sharply defined disappearance of the subcutaneous fat, without exudative reactions or appreciable fibrosis (Marble and Smith 1942). Lipoatrophy is divided into Generalized, Partial (extensive, but not generalized), and Localized (limited to a localized area) types.[1] There is no universal or precise proven reason for lipoatrophy; however, literature suggests impairment of adipocyte differentiation, adipocyte apoptosis, and mitochondrial dysfunction, as the heterogeneous pathogenesis, reflecting the different subtypes.[2]
Generalized lipoatrophy is a rare disorder characterized by a near complete absence of fat. Both congenital and acquired forms are reported. The congenital type is a genetic disturbance, presenting with a generalized absence of fat within the first year of life and is followed by a series of abnormalities like insulin resistance and acanthosis nigricans before adolescence. The acquired form is autoimmune in nature. The onset is during childhood, with widespread panniculitis, and a strange physical stature.
Partial lipoatrophy was first reported in1885 by Mitchell.[3] It has a characteristic beginning of progressive subcutaneous fat loss in the face and scalp, and then spreads up to the iliac crests. Children between five and eight years are the target group, with girls outnumbering boys by 4:1.
Iatrogenic causes of lipoatrophy include complications of injected medications like insulin, corticosteroids, antibiotics (Penicillin G), iron, heparin, and vaccines.[4] HIV-positive patients on anti-retroviral therapy, especially, nucleoside reverse transcriptase inhibitors (NRTs)[2] and protease inhibitors (PI) [5] manifest lipoatrophy as an adverse drug effect.
CASE REPORT
A 28-year-old female patient reported to our institution with a complaint of a depression appearing on the right lower facial region. It had started as a small depression two years earlier, with no accompanying pain or discomfort, which progressed to the present state of asymmetry and abnormal appearance. Her medical records showed no history of facial trauma or dental infections. On examination, the facial asymmetry was found to be due to deficiency of the fat layer in the right parasymphyseal region, extending inferiorly to the lower border of the mandible [Figure 1a]. The regional skin was extremely thin with pigmentary changes [Figure 1b]. The intraoral examination revealed healthy oral mucosa and a complete set of dentition. Localized idiopathic subcutaneous atrophy of the face was considered as a clinical diagnosis and the relevant diagnostic workup was started.

- A 28-year-old female patient with facial asymmetry and sunken right cheek.

- Right profile view of the patient shows the atrophic region with pigmentation.
An en-face photograph and profile views of the patient were taken and analyzed together, to assess the degree of asymmetry [Figures 1a and b].
Ultrasonography using, 7-10 MHZ frequency linear probe (Volvuson 730 pro expert GE machine) revealed the normal superficial skin layer bilaterally. The thickness of subcutaneous plane was 0.22 cm on the right side and 0.28 cm on the left side. Altered echogenicity was noted on the right masseter muscle. On the affected side, the muscle thickness was 0.83 cm, whereas, on the normal side, it was 1.26 cm [Figures 1c and d]
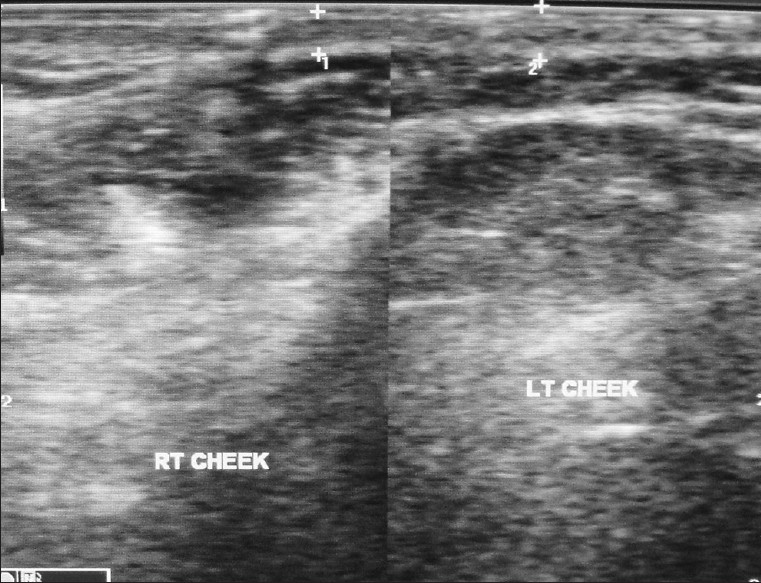
- Ultrasound image reveals normal facial anatomy on the left side and altered echogenicity on the right cheek at the subcutaneous and massetric layer.
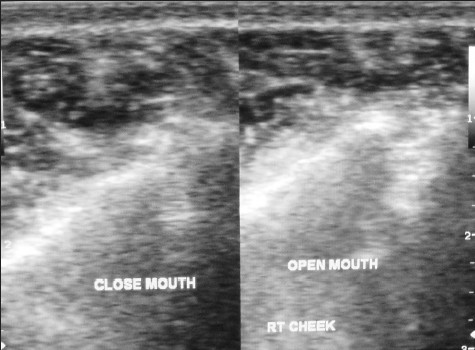
- Ultrasound image of the affected side, allows measurement of muscle thickness in both open and closed mouth positions.
The serial axial and coronal CT sections of the craniofacial bones obtained with multiplanar and volume-rendered reconstructions confirmed the asymmetry of the subcutaneous soft tissues, which were atrophied on the right cheek region. The underlying muscles and bones appeared normal [Figures 1e and f]

- Coronal CT shows subcutaneous atrophy of fat on the right side.

