Translate this page into:
Diagnostic and Clinical Management of Skull Fractures in Children
Address for correspondence: Dr. Christoph Arneitz, Feschnigstraße 11, 9020 Klagenfurt, Austria. E-mail: christoph.arneitz@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
The indications of routine skull X-rays after mild head trauma are still in discussion, and the clinical management of a child with a skull fracture remains controversial. The aim of our retrospective study was to evaluate our diagnostic and clinical management of children with skull fractures following minor head trauma.
Methods:
We worked up the medical history of all consecutive patients with a skull fracture treated in our hospital from January 2009 to October 2014 and investigated all skull X-rays in our hospital during this period.
Results:
In 5217 skull radiographies, 66 skull fractures (1.3%) were detected. The mean age of all our patients was 5.9 years (median age: 4.0 years); the mean age of patients with a diagnosed skull fracture was 2.3 years (median age: 0.8 years). A total of 1658 children (32%) were <2 years old. A typical boggy swelling was present in 61% of all skull fractures. The majority of injuries were caused by falls (77%). Nine patients (14%) required a computed tomography (CT) scan during their hospital stay due to neurological symptoms, and four patients had a brain magnetic resonance imaging. Nine patients (14%) showed an intracranial hemorrhage (ICH; mean age: 7.3 years); one patient had a neurosurgery because of a depressed skull fracture. Nine patients (14%) were observed at our pediatric intensive care unit for a mean time of 2.9 days. The mean hospital stay was 4.2 days.
Conclusions:
Our findings support previous evidence against the routine use of skull X-rays for evaluation of children with minor head injury. The rate of diagnosed skull fractures in radiographs following minor head trauma is low, and additional CT scans are not indicated in asymptomatic patient with a linear skull fracture. All detected ICHs could be treated conservatively. Children under the age of 2 years have the highest risk of skull fractures after minor head trauma, but do not have a higher incidence of intracranial bleeding. Neuroobservation without initial CT scans is safe in infants and children following minor head trauma and CT scans should be reserved for patients with neurological symptoms.
Keywords
Computed tomography
neuroobservation
pediatric
radiography
skull fracture

INTRODUCTION
Minor head injury is common in children and an important cause of morbidity and mortality in the pediatric population. In many institutions, skull radiographs are broadly used in children with minor head trauma although several studies suggest that the guidelines for skull radiography in children are too wide and a skull fracture is not a reliable indicator of an intracranial injury.[123] Following the instructions of recent guidelines can achieve a significant reduction of skull X-rays without detriment of any patient.[24]
The clinical management of children with a skull fracture differs among institutions and individuals. While children and adolescents with an isolated skull fracture are routinely admitted to our hospital for neurological observation, some authors suggest that isolated linear skull fractures can be safely discharged home directly from the emergency department (ED).[5678] Several guidelines include a cerebral computed tomography (cCT) scan for children with an isolated skull fracture without any neurological symptom.[91011] While the number of cCT scans in the United States increased rapidly in the past two decades, at our department, a cCT is reserved for neurologically impaired children after blunt head trauma.[121314]
Our numbers of skull radiographs seem to be high, reaching more than 1000 skull X-rays per year. The aim of our retrospective study was to evaluate the diagnostic use of skull radiography in children following minor head trauma and approve our clinical management of patients with skull fractures.
METHODS
All skull radiographs of patients under the age of 18 years taken at our ED from January 2009 to October 2014 were documented and analyzed retrospectively. The study population included all patients with a diagnosed skull fracture in two-plane radiographs (exclusion of facial and basal skull fractures) after minor head trauma and was divided in infants younger than 2 years and children between 2 and 18 years old. Minor head trauma was defined as history or physical signs of blunt trauma to the head in an infant or child.[15]
The collected data included age, sex, mechanism of injury, presence of neurological symptoms or clinical signs, type of skull fracture, diagnostic management, surgical intervention, length of hospital stay, complications, and outcome. cCT scans were performed in children with neurological symptoms. All radiological investigations were seen by a pediatric surgeon and routinely analyzed by a pediatric radiologist. In the case of a suspicious brightening line in the radiography, an ultrasound was done to confirm or exclude the diagnosis. Each child with a recently sustained skull fracture was admitted to hospital for close neurological observation for at least 5 days. Six weeks after the trauma, each patient was ordered to a clinical inspection.
For statistical analysis, a Chi-square test and Fisher's exact test were used; P < 0.05 was considered to be statistically significant.
RESULTS
Skull radiographs were performed in 5217 patients. The mean age of all our patients was 5.9 years (median age: 4.0 years). A total of 1685 children (32%) were <2 years old. The study population consisted of 66 patients (1.3%) with a mean age of 2.3 years (median age: 0.8 years). 5151 patients with normal skull radiography were excluded from our study.
The majority of our patients with a skull fracture were male (58%). The majority of injuries were caused by falls (79%) followed by bicycle accidents (4.5%), struck by object (4.5%), battered child (3%), car-pedestrian accident (1.5%), tobogganing accident (1.5%); and in four cases, the trauma was unclear (6%).
