Translate this page into:
Fluorine-18-fluorodihydroxyphenylalanine Positron-emission Tomography Scans of Neuroendocrine Tumors (Carcinoids and Pheochromocytomas)
Address for correspondence: Dr. Italo Zanzi, 27 Aerie Court, Manhasset, NY 11030, USA. E-mail: izanzi@northwell.edu
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives:
Conventional methods of imaging neuroendocrine tumors with computed tomography, magnetic resonance imaging, indium-111-octreotide, or radiolabeled metaiodobenzilguanidine scintigraphy have limitations. This pilot study tried to improve the localization of these tumors with fluorine-18-fluorodihydroxyphenylalanine (F-DOPA) positron-emission tomography (PET) scanning.
Materials and Methods:
We studied 22 patients, the majority of whom were referred with clinical diagnosis or suspicion of carcinoid (n = 11), neuroendocrine tumors (n = 7) or pheochromocytoma/paraganglioma (PGL) (n = 4). The comparison was made with the prior conventional imaging.
Results:
The F-DOPA findings were compared with the results of subsequent surgery (2), endoscopy (1), or a long-term follow-up (mean duration, 49 months) for 17 patients. Two patients were lost to follow-up. Foci of F-DOPA deposition were detected in eight patients (final diagnosis of carcinoid in six, of neuroendocrine tumors in one, and of PGL in another). Comparison with the final diagnoses revealed concordance in 16 of the 22 patients. F-DOPA results appeared superior to those obtained with conventional imaging. Despite the small number and diagnostic heterogeneity, in a substantial fraction of patients F-DOPA PET added information relevant to clinical management.
Conclusion:
F-DOPA scanning added prognostic value, particularly when multiple abnormal foci versus a negative examination were considered.
Keywords
Carcinoid
fluorodihydroxyphenylalanine positron-emission tomography
neuroendocrine tumor
pheochromocytoma/paraganglioma

Introduction
Carcinoid tumors, one of the most common types of neuroendocrine tumors, frequently manifest with neurosecretory symptoms and biochemical abnormalities, such as secretion of tumor markers.[1] Approximately 10% of all patients with carcinoid exhibit the carcinoid syndrome: facial flushing, episodic diarrhea, bronchoconstriction, and right-side valvular heart disease.[2] These are frequently benign, and resection may result in cure.[34] In approximately 50%–75% metastases are present, most frequently in lymph nodes, liver, and/or bone.[45] Additional treatments, such as somatostatin analogs, interferon-alpha, chemotherapy, and/or peptide-targeted radionuclide therapy, are neuroendocrine tumors used in those with aggressive properties.[6]
Pheochromocytoma (PHEO) is usually a benign unilateral neuroendocrine tumor of the adrenal medulla. However, it may be bilateral, sporadic, or familial, in extra-adrenal sites, malignant and metastatic, or combined with other neuroendocrine tumors.[78] PHEOs are functional tumors that secrete catecholamines which are the source of symptoms, such as palpitations, hypertension, or others. Catecholamine-producing tumors that arise from sympathetic ganglia are termed paragangliomas (PGLs). The main diagnostic tool is laboratory examinations, such as plasma catecholamines levels and 24-h urine vanillylmandelic acid, which have sensitivities in the range of 89%–100%. Tumors left untreated may have a fatal outcome. The treatment of choice is complete surgical resection.