- Axial CT demonstrates subcutaneous atrophy at the level of the right mandible.

- Patient's face after soft tissue reconstruction.

- Patient's right profile after soft tissue reconstruction.
The patient was advised biopsy, but she refused. Clinical investigations showed normal values for complete blood count, blood glucose, serum cholesterol, and triglycerides. Plasma C3 and C4 levels were within normal limit. The Antinuclear Antibody (ANA) test was negative.
Based on the clinical and imaging, we concluded the final diagnosis as localized, idiopathic involutional grade 1 lipoatrophy of the face. The patient was treated in the Plastic and Reconstructive Surgery Department. Autologous fat harvested from the abdomen was injected to the subcutaneous plane to rebuild the sunken area [Figures 1g and h]
DISCUSSION
Facial esthetics depends on the balance between the mobility and stability of facial anatomy. The subcutaneous fat provides volume and mobility, and is supported by fibrous retinacular cutis, which connects the dermis to the muscle apponeurotic system. The subcutaneous layer is critical, because, wasting of subcutaneous fat results in atrophy, whereas, its increased thickness leads to lengthening of the retinacular fibers, therefore, weakness and distention. Paucity or complete absence of fat in the confined subdermal layer, with lack of inflammatory signs, is known as idiopathic localized involutional lipoatrophy (ILIL).[6] Peters and Winkelmann first reported this condition, as a sharply demarcated skin depression without any epidermal alteration.[7] The features of facial lipoatrophy include sunken cheeks, deep folds in the nasolabial region, skin depression at the temples, sides of forehead, and around the eye sockets. Spontaneous regression in few weeks is usual, however, in some cases the lesion may persist and cause cosmetic concerns.
The facial lipoatrophy can be graded as follows.[8]
Grade 0 — No facial lipoatrophy.
Grade 1 — Mild flattening or shadowing on one or more facial regions; No prominent bony land marks and no visibility of the underlying musculature.
Grade 2 — Intermediate point between Grade 1 and Grade 3.
Grade 3 — Moderate concavity of one or more facial regions, prominence of bony land marks, and possible visibility of the underlying musculature.
Grade 4 — Intermediate point between Grade 3 and Grade 5.
Grade 5 — Severe depression of one or more facial regions, severe prominence of bony land marks, and clear visibility of the underlying musculature.
Computed tomography (CT) plays an useful role in the diagnosis of focal lipoatrophy as fat can be easily appreciated on CT.[9] US can demonstrate asymmetry of the face and loss of fat in focal lipoatrophy but it has less sensitivity than CT.
To improve esthetics, common treatment modalities, with evidence of safety and efficacy are, using permanent and non-permanent types of fillers. The possibility of severe infection, contour abnormalities, and facial nerve and muscle damage, restrict the use of permanent type of fillers like silicone oil. Non-permanent fillers, being biodegradable, can diminish over time and may necessitate a revamp, but they do not cause foreign body reactions or granulomas. Injection of a biodegradable and bioabsorbable poly-L-lactic acid (PLA) filler causes cutaneous thickening by fibrous connective tissue formation over a month. The call for multiple treatment sessions, cost, and transitory relief, limit its use for augmentation. Autologous fat transfer (AFT) is a secure and cost-effective option, exclusively for non-HIV patients with lipoatrophy.[10] In our patient, as the abnormality was a mild cosmetic disorder, with no disability, needle extraction of adipose tissue from the abdomen and injecting this at the site of the atrophy was done with the aim of ensuring rapid revascularization and less resorption. A soft, slightly curved, and well-defined anatomy with esthetic satisfaction was achieved. Frequent patient follow-up is essential to monitor the acceptance and consequences, and to see if there is a need for repeating the treatment.
CONCLUSION
Facial lipoatrophy in otherwise healthy individuals is uncommon and patients usually present for cosmetic reasons. CT imaging is useful in the diagnosis and biopsy is confirmatory. This is a benign condition that can be easily corrected with surgery. The current case report highlights its diagnosis and management.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/14/94229
REFERENCES
- Discovery of a lipoatrophy gene.One answer, one hundred questions. Eur J Endocrinol. 2000;143:565-7.
- [Google Scholar]
- Adipose tissue biology and HIV- infection. Best Pract Res Clin Endocrinol Metab. 2011;25:487-99.
- [Google Scholar]
- Singular case of absence of adipose matter in the upper half of the body. Am J Med Sci. 1885;90:105-6.
- [Google Scholar]
- Insulin - induced lipoatrophy in type I diabetes: A possible tumor necrosis factor- α mediated differentiation of adipocytes. Diabetes Care. 1996;19:1283-5.
- [Google Scholar]
- Subcutaneous adipocyte apoptosis in HIV - 1 Protease inhibitor associated Lipodystrophy. AIDS. 1999;13:2261-7.
- [Google Scholar]
- Localized involutional lipoatrophy: Report of six cases. J Dermatol. 2002;29:638-43.
- [Google Scholar]
- Localized lipoatrophy (atrophic connective tissue disease panniculitis) Arch Dermatol. 1980;116:1363-8.
- [Google Scholar]
- Full scope of effect of facial lipoatrophy: A framework of disease understanding. Dermatol Surg. 2006;32:1058-69.
- [Google Scholar]
- New and emerging agents in the management of lipodystrophy in HIV-infected patients. HIV/AIDS. 2010;2:167-78.
- [Google Scholar]
- A case of fat injection for treating subcutaneous atrophy caused by local administration of corticosteroid. Tokai J Exp Clin Med. 2010;35:66-9.
- [Google Scholar]






