Translate this page into:
Diagnostic Accuracy of Color Doppler and Calcium Scoring versus Dual-Energy Computed Tomography Angiography in the Assessment of Peripheral Arterial Diseases of Lower Limb

*Corresponding author: Sachin Khanduri, Department of Radiodiagnosis, Era’s Lucknow Medical College and Hospital, Lucknow, Uttar Pradesh, India. drsachinrad@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yadav V, Khanduri S, Yadav P, Pandey S, Tyagi E, Yadav H, et al. Diagnostic accuracy of Color Doppler and calcium scoring versus dual-energy computed tomography angiography in the assessment of peripheral arterial diseases of lower limb. J Clin Imaging Sci 2020;10:45.
Abstract
Objectives:
Peripheral arterial disease (PAD) leads to narrowing and hardening of arteries which leads to increased risk of lower extremity amputation. Hence, the accuracy of non-invasive diagnostic methods such as calcium scoring and color Doppler needs to be assessed in comparison to the gold standard dual-energy computed tomography (DECT) angiography. This study aims to evaluate the accuracy of color Doppler and calcium scoring when compared to DECT angiography in the assessment of PAD of the lower limb. It is a cross- sectional retrospective study.
Material and Methods:
The study included 55 patients aged between 40 and 70 years. All the patients with symptoms suggestive of PAD underwent color Doppler study of lower limb arterial system. Afterward, the patient underwent CT angiography. The first plain images were taken for calcium scoring following which contrast was given and further images were taken.
Results:
As compared to CT angiography assessment, Doppler assessment was 88.1% sensitive but only 69.2% specific with diagnostic accuracy of 83.6%. For angiographically detected atheromatous changes, color Doppler had sensitivity and specificity of 86.2% and 76.9%. The derived cutoff value >149.1 of calcium score in lower limb arteries was in 100% agreement with CT angiography detected PAD, whereas, for atheromatous changes, total calcium score at a cutoff value of >842.2 had sensitivity and specificity of 75.9% and 80.8%.
Conclusion:
Calcium scoring as compared to color Doppler has a higher diagnostic efficacy for the detection of DECT angiography confirmed PAD, whereas calcium score lacks adequate sensitivity at projected cutoff in the evaluation of atheromatous changes.
Keywords
Dual-energy computed tomography
Peripheral arterial disease
Color Doppler
Calcium score
INTRODUCTION
The atheromatous narrowing or occlusion of extremities known as peripheral arterial disease (PAD) is a part of the global vascular problem of diffuse atherosclerosis. Although symptoms vary, mortality is primarily due to cardiac and cerebrovascular events. Management strategies range from conservative (for intermittent claudication) to angioplasty, surgical revascularization, or amputation for limb threatening ischemia.[1]
Conventional angiography is the gold standard study for PAD diagnosis while other modalities such as duplex ultrasound, MRI angiography, and CT angiography provide great anatomical details and thus useful in interventions.[2]
Invasive nature of conventional angiography restricts its frequent use, which is overcome by color Doppler ultrasound in which arteries at depth of 6 cm or less are easily evaluated [3] and computed tomography angiography (CTA) which has become the preferred choice for diagnosing and evaluating PAD in a manner comparable to invasive angiography and other non-invasive imaging methods.[4] The use of CT also helps to assess and quantify vascular calcification which is characteristic of atherosclerosis.[5]
Coronary calcium scoring using CT serves as a marker for the extent of atherosclerosis and is used to risk stratify patients.[6] Lower extremity arterial calcium score has been found to be an indicator of disease severity and outcome.[7]
Recent innovation like dual-energy computed tomography (DECT) is not only a feasible and accurate diagnostic method in the assessment of symptomatic peripheral arterial occlusive disease but has superior results as compared to the conventional bone removal technique and less dependent on vessel wall calcifications. Dual-energy CT evaluation also works efficiently with low contrast medium volume. DECT has been found to be a non-invasive and accurate diagnostic procedure in the diagnostic assessment of PAD with high diagnostic value.[8,9]
With this background, we aim to assess the efficacy of color Doppler and calcium scoring when compared to DECT angiography in the assessment of PAD of lower limb.
MATERIAL AND METHODS
A cross-sectional retrospective study was conducted on 55 patients for a period of 18 months on patients aged between 40 and 70 years with normal kidney function and symptoms suggestive of PAD such as pain, fatigue, burning, or discomfort in the muscles (feet, calves, or thighs), dark or blue looking skin of legs, non-healing sores, low or absent pulse of leg, withered or atrophied calf muscles, loss of hair over lower limbs, and painful non-bleeding sores of toe or toes. Patients who were allergic to contrast, with deranged kidney function test and with an active skin infection over lower limb, were excluded from the study.