Conventional imaging, such as computed tomography (CT), magnetic resonance (MR) imaging, and usual nuclear medicine techniques are frequently unsuccessful in the localization of neuroendocrine tumors for resection.[9] Following the approval by the Institutional Ethics Committee (Institutional Review Board [IRB]), we performed positron-emission tomography (PET) scans postintravenous (IV) injection of fluorine-18-fluorodihydroxyphenylalanine (F-18-F-DOPA) in 22 patients with suspected neuroendocrine tumors. The aim of this study was to explore the possible clinical value of this imaging modality in patients with equivocal localization of neuroendocrine tumors. The inclusion (and publication) of two initial patients studied under compassionate approval was approved by the IRB. Carbidopa (alpha-methyl-dopa hydrazine), an aromatic-L-amino acid decarboxylase inhibitor, was given before the injection of F-DOPA in some of our patients to decrease the urinary excretion of F-DOPA, decrease image reconstruction artifacts, and possibly increase its uptake in tumors with the aim of improving the detection of neuroendocrine tumors.[1011]
Materials and Methods
Patients
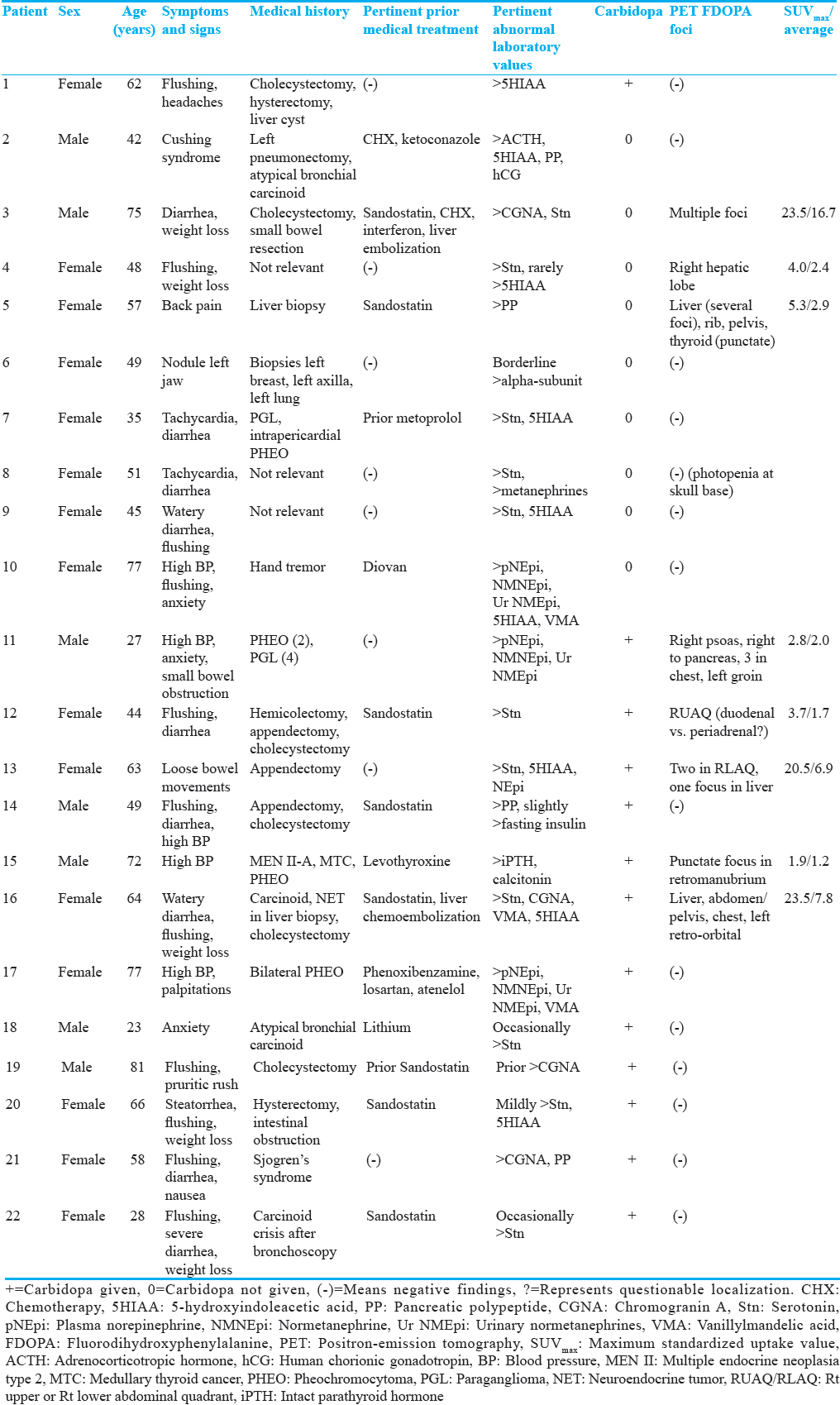
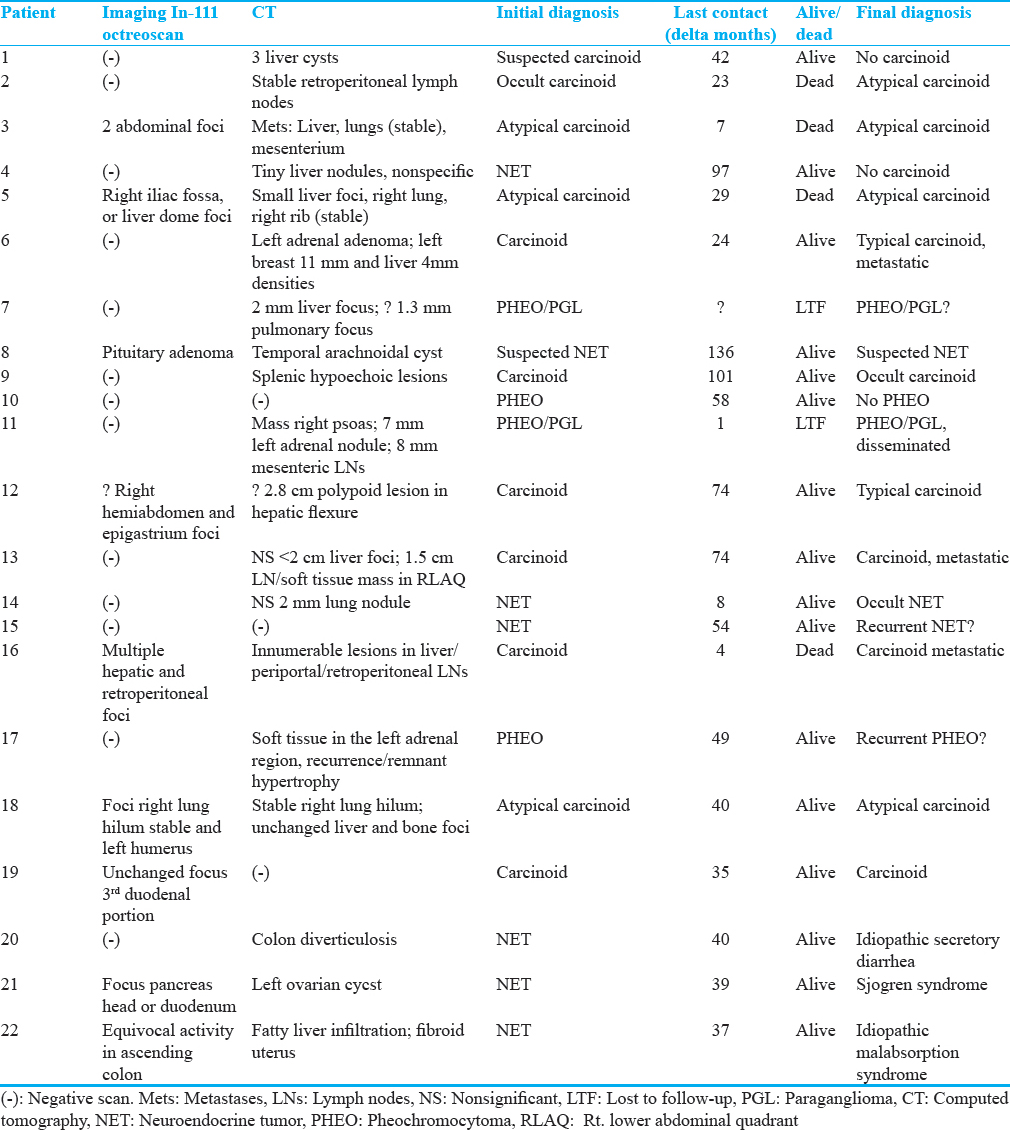
Twenty-two referred patients (15 women and seven men) were studied; mean age, 54 years (median = 57, range = 23–81). Demographics, symptoms, pertinent medical history, treatment, laboratory results, and findings of prior scintigraphy (indium-111-octreotide [In-111-OCT] or iodine-123-metaiodobenzylguanidine [I-123-MIBG]), and CT scans are presented in Tables 1 and 2. Referral diagnoses were carcinoid (n = 11) including three atypical, one occult, and one suspected but unproved; neuroendocrine