Translate this page into:
Dilated Appendix: Is There More to It? Case Report and Brief Review of Literature with Radiologic-Pathological Correlation
* Corresponding author: Dr. Pranav Sharma, Department of Radiology, Yale New Haven Health Bridgeport Hospital, 267 Grant Street, Bridgeport, CT, USA. drpranavsharma29@gmail.com
-
Received: ,
Accepted: ,
Abstract
Mucocele of the appendix is rare and represents only the tip of the iceberg of underlying benign and malignant pathological processes. Intraoperative diagnosis is also tricky because the inflammation of the appendix often hides the tumor. The preoperative diagnosis is essential to differentiate appendiceal mucocele from acute appendicitis as the treatment varies from open surgical versus laparoscopic surgical approach and for decreasing intraoperative and postoperative morbidity and mortality rate. We present three cases of appendiceal mucocele. The purpose of this paper is to make the physicians aware of the entity, its associations and the effect on management. This review will provide radiologic and pathologic correlation for the preoperative diagnosis of benign and malignant causative processes and differential diagnostic considerations.
Keywords
Appendiceal mucocele
appendicitis
mucinous neoplasm of appendix
pseudomyxoma peritonei

HIGHLIGHTS
-
Appendicular mucocele (AM) is the chronic transformation of the appendix into a mucus-filled sac
-
The appendicular diameters of ≥15 mm are the threshold for diagnosing appendiceal mucocele, versus 6-mm outer diameter for the diagnosis of acute appendicitis
-
The “onion skin sign” is pathognomonic for mucocele. This appears as multiple echogenic layers surrounding a giant mucocele due to mucin reflecting the ultrasound beam at different giving the appearance of multiple layers
-
The presence of wall calcification supports the diagnosis of mucocele, but cannot exclude benign from malignant mucocele
-
Atypical imaging features such as irregular walls, soft-tissue mass, ascites, or pseudomyxoma peritonei can differentiate malignant versus benign etiology. The soft-tissue thickening and wall irregularity are highly suggestive of the neoplastic process.
INTRODUCTION
Appendicular mucocele (AM) refers to the chronic transformation of the appendix into a mucus-filled sac. It is generally detected in the fifth–seventh decades of life.[1] It accounts for 0.3%–0.7% of all appendiceal pathologies and 8% of malignancies of appendix, although has an uncertain histopathological diagnosis, and the terminology is unsettled.[2] The clinical presentation is often nonspecific right lower quadrant pain;[3] therefore, it is imperative for the clinician to be well aware of differentials. Management with simple appendectomy or right hemicolectomy depends on the preoperative diagnosis of the benign or malignant process.[4]
CASE REPORTS
Case 1
A 37-year-old male presented to the emergency department with the right lower quadrant abdominal pain for 3 days. The computed tomography (CT) scan demonstrated dilated appendix measuring up to 17 mm in diameter without the evidence of periappendiceal inflammatory changes, concerning for mucocele [Figure 1]. He underwent hemicolectomy. On histopathology, low-grade simple retention mucocele of the appendix was confirmed.
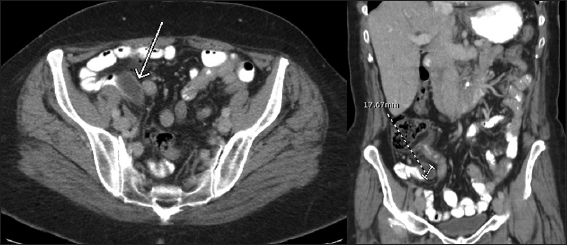
- A 37-year-old male with the right lower quadrant pain. Axial and coronal computed tomography scan showing dilated appendix measuring about 17 mm with near water density fluid in lumen and no periapendiceal inflammatory changes suggesting mucocele.