Color Doppler assessment was done on GE VOLUSON P9 machine using curvilinear (25–5 MHz) and linear (5–7 MHz) probe with combined real time B mode and pulsed wave Doppler from aortic bifurcation till the level of ankle distally. Lower limb vessels were evaluated on gray scale for luminal narrowing, thrombosis, and atheromatous plaque [Figure 1]. On color and spectral analysis, lower limb vessels were evaluated for the absence of color flow within the lumen or loss of laminar flow pattern or monophasic waveform, all of which are suggestive of PAD [Figure 2]. Arteries with clear lumen, thin uniform wall, and with triphasic flow were considered normal. The angle of Doppler was kept <60° and color box was kept small with optimal pulse repetition frequency to detect the accurate velocity and color flow.

- Atheromatous changes in the left femoral artery on ultrasound. Arrows indicate echogenic plaques in wall of artery.
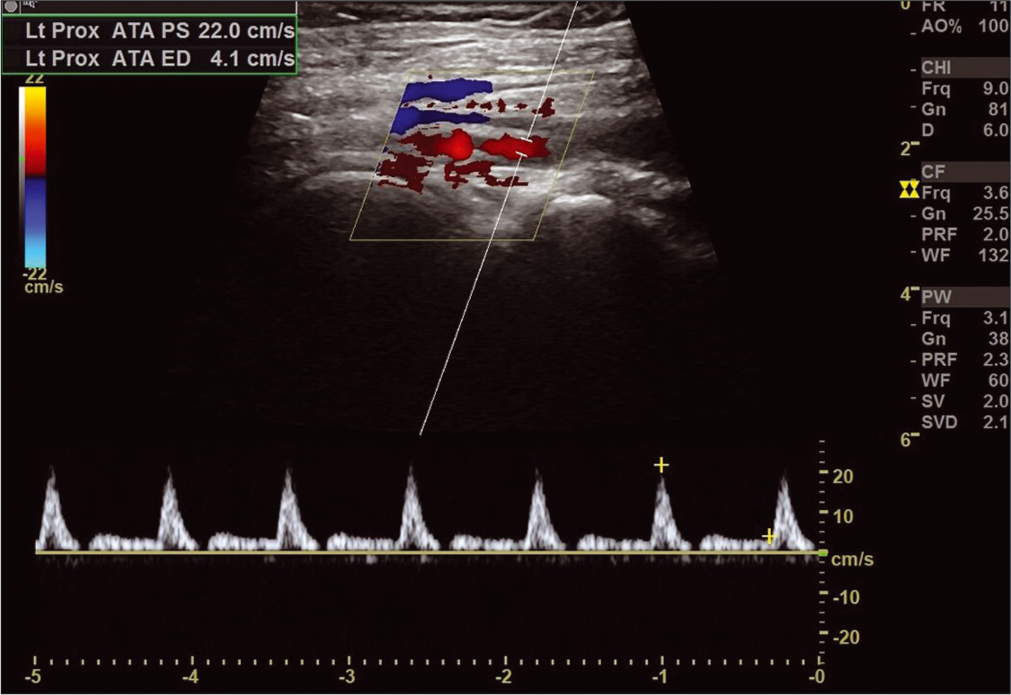
- Monophasic flow in the left anterior tibial artery
CT angiography was performed using the third-generation dual-source dual-energy 384 slice CT scanner (SOMATOM force). Plain images were taken for calcium scoring which was evaluated in three segments, namely, iliac, thigh, and calf region for both lower limbs, respectively [Figures 3 and 4]. Agatston equivalent scoring system was used for the evaluation of calcium score.