tumors (n = 7); and PHEO including two PHEO/PGLs (n = 4). Minors and pregnant or lactating women were not included in this study. Prior histories of radiation therapy, recent chemotherapy, or antituberculosis medications, which are monoamine oxidase inhibitors, were cause of exclusion. All patients received complete information regarding the research study and signed the corresponding consent form. The results of the F-DOPA/PET scan were communicated to the referring physicians. Efforts were made to collect information regarding the long-term clinical outcome of the patients.
Materials and methods
F-18-F-DOPA was prepared based on an established procedure[12] which has been modified to improve the yield and quality of the drug product by using a disposable synthesizer to achieve the required sterility and apyrogenicity. In the actual synthesis, F-DOPA was produced by the nucleophilic fluorination of L, 4, 5 dimethoxy-2-trifluoroacetatemercuri-N-trifluoroacetyl-phenylalanine ethyl ester using acetyl hypofluorite. The fluorinated intermediate was hydrolyzed with acetic anhydride and hydroiodic acid (30 min). The hydrolyzed product was extracted with buffer and subjected to HPLC separation using a Phenomenex ODS column (magnum) and 0.1% acetic acid as the eluent. The separated product (peak at 10 min) was passed through a sterile Millipore filter into a sterile vial. The product was subjected to quality control to ensure the purity and the sterility of the product. The quality of the product was validated using three consecutive syntheses according to the Food and Drug Administration (FDA) requirements and has been used for neurological studies under an FDA-approved Expanded Access investigational new drug.