The most common fracture localization was parietal (77%) followed by occipital (15%), frontal (6%), and temporal (1.5%). Three patients (4.5%) had a depressed fracture, two of them were treated conservatively and one required neurosurgery for elevation of a depressed fragment.
A typical boggy swelling was present in 61% of all skull fractures. Two patients had a compound fracture, one child had a hemotympanum, and another presented with a palpable notch. Four patients (6%) were completely asymptomatic. In 18 cases, a radiological suspected skull fracture was confirmed by ultrasound.
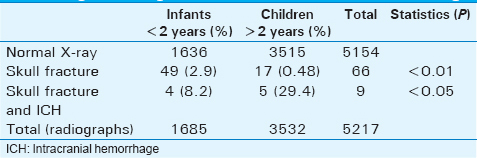
Forty-nine patients with a skull fracture were younger than 2 years and 4 (8.2%) of them had an intracranial hemorrhage (ICH). Seventeen patients between 2 and 18 years of age had a skull fracture, whereof 5 (29.4%) were diagnosed with an ICH. Skull fractures were statistically significant more frequent in children <2 years old compared to children beyond this age (P < 0.01). The incidence of an ICH in patients with a skull fracture was not higher in the younger age group (P = 0.042) [Table 1].
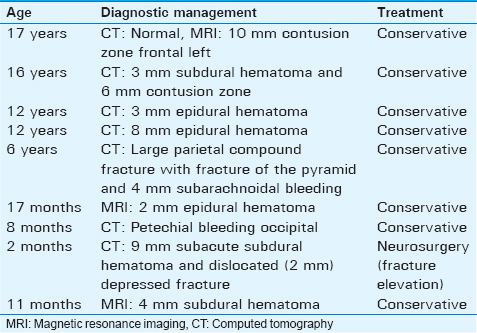
Five patients (10.6%) required a CT scan immediately at admission due to altered level of consciousness or reduced Glasgow Coma Scale and four patients had a CT scan during hospital stay because of increasing neurological symptoms. The CT scans were considered as normal in three cases; six patients showed an ICH, which could be treated conservatively. A 2-month old girl with a subacute, small subdural hematoma was operated on a depressed skull fracture.
Four patients had a brain magnetic resonance imaging (MRI) during hospital stay due to persistent neurological complaints. One of them had a contusion zone visible in the MRI without pathological findings on the initial CT scan, in two patients a small ICH was present, and in one patient the MRI was considered as normal. None of them required neurosurgery [Figure 1].

- Diagnostic management.
The majority of our patients (81.1%) were admitted to our hospital directly after the trauma. Twelve patients with a skull fracture visited our hospital in delay, between 1 and 10 days (mean: 4.1 days) after their head injury, because of a persistent boggy swelling. Ten of them had no neurological symptoms and could be discharged without further radiological investigations. One patient had a CT scan because of a depressed fracture in the skull X-ray without therapeutic consequences. Another patient had a brain MRI, which showed a small subdural hematoma and was treated conservative. One patient denied hospital admission and was discharged.
In summary, nine patients showed an ICH (mean age: 7.3 years; median: 5.9 years), which was diagnosed by a CT scan in 6 cases and MRI in 3 cases. All ICHs could be managed conservatively [Table 2].
The patients with an ICH were observed at our pediatric intensive care unit for a mean time of 2.9 days. All other patients had close neuroobservation at the regular hospital ward and their mean hospital stay was 4.2 days. Forty-nine patients (74%) were available for a clinical control after 6 weeks; no complications occurred.
DISCUSSION
Blunt head trauma is very common in children and can result in a skull fracture in up to 30%.[16] In our study, the rate of diagnosed fractures in two-plane skull X-rays following head trauma is particularly low. The diagnosis of a skull fracture had to be confirmed by an additional ultrasound in 18 patients. Hence, the number of reliable diagnosed skull fractures in two-plane radiographs is below 1%.