Case 2
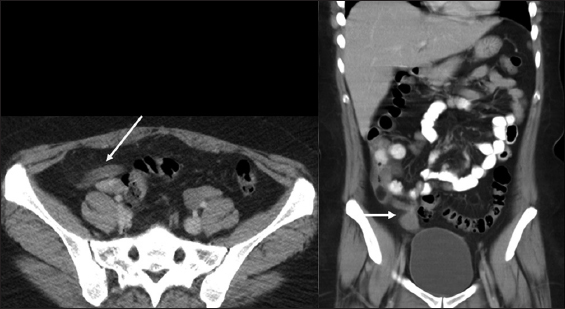
A 35-year-old female presented to the emergency department with worsening right lower quadrant abdominal pain for the past 2 days, raised white blood cell count of 20,000 cells/mm3 and mild transaminitis. CT scan demonstrated a mildly dilated appendix measuring 10 mm with the evidence of calcium within the mildly enhancing walls without surrounding inflammatory changes suggesting the diagnosis of equivocal appendicitis with incidental hypodense cystic structure abutting the tip of appendix [Figure 2]. She underwent laparoscopic appendectomy. Histopathology revealed simple retention mucocele of appendix.

- A 35-year-old female, axial and coronal computed tomography scan in a different patient showing fluid filled dilated appendix measuring up to 15 mm without periappendiceal inflammatory changes. Sagittal computed tomography image showing the calcium in appendix and partially visualized cyst. Note the fluid density structure near the tip of appendix which represented mesenteric cyst on histopathology.
Case 3
A 69-year-old female patient presented to the emergency department with the right lower quadrant abdominal pain for 3 days. The CT scan demonstrated thickened heterogeneously enhancing mass at the tip of appendix measuring up to 18 mm, proximal appendix measured up to 8 mm in diameter without evidence of periappendiceal inflammatory changes concerning for the appendiceal tumor [Figure 3]. He underwent hemicolectomy. On histopathology, low-grade mucinous neoplasm of appendix was confirmed [Figure 4].
- A 69-year-old female, axial and coronal computed tomography scan showing thickened heterogeneously enhancing mass at the tip of appendix measuring up to 18 mm, proximal appendix measured up to 8 mm in diameter without evidence of periappendiceal inflammatory changes concerning for the appendiceal tumor.
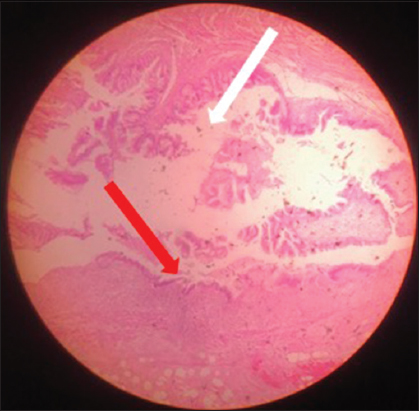
- A 69-year-old female with dilated appendix and enhancing mass at the tip of appendix. The histopathology (×10) H and E stained section of appendix shows thinned out and denuded mucosal lining (red arrow) along with areas showing mucus extending into the wall (white arrow). Findings are consistent with mucinous cystadenoma of appendix.
Pathological findings
Histopathologically, “mucocele” of the appendix may be caused by a variety of benign and malignant causes of obstruction of the lumen which lead to overproduction of mucus. It is subclassified depending on the depth of invasion of the wall, cellular atypia, extra-appendiceal mucin, and the presence of signet ring cells (associated with poor prognosis). Modern classification is divided into nonneoplastic variants including mucous retention cyst and mucosal hyperplasia and neoplastic variants, including mucosal adenoma (confined to mucosa, mild to moderate cytologic atypia and no atypical mitotic figures), low-grade mucinous neoplasm (low-grade atypia, the loss of muscularis mucosae, and or extra-appendiceal cells, mucocele rupture with extra-appendiceal mucin can lead to this) and mucinous cystadenocarcinoma (high-grade cytologic atypia) [Table 1]. Most benign mucoceles are due to mucinous adenoma which is sessile with dilated appendix with circumferential involvement of mucosa, without extra-appendiceal mucin and are asymptomatic with no recurrence risk after complete excision. Nonneoplastic variant results from chronic, long-standing obstruction of the appendiceal lumen by any nonneoplastic process and are called inflammatory, obstructive, simple mucocele, or retention cyst of the appendix. Mucinous neoplasm of the appendix of low malignant potential is one of the most common causes of “pseudomyxoma peritonei” associated with mucinous peritoneal implants and leads to extensive peritoneal disease without associated lymph node, lung, or liver metastases.[4,5]
| Nonneoplastic variants | Neoplastic variants |
|---|---|
| Mucosal retention cyst | Mucosal adenoma |
| Mucosal hyperplasia | Low-grade mucinous neoplasm |
| Mucinous cystadenocarcinoma |
Colonoscopy findings
Colonoscopy may show a soft erythematous mass, with a central crater due to the protrusion of appendiceal ostium, which can increase or decrease according to the respiratory movement. This condition is known as “Volcano Sign”-specific finding of appendiceal mucocele. This examination may show the presence of synchronic neoplastic lesions in the colon, which occur in up to 20% of the cases.[6,7]
Radiological features and pathological correlation