F-DOPA imaging protocol was similar to that used routinely for oncology patients with fluorodeoxyglucose (FDG), obtaining images from the neck to the pelvic/groin region. Patients fasted for a minimum of 4 h before the IV injection of a dose of up to 8.5 mCi. A standard dose of 150 mg of carbidopa (Lodosyn) was administered 60–90 min before the injection of F-DOPA for PET imaging in 13 of the 22 patients studied.
Acquisition of emission tomographic images started 60–90 min after F-DOPA injection, which is similar to the interval used for brain studies.[13] Two-dimensional images were obtained in the GE Advance PET scanner which provides eight-bed positions. A duration of 5 min for transmission and emission views was used to obtain attenuation corrected images which were reconstructed with an iterative procedure. The reconstructed views were assessed by two experienced nuclear medicine physicians on films and computer monitor (GE Entegra) on orthogonal computed sections and in cinematic mode. These scans were interpreted at different times by those physicians, one of them “masked” to prior anatomical and scintigraphic imaging modalities. In discrepancy, the two readers reached a consensus at a combined reading. The criterion for abnormality was any focal deposition of the radiopharmaceutical exceeding normal regional tracer uptake.
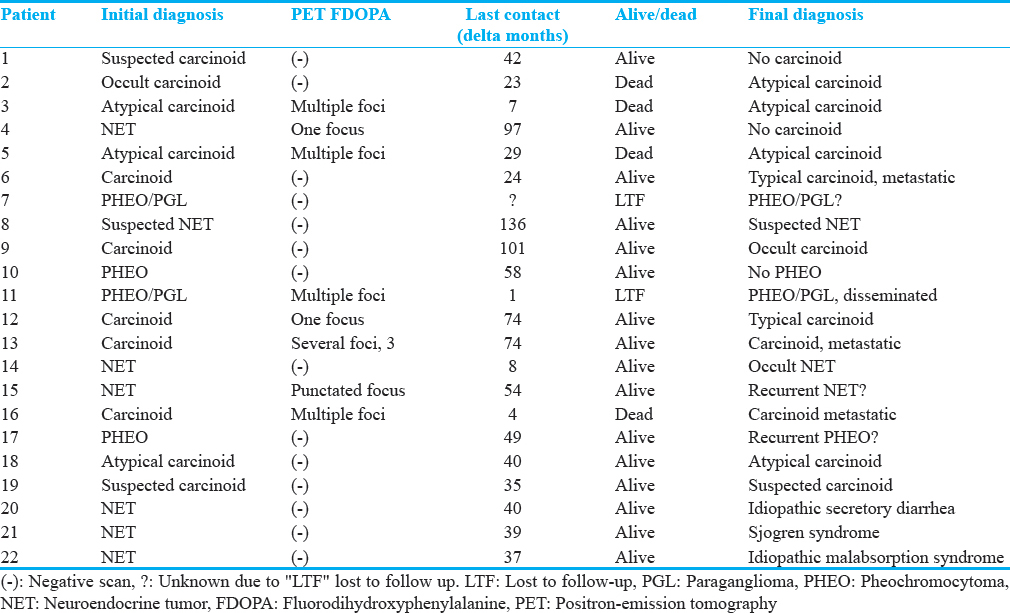
Results
The interpretations of the F-DOPA/PET studies by readers “masked” and “nonmasked” to pretest clinical information were similar. Table 1 includes the results of F-DOPA/PET studies performed with/without prior administration of carbidopa, and the standardized uptake values (SUV) for the abnormalities noted. Table 2 shows the referral diagnosis, duration of patients’ follow-up, and their condition and diagnosis at the time of the last contact as provided by the referring physicians. These final declarations, in view of the few surgical pathology results, were used to validate the majority of the interpretations of the F-DOPA scans.
Over all, focally increased distribution of F-DOPA was noticed in eight patients: five patients with final diagnosis of carcinoid, one with PGL, and two with a nonspecific neuroendocrine tumor (in one of them, atypical carcinoid was suspected on referral). As focal uptake of F-DOPA was seen in five of the 13 patients who received carbidopa and in three of those nine who had not, no overt difference in the frequency of abnormalities was apparent in both groups. No abnormally increased F-DOPA uptake was identified in the remaining 14 patients.