Lloyd et al., demonstrated in their prospective study that out of 6011 skull radiographs only 162 skull fractures were diagnosed (2.7%). All patients with ICH on CT scan had neurological abnormalities.[1] Erlichman et al., reviewed 114 children with a skull fracture in their retrospective study. They found 29 patients (25%) with an ICH, but all ICHs were small and did not require neurosurgery.[17] Powell et al., presented in their prospective series 43.904 children after minor head trauma and diagnosed 350 patients with an isolated linear skull fracture. None of them required a neurosurgical intervention.[5]
Mossop and Soysa as well as Simon and Dodds demonstrated a significant reduction of skull X-rays after implementation of guidelines, without detriment of any patient.[24] In our series, skull radiographs were performed in all patients following minor head trauma, even in patients without any clinical sign. In summary, we had to radiograph over 1000 children to diagnose one completely asymptomatic patient with a skull fracture without any clinical relevance. Our indications for skull radiography in children seem to be too wide and skull X-rays should only be recommended for infants with suspected nonaccidental injury, penetrating trauma, or compound fracture and in presence of a boggy swelling.[124]
We found a low cCT rate in our study population (14%). This in strong contrast to other published studies, where the CT rate is up to 100% in patients with a skull fracture.[15101617]
At our department, a cCT is reserved for neurologically impaired children after minor head trauma. The routine use of CT scans, after radiologically diagnosed skull fractures, is not necessary in children without clinical signs of intracranial injury and neuroobservation is the reasonable management for patients with normal level of consciousness. There is strong evidence for an increased risk of fatal cancer from CT scans in childhood.[1214]
The clinical management of children with a skull fracture differs among institutions and individuals. Neurosurgeons are more willing to discharge patients than do pediatric surgeons.[8] While children and adolescents with an isolated skull fracture are routinely admitted to our hospital for neurological observation, several authors suggest that isolated linear skull fractures can be safely discharged home directly from the ED.[5678] However, all of the published patients had a cCT scan at their ED evaluation and a recent intracranial injury was excluded from the study. In neurologically normal children, an evolving intracranial injury can be difficult to recognize at presentation, especially in infants younger than 2 years.[1018] In concordance with published studies, children younger than 2 years are more likely to sustain a skull fracture compared to older children, but do not have a higher incidence of intracranial bleeding.[5101819]
Neurosurgical intervention is rare and also depressed fractures measuring <5 mm can be safely treated conservatively.[20] All our patients with ICHs could be treated conservatively. Only one patient needed neurosurgical repair of a depressed occipital skull fracture.
The limitations of this study are, that is, the study was done in retrospect and the cohort was small.
CONCLUSIONS
Our findings support previous evidence against the routine use of skull X-rays for evaluation of children with minor head injury. The rate of diagnosed skull fractures in radiographs following minor head trauma is low and neurosurgical interventions are rare. We conclude that there is no need for routine skull radiography and in case of neurological symptoms a cCT scan is the right diagnostic approach. Additional CT scans are not indicated in asymptomatic patient with a linear skull fracture. Children under the age of 2 years have the highest risk of skull fractures after minor head trauma, but do not have a higher incidence of intracranial bleeding. Neuroobservation without initial CT scans is safe in infants and children following minor head trauma and CT scans should be reserved for patients with neurological symptoms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2016/6/1/47/194261
REFERENCES
- Predictive value of skull radiography for intracranial injury in children with blunt head injury. Lancet. 1997;349:821-4.
- [Google Scholar]
- The use of skull X-rays in head injury in the emergency department - A changing practice. Ann R Coll Surg Engl. 2005;87:188-90.
- [Google Scholar]
- Role of skull radiography in the initial evaluation of minor head injury: A retrospective study. Acta Neurochir (Wien). 1994;129:11-4.
- [Google Scholar]
- The use of skull X-rays in the accident and emergency department. Ann R Coll Surg Engl. 2003;85:120-2.
- [Google Scholar]
- Isolated linear skull fractures in children with blunt head trauma. Pediatrics. 2015;135:e851-7.
- [Google Scholar]
- Impact of newly adopted guidelines for management of children with isolated skull fracture. J Pediatr Surg. 2014;49:1856-60.
- [Google Scholar]
- Isolated skull fractures: Trends in management in US pediatric emergency departments. Ann Emerg Med. 2013;62:327-31.
- [Google Scholar]
- Variation in specialists’ reported hospitalization practices of children sustaining blunt head trauma. West J Emerg Med. 2013;14:29-36.
- [Google Scholar]
- A decision rule for identifying children at low risk for brain injuries after blunt head trauma. Ann Emerg Med. 2003;42:492-506.
- [Google Scholar]
- Nondepressed linear skull fractures in children younger than 2 years: Is computed tomography always necessary? Clin Pediatr (Phila). 2012;51:745-9.
- [Google Scholar]
- Diagnostic testing for acute head injury in children: When are head computed tomography and skull radiographs indicated? Pediatrics. 1997;99:E11.
- [Google Scholar]
- Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: A retrospective cohort study. Lancet. 2012;380:499-505.
- [Google Scholar]
- The ‘image gently’ campaign: Increasing CT radiation dose awareness through a national education and awareness program. Pediatr Radiol. 2008;38:265-9.
- [Google Scholar]
- Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001;176:289-96.
- [Google Scholar]
- Evaluation and management of children younger than two years old with apparently minor head trauma: Proposed guidelines. Pediatrics. 2001;107:983-93.
- [Google Scholar]
- Pediatric skull fractures: The need for surgical intervention, characteristics, complications, and outcomes. J Neurosurg Pediatr. 2014;14:205-11.
- [Google Scholar]
- Association between linear skull fractures and intracranial hemorrhage in children with minor head trauma. Pediatr Radiol. 2010;40:1375-9.
- [Google Scholar]
- Identification of children at very low risk of clinically-important brain injuries after head trauma: A prospective cohort study. Lancet. 2009;374:1160-70.
- [Google Scholar]
- Computed tomographic scan in head trauma: What is the rational in children? Eur J Pediatr Surg. 2013;23:444-53.
- [Google Scholar]
- Rational management of simple depressed skull fractures in infants. J Neurosurg. 2005;103(1 Suppl):69-72.
- [Google Scholar]