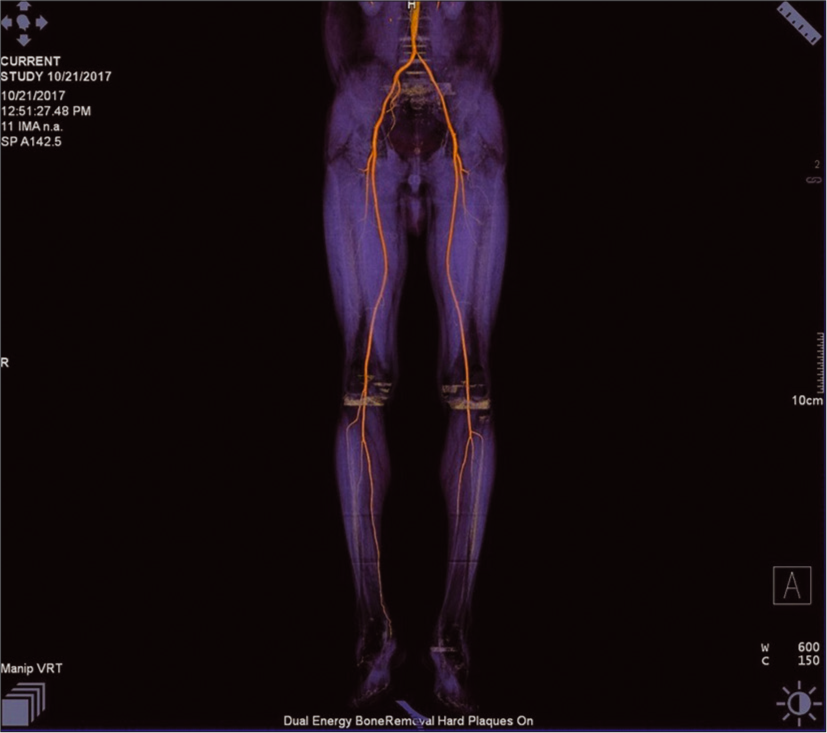
- 3D volume rendering with bone removal dual-energy computed tomography image of lower limb arteries showing stenosis in the left posterior tibial and dorsalis pedis artery.
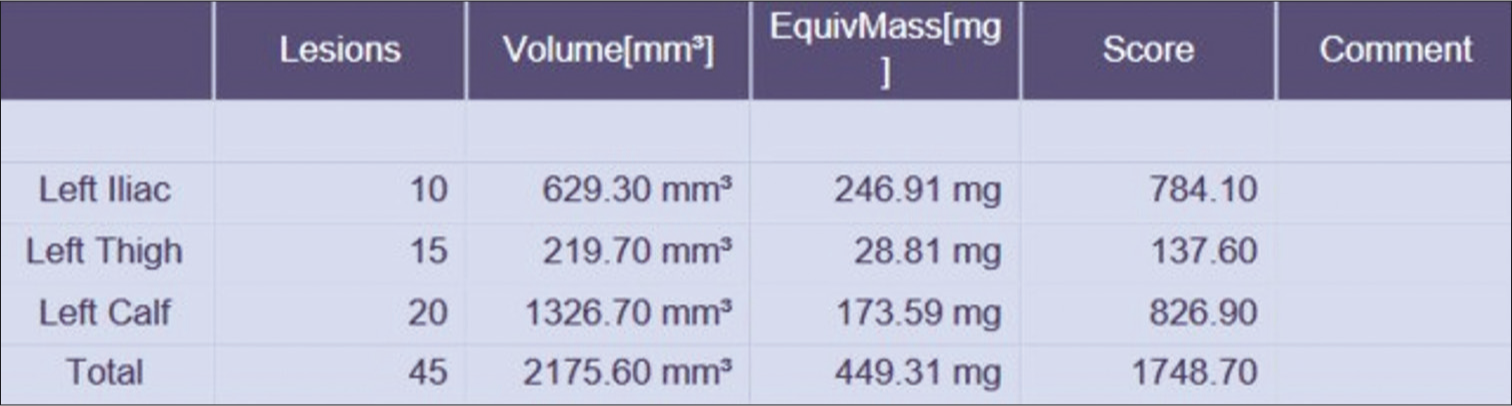
- Result of segmental calcium score of the left limb of the patient.
Afterward, 140 ml of non-ionic iodinated contrast material was given with a power injector at an injection rate of 4 ml/s followed by a bolus injection of 40 ml of saline at the same flow rate and images acquired for angiography.
Bolus triggered that acquisition timing was used to initiate the CTA. For this purpose, a region of interest was placed in the distal aorta. The scan was started immediately after the enhancement curve reached its peak with a minimum of at least 200 Hounsfield units (HU). Data were acquired in a craniocaudal direction with the following scanning parameters: Tube A: Tube voltage of 80 kV, reference current time product of 250 mAs; tube B: Sn140 kV, where Sn indicates the use of an integrated tin filter; reference current time product of 150 mAs, 1280.6 mm collimation, 0.6 pitch, and 0.5 s rotation time. CTA data were transferred to syngo.via workstation for image analysis. The data were post processed through dual-energy body bone removal technique and images were analyzed for atheromatous changes and luminal narrowing.