Evaluation of the detected abnormal foci
Of the five patients with final diagnosis of carcinoid, three of them, with atypical (#3) and metastatic carcinoids (#13 and #16), had foci of intense uptake of F-DOPA with very high SUV/max (23.5, 20.5 and 23.5). These three patients had the tumors visualized in the liver, and two of them died shortly after the scan; the third underwent surgical resection of the lesions detected. In the remaining two patients referred as with carcinoid, a punctate focus was seen on the F-DOPA scan in patient #12 (SUV/max value slightly elevated, 3.7) and multiple foci were reported in #5 (SUV/max, 5.3). This last patient underwent chemotherapy, external beam radiotherapy, and radioembolization of the liver before expiring 29 months after that scan. Regarding the patient with carcinoid, there was no clear correlation between the abnormality of the F-DOPA scans and the elevated serum serotonin. These elevated levels were present in four of them, but also increased in three patients with negative F-DOPA imaging [Table 2].
In patient #4 referred with an impression of neuroendocrine tumor in whom “tiny nonspecific” foci were reported on CT, and a small focus was visualized with F-DOPA (SUV/max value slightly elevated, 4.0), no confirmation of neuroendocrine tumor or carcinoid was obtained on follow-up at 97 months postscan (despite this, the tiny finding was considered a false positive for analysis). In the remaining patient referred with an impression of nonspecific neuroendocrine tumor (#15), a punctate, faint F-DOPA focus was visualized. At 54 months follow-up, this patient's clinical condition was stable.
The focal F-DOPA abnormalities detected in the only patient (#11) of the four patients with diagnosed or suspected PHEO or PGLs, had low SUV/max values (2.8). Direct positive confirmations of the abnormal F-DOPA findings were obtained in the two patients who underwent surgery (#13) or endoscopy (#12). Three of the known four dead patients at follow-up (at a mean time interval of 15 months poststudy; range 4–29), had multiple abnormal foci on F-DOPA scans (positive correlation). Two of them had a final diagnosis of atypical carcinoid and the other metastatic carcinoid. The remaining expired patient (at 23 months postscan), with diagnosis of atypical carcinoid, had a negative F-DOPA scan and was tabulated as false negative finding. Of the 15 patients known to be still alive at a median follow-up time of 49 months (range 8–136), 11 had correlated negative F-DOPA studies. The remaining four patients in whom some abnormalities were reported with the use of F-DOPA received a variety of treatments. In one of these patients, one F-DOPA-avid focus was suspected which we tabulated as a false positive interpretation despite the patient's unchanged condition at 97 months postscan. No follow-up could be obtained in three patients.
Table 3 is a summary of the correlation between the interpretation of F-DOPA/PET and the final diagnosis. Overall, there was correlation in 16 of the 22 patients. The test localized the presence of tumor in six of the eight patients with the final diagnoses of typical, metastatic, or atypical carcinoids (in three of the four patients with typical or metastatic carcinoids and in two of the four with atypical carcinoid). In contrast, F-DOPA uptake was noted in only one of the seven with questionable or no carcinoid on extended follow-up. Regarding the rest of the nonspecific neuroendocrine tumors patients, the F-DOPA/PET images were negative in two, who were on stable condition on the last follow-up. A punctuate focus was reported in patient (#4), with originally questionable neuroendocrine tumor diagnosis, also stable on follow-up. One of the four patients with the clinical diagnosis of PHEO and/or PGL had positive F-DOPA scans (which were negative in the other three).
Other imaging studies
Table 2 illustrates the findings of prior scintigraphy (In-111-OCT or I-123 MIBG) and CT scans. Ultrasound examinations and/or PET scans obtained with F-18-FDG were available in very few patients. The CT scans, obtained in all 22 patients, reported no lesions or nonspecific findings in 17; a neuroendocrine tumor in three (considered carcinoid, atypical, and questionable carcinoids, respectively), and a combination of specific and nonspecific findings in three patients. Regarding the patients with carcinoid and atypical carcinoid, in two, one with each diagnosis, there were more regions of increased F-DOPA accumulation than those reported with In-111-OCT. In two patients (with carcinoid and atypical carcinoid, respectively) PET demonstrated foci of F-DOPA uptake where no somatostatin receptor positive lesions were described on pentetreotide scan. Only one focus of F-DOPA deposition was noted in the one patient with carcinoid in whom two foci were suspected on OCT. Two foci of In-111-OCT uptake reported in one patient with questionable carcinoid were not confirmed using F-DOPA. In one patient with diagnosis of carcinoid, a photopenic lesion at the base of the skull on PET/FDG was imaged on OCT study but not on F-DOPA images. It was reported as corresponding to an arachnoid cyst on MR images and was tabulated as a true negative F-DOPA finding.