The ultrasound is the preliminary diagnostic tool and may be decisive for the differential diagnosis of appendiceal mucocele and acute appendicitis. The appendicular diameters of ≥15 mm are the threshold for diagnosing appendiceal mucocele, (sensitivity of 83% specificity of 92%) versus 6-mm outer diameter for the diagnosis of acute appendicitis.[3,8] At the ultrasound, mucocele appears as an elliptical cystic mass with or without acoustic shadowing from dystrophic mural calcification. A mucocele is usually encapsulated on ultrasound, with variable echogenicity in relation to the quantity and fluidity of the mucous contained. The inner wall can appear irregular due to the presence of debris or epithelial hyperplasia. The lumen of giant mucocele can have echogenic layers surrounded by mucin so-called “onion skin sign,” pathognomonic for mucocele.[9] Lesser dilated portion of appendix can give “drumstick or pear-shaped” appearance. On ultrasound, mucinous ascites show low-level echoes and poorly defined septation. Ultrasound-guided Fine needle aspiration has not been proposed to avoid dissemination of the mucous leading to pseudomyxoma peritonei.
The CT scan is the modality of choice showing near water density dilated appendix to more than 15 mm with or without wall calcification. When imaged with CT, simple mucocele appears as a well-defined water density mass in the right lower quadrant with curvilinear calcification within the wall. The presence of wall calcification supports the diagnosis of mucocele, but the presence of wall calcification cannot exclude benign from malignant mucocele. Atypical imaging features such as heterogeneity of outer wall diameter, calcifications, periappendiceal fat stranding, or intraperitoneal free fluid are not specific in differentiating malignant from benign mucoceles and can be seen with secondary inflammation/infective process. However, concerning features such as irregular walls, soft-tissue mass, ascites, or pseudomyxoma peritonei can differentiate malignant vs benign etiology. The soft-tissue thickening and wall irregularity are highly suggestive of the neoplastic process.[10] Intraluminal air foci or an air-fluid level within a mucocele are characteristics for secondary infection. CT findings of mucinous cystadenoma and mucocele are indistinguishable and appear as encapsulated low-attenuation cyst. At CT, low-grade mucinous neoplasm appears as a markedly distended appendix (>2 cm) containing low-attenuation mucin with wall calcification. It can demonstrate wall thickening, periappendiceal fat stranding and extraappediceal hypodense mucin from tumor infiltration or superimposed appendicitis. Search for extracellular mucin should be done once mucocele is identified in imaging, which may be localized in perieppendiceal or pericecal region, mesentery or omentum or in the dependent areas in peritoneum such as pouch of Douglas, rectovesical pouch, around ovaries or perihepatic space. CT findings of pseudomyxoma peritonei includes mucinous ascites (hyperdense, internal septations with fixed bowel loops versus central free floating bowel loops in simple ascites), peritoneal soft-tissue implants, scalloped appearance on solid organs with or without parenchymal involvement due to mass effect of tumor implants, omental caking, and may have linear or punctate calcifications of the mucinous deposits. Findings of small-bowel or ureteral obstruction or extensive upper abdominal disease associated with poor prognosis. On CT scan, the mucinous cystadenocarcinoma appears as low attenuating mucin filled dilated appendix or solid appendiceal mass, periappendiceal fat stranding/soft-tissue deposits, pseudomyxoma peritonei and intraperitoneal metastasis.[5] At CT, “arrowhead sign” (focal thickening of the cecal wall at appendiceal orifice with luminal contrast appearing as arrowhead), appendiceal wall thickening, peri-appendiceal fat stranding, small-bowel mural thickening, lymphadenopathy, appendicolith, and abscess points toward inflammatory etiology like acute appendicitis. Other differentials include cystic ovarian neoplasm or tubo-ovarian abscess, duplication cyst (tubular cystic structure communicating with bowel), hydrosalpinx (usually symptomatic), mesenteric cyst, and intussusception. Mesenteric cyst is reportedly rare and most often detected incidentally. They can be developmental, acquired, neoplastic or infectious or degenerative. In the second case, there was an incidental cystic structure abutting the tip of appendix which raised the possibility of mucinous deposit with appendicular mucocele. This was resected along with appendectomyand the pathology was a benign squamous lined cyst with underlying fibrous scar consistent with mesenteric inclusion cyst with squamous metaplasia. These findings should be well documented and if possible, the surgeon should be informed and notified of the possibility of carcinoma in 10% of the cases. Final diagnosis can be confirmed by histopathological evaluation of appendectomy specimen.