Of the five patients with clinically suspected PHEO or PGLs, the F-DOPA study revealed multiple lesions in the patient with PGLs. In this patient, only two of those abnormalities were reported (one questionably) on I-123-MIBG scan; none was evident with In-111-OCT. On the remaining four patients, in one (#15) a questionable focus was described on F-DOPA/PET and I-123-MIBG scans, but not with In-111-OCT. In another patient of those four (#17), two stable foci were reported with In-111 pentetreotide which were not evident on F-DOPA/PET or I-123-MIBG scan.
Illustrative case
A 63-year-old female (#13) was presented. A prior biopsy of terminal ileum revealed carcinoid. No symptoms of carcinoid syndrome were reported. Prior In-111-OCT was “probably normal”. CT scan revealed subcentimeter hypodensities in both lobes of the liver “too small to characterize” and a 1.5 cm × 0.7 cm soft tissue density in the right lower quadrant mesentery “possibly representing an enlarged lymph node.” F-DOPA/PET following administration of carbidopa showed two intense foci in the right lower abdominal quadrant (SUV/max, 20.5 and 13.5) probably corresponding to foci in the mesentery or small intestine. Figure 1 shows an intense focus very near or at the lower tip of the right hepatic lobe (SUV/max 13.5). These foci were reported as highly suspicious of the presence of neuroendocrine tumor. She underwent surgical resection of segment 6 of the liver and the terminal ileum; two of 26 lymph nodes were found with metastatic neuroendocrine tumor. The patient was alive at least 74 months after the F-DOPA study.
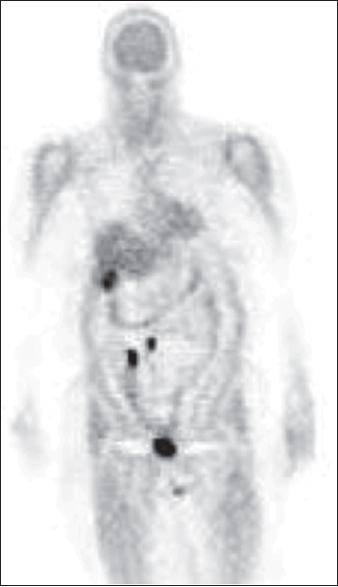
- 63-year-old woman (#13) with carcinoid identified on prior biopsy of terminal ileum. Previously, In-111-octreotide was unremarkable. Coronal image (head/low thighs) of positron-emission tomography scan obtained after oral administration of carbidopa and postintravenous injection of fluorine-18-fluorodihydroxyphenylalanine shows abnormal foci of fluorine-18-fluorodihydroxyphenylalanine accumulation: Two in the right lower abdomen and one at the lower tip of the right hepatic lobe. Radiotracer accumulation in the bladder is physiological. Two months later, the patient underwent surgical resection of segment 6 of the liver and terminal ileum; these and two of 26 lymph nodes were found with carcinoid. The patient was alive at least 74 months after the fluorine-18-fluorodihydroxyphenylalanine study.
Discussion
Carcinoid neoplasms overexpress somatostatin receptors. Somatostatin analogs (OCT) labeled with radionuclides such as In-111 pentetreotide (OctreoScan, OCT) made possible the scintigraphic imaging, augmented with single-photon emission computed tomography, of this type of neuroendocrine tumors and others.[14] The sensitivity of OCT for carcinoids, limited by lack of expression of some of the several receptors or to heterogeneity of the tumor tissue, has been reported in a range of 57%–85% overall, with frequent false positive localizations. Despite this, OCT frequently used as the initial imaging modality for visualization of carcinoids. Scintiscans obtained with MIBG labeled with I-131 and, more recently, with I-123, have been used as well. All these functional modalities are limited by poor anatomical resolution and are not always successful.[151617]
Patients with carcinoid have been studied with F-DOPA and the technique of PET, the great majority in Europe. In an early series of 17 patients comparing this modality with OCT, PET scans obtained with F-18-FDG, and morphological imaging procedures, the following sensitivities were calculated: F-DOPA, 63%; FDG/PET, 29%; OCT, 57%; and anatomical imaging, 73%. The authors considered that although the morphological procedures were most sensitive for metastases of carcinoid, F-DOPA/PET enabled best localization of primary tumors and lymph node staging.[18]
Imaging of a PHEO is important before surgery for exclusion of multifocality. Both conventional anatomical imaging (CT scan and MR images) and functional scans (I-131 or I-123 labeled MIBG, In-111-OCT, or FDG-PET) have been used.[1920212223] The scintigraphic method of choice, MIBG labeled with I-131, and more recently with I-123 is limited by poor resolution and lack of uptake of the radiopharmaceutical by a substantial number of the neoplasm.[20] A 75%–90% sensitivity for identification of PHEOs with OCT has been reported.[23] These last two tests are complementary as approximately 25% of PHEOs are visualized with MIBG only and another 25% only with OCT. The results obtained with FDG/PET have been discordant.[2122] Recently, the use of PET with F-DOPA as imaging agent has been reported with promising results in a limited number of patients.[2425]
This pilot study shows that F-DOPA scanning appears superior to In-111-OCT for localization of neuroendocrine tumors such as carcinoid tumors. The F-DOPA scanning was performed on consecutive, unselected patients referred with suspected, questionable, or known neuroendocrine tumors for evaluating the possibility that F-DOPA studies may help in its diagnosis and/or the evaluation of the extent of the disease. The diagnosis or its suspicion was based on clinical findings and laboratory abnormalities. In most of the patients, there was no similar evidence on CT or In-111-OCT. In others, the abnormal or suspected findings in those imaging modalities were very small or equivocal. In contrast with our population, we have noticed that larger lesions were described in a substantial number of the patients included in other published studies evaluating F-DOPA scans. We consider that the above-described characteristics of the lesions present in our patients are more representative of the usual difficulties in the diagnosis and management of neuroendocrine tumors.
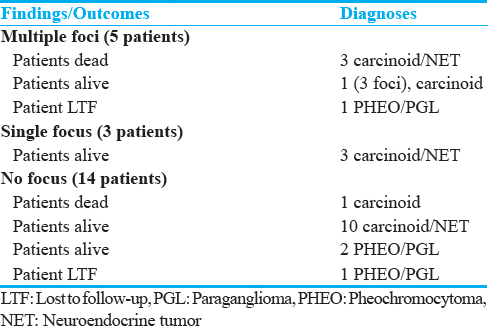
In addition, F-DOPA scanning appears to have some prognostic value as shown in Table 4. Not counting the two patients with PHEO/PGLs lost to extended follow-up, of the four patients with final diagnosis of carcinoid/neuroendocrine tumors in whom multiple foci of F-DOPA uptake were noted, three were dead, and one was alive on follow-up. The three carcinoid/neuroendocrine tumors patients in whom a single focus was detected and the 13 patients with a negative scanning were all alive when last seen.
Limitations
The number of patients studied is small and heterogeneous, related to its pilot nature, and the rarity of the diseases. That few patients underwent surgery postscan made it necessary to rely on extended follow-up for the evaluation of the imaging procedure.
Even with these limitations, F-DOPA scan provided relevant information to the referring physicians. On the one hand, it supported the referral diagnoses and allowed the localization of the lesions in four of the seven patients with typical and atypical carcinoids. In a few patients, the localization of additional unsuspected focal abnormalities was valuable for performing or canceling a specific treatment for a neuroendocrine tumor. The negativity of the F-DOPA scans of seven patients originally suspected of carcinoid/neuroendocrine tumor was consistent with the postscan long-term evolution of those patients with no evidence of those conditions. The finding of a small F-DOPA-avid focus in one patient referred with a neuroendocrine tumor despite no evidence of such condition in a follow-up of 97 months was considered a false positive case. Overall, these results show a substantial improvement compared with the impressions derived from the In-111 pentetreotide or CT scans obtained in the patients.
The small number of patients with PHEO/PGLs prevents definitive conclusions but, overall, the results are in line with those of the F-DOPA imaging of our patients with carcinoid/neuroendocrine tumors. Recently, Fiebrich et al.[26] considered F-DOPA superior to I-123-MIBG for visualization of tumors with catecholamine excess. A retrospective study of patient with these conditions concluded that F-DOPA appeared to be very sensitive for these entities.[27] In one of our patients with PGL, the F-DOPA scan was particularly valuable as it influenced the adoption of medical treatment instead of a new surgical intervention.
Conclusion
F-DOPA scanning added prognostic value, particularly when multiple abnormal foci versus a negative examination were considered.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We acknowledge Josephine Rini, MD for her support and Ms Miyuki Yoshida-Hay, CNMT for help with manuscript preparation.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2017/7/1/20/206658
References
- Clinical features, diagnosis, and localization of carcinoid tumors and their management. Gastroenterol Clin North Am. 1989;18:865-96.