On magnetic resonance imaging, the features are similar to CT scan of a cystic mass which is hypointense on T1WI, hyperintense on T2WI; however, it is difficult to assess intraluminal air and calcification.[5]
Plain abdominal radiography may show soft-tissue opacity with curvilinear peripheral calcification in the right lower quadrant. On barium enema, there may be a sub-mucosal or extrinsic mass indenting and displacing the medial wall of caecum with filling the defect.[5]
The treatment of AM is en bloc resection with conventional surgery preferred over laparoscopic surgery due to the risk of rupture. When benign mucocele is suggested, simple appendectomy is performed. If malignant imaging features are suspected, then right hemicolectomy is performed along with abdominal exploration due to the association of AM with other mucinous neoplasms of colon and ovary.[11]
CONCLUSION
Due to its rarity, mucocele of appendix continues to fascinate the surgeon as well as the radiologist and pathologist likewise. It often causes a diagnostic dilemma in the setting of nonspecific symptoms. Although US is often the primary diagnostic modality that is performed, CT is the modality of choice for better characterization. Although a rare disease, surgical management is mandatory because the risk of malignant transformation and prevention of pseudomyxoma peritonei due to rupture of the mucocele itself. Therefore, preoperative diagnosis or suspicion is required for carefully planned resection to excise the tumor.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Laparoscopic appendectomy. The Journal of the American Association of Gynecologic Laparoscopists. 2003;10:166-8.
- [Google Scholar]
- Sternberg's Diagnostic Surgical Pathology. Lippincott Williams &Wilkins; 2004.
- Appendiceal mucocele:Case reports and review of current literature. World J Gastroenterol. 2008;14:2280-3.
- [Google Scholar]
- Mucinous appendiceal neoplasms:Pathologic classification, clinical implications, imaging spectrum and mimics. Abdom Radiol (NY). 2018;43:2913-22.
- [Google Scholar]
- Neoplasms of the appendix:Pictorial review with clinical and pathologic correlation. Radiographics. 2017;37:1059-83.
- [Google Scholar]
- Mucus containing cystic lesions “mucocele” of the appendix:The unresolved issues. Int J Surg Oncol. 2015;2015:139461.
- [Google Scholar]
- Appendiceal mucinous neoplasms:A clinicopathologic analysis of 107 cases. Am J Surg Pathol. 2003;27:1089-103.
- [Google Scholar]
- Appendiceal outer diameter as an indicator for differentiating appendiceal mucocele from appendicitis. Am J Emerg Med. 2006;24:801-5.
- [Google Scholar]
- Sonographic appearance of a giant appendicular mucocele. J Clin Ultrasound. 2011;39:290-2.
- [Google Scholar]
- Appendiceal mucocele:A diagnostic dilemma in differentiating malignant from benign lesions with CT. AJR Am J Roentgenol. 2013;201:W590-5.
- [Google Scholar]
- Surgical treatment of mucocele of the appendix:A systematic review and case report. J Surg Case Rep. 2018;2018:rjy102.
- [Google Scholar]