- [Google Scholar]
- Surgical management of gastrointestinal carcinoid tumors. Adv Surg. 1995;28:317-36.
- [Google Scholar]
- Malignant carcinoid tumors. An analysis of 103 patients with regard to tumor localization, hormone production, and survival. Ann Surg. 1987;206:115-25.
- [Google Scholar]
- Consensus guidelines for the management and treatment of neuroendocrine tumors. Pancreas. 2013;42:557-77.
- [Google Scholar]
- Recent developments in the diagnosis and treatment of pheochromocytoma. Mayo Clin Proc. 1990;65:88-95.
- [Google Scholar]
- Pheochromocytomas, multiple endocrine neoplasia type 2, and von Hippel-Lindau disease. N Engl J Med. 1993;329:1531-8.
- [Google Scholar]
- Neuroendocrine gastrointestinal tumors – A condensed overview of diagnosis and treatment. Ann Oncol. 1999;10(Suppl 2):S3-8.
- [Google Scholar]
- Improved human brain 6-L (F-18) fluorodopa uptake by carbidopa pretreatment. J Cereb Blood Flow Metab. 1989;9(Suppl 1):S419.
- [Google Scholar]
- Carbidopa pretreatment improves image interpretation and visualization of carcinoid tumours with C-11-5-hydroxytryptophan positron emission tomography. Eur J Nucl Med Mol Imaging. 2006;33:60-5.
- [Google Scholar]
- Remote semi automated production of 6-[F18]fluoro-L-dopa for human studies with PET. Appl Radiat Isot. 1990;41:275-81.
- [Google Scholar]
- Kinetics and modeling of L-6-[18F] fluoro-dopa in human positron emission tomographic studies. J Cereb Blood Flow Metab. 1991;11:898-913.
- [Google Scholar]
- Somatostatin analogue scintigraphy in carcinoid tumours. Eur J Nucl Med. 1993;20:283-92.
- [Google Scholar]
- SPECT improves accuracy of somatostatin receptor scintigraphy in abdominal carcinoid tumors. J Nucl Med. 1996;37:1452-6.
- [Google Scholar]
- Iodine-131 metaiodobenzylguanidine scintigraphy of carcinoid tumors. J Nucl Med. 1986;27:1691-6.
- [Google Scholar]
- Scintigraphic imaging of carcinoid tumours with 131I-metaiodobenzylguanidine. Lancet. 1984;2:165.
- [Google Scholar]
- Whole-body 18F dopa PET for detection of gastrointestinal carcinoid tumors. Radiology. 2001;220:373-80.
- [Google Scholar]
- Metaiodobenzylguanidine and somatostatin in oncology: Role in the management of neural crest tumours. Eur J Nucl Med. 1994;21:561-81.
- [Google Scholar]
- Pheochromocytoma and the normal adrenal medulla: Improved visualization with I-123 MIBG scintigraphy. Radiology. 1985;155:789-92.
- [Google Scholar]
- Limited value of fluorine-18 fluorodeoxyglucose positron emission tomography for the imaging of neuroendocrine tumours. Eur J Nucl Med. 1998;25:79-83.
- [Google Scholar]
- Pheochromocytomas: Imaging with 2-[fluorine-18]fluoro-2-deoxy-D-glucose PET. Radiology. 1999;212:35-41.
- [Google Scholar]
- Radiolabelled somatostatin analogue (s) for peptide receptor scintigraphy and radionuclide therapy. Ann Oncol. 1999;10(Suppl 2):S23-9.
- [Google Scholar]
- Pheochromocytomas: Detection with 18F DOPA whole body PET – initial results. Radiology. 2002;222:507-12.
- [Google Scholar]
- 18F-FDOPA PET and PET/CT accurately localize pheochromocytomas. J Nucl Med. 2009;50:513-9.
- [Google Scholar]
- 6-[F-18]Fluoro-L-dihydroxyphenylalanine positron emission tomography is superior to conventional imaging with (123) I-metaiodobenzylguanidine scintigraphy, computer tomography, and magnetic resonance imaging in localizing tumors causing catecholamine excess. J Clin Endocrinol Metab. 2009;94:3922-30.
- [Google Scholar]
- Functional characterization of nonmetastatic paraganglioma and pheochromocytoma by (18) F-FDOPA PET: Focus on missed lesions. Clin Endocrinol (Oxf). 2013;79:170-7.
- [Google Scholar]