For calcium scoring, lower extremity was divided into three segments: The iliac, thigh (above-knee) segment, and calf (below-knee) segment. Calcium score was analyzed using standardized calcium scoring software. Calcification with a cross-sectional area >1 mm2 and a density of >130 HU were identified on axial images of the lower limb and scored. Calcium score for the desired segment was determined and expressed as Agatston score.
RESULTS
We evaluated 55 patients (49 males and 6 females) using color Doppler followed by calcium scoring through DECT assessment. All the patients were finally subjected to DECT angiography which was taken as the gold standard for final diagnosis. Out of 55, 23 were <50 years, 13 were of age group 50–60 years, and 19 were of age group 60–70 years.
On final DECT angiography findings, out of 55 cases, 13 cases were normal, 42 were abnormal with narrowing in 13 cases, and atheromatous changes in 29 cases, as shown in Table 1.
| DECT angiography finding | No. of cases | Percentage |
|---|---|---|
| Normal | 13 | 23.6 |
| Abnormal | 42 | 76.4 |
| Atheromatous changes | 29 | 69.0 |
| Narrowing | 13 | 31.0 |
On Doppler assessment, 41 (74.5%) cases were with abnormal findings and 14 (25.5%) were with normal findings, as shown in Table 2. The proportion of abnormal Doppler findings was higher among those with abnormal DECT angiography finding (88.1%) as compared to those having normal DECT angiography finding (30.8%). The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of color Doppler for the assessment of PAD were calculated as 88.1%, 69.2%, 90.2%, 64.3%, and 83.6%, respectively.
| Doppler assessment | Total | DECT abnormal (n=42) |
DECT normal (n=13) |
|||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Abnormal | 41 | 74.5 | 37 | 88.1 | 4 | 30.8 |
| Normal | 14 | 25.5 | 5 | 11.9 | 9 | 69.2 |
χ2=17.19; P<0.001
Doppler diagnosed atheromatous changes in 31 (56.4%) cases. The proportion of Doppler detected atheromatous changes was significantly higher among those having DECT detected atheromatous changes (86.2%) as compared to those having normal DECT for atheromatous changes (23.1%) (P < 0.001), as shown in Table 3.
| Doppler assessment | Total (n=55) | DECT athero (n=29) |
DECT normal (n=26) |
|||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Atheromatous changes | 31 | 56.4 | 25 | 86.2 | 6 | 23.1 |
| Normal | 24 | 43.6 | 4 | 13.8 | 20 | 76.9 |
χ2=22.22; P<0.001. Sensitivity=86.2; specificity=76.9%; PPV=80.6%: NPV=83.3%; accuracy=81.8%
On calcium scoring, mean calcium scores for different arteries ranged from 183.95 ± 314.36 (iliac right) to 351.27 ± 272.46 (calf right) among cases with abnormal angiographic findings, whereas among those with normal angiographic findings, they ranged from 0 (iliac left and right and calf right and left) to 17.63 ± 33.50 (thigh left), as shown in Table 4. Total calcium score was 1515.1 ± 1198.3 in patients with abnormal angiographic findings as compared to 30.18 ± 57.36 among those with normal angiographic findings. Statistically, mean calcium scores for all the three locations in both the sides were significantly higher in cases with abnormal angiographic finding as compared to those with normal angiographic findings (P < 0.05). Overall too, mean total calcium scores were significantly higher among those with abnormal angiographic findings as compared to those having normal angiographic findings (P < 0.001).
| Characteristic | Abnormal (n=42) | Normal (n=13) | Statistical significance P-value |
|---|---|---|---|
| Iliac right | 183.95±314.36 | 0.00 | t=2.096; P=0.041 |
| Iliac left | 277.05±293.28 | 0.00 | t=3.384; P=0.001 |
| igh right | 202.61±269.82 | 12.55±23.86 | t=2.520; P=0.015 |
| igh left | 287.30±292.44 | 17.63±33.50 | t=3.297; P=0.002 |
| Calf right | 212.90±239.15 | 0.00 | t=3.189; P=0.002 |
| Calf left | 351.27±272.46 | 0.00 | t=2.096; P<0.001 |
| Total calcium score | 1515.2198.3 | 30.18+57.36 | t=4.438;P<0.001 |
On receiver-operator characteristic curve analysis to derive a cutoff value of total calcium score for prediction of PAD, the projected total calcium score >149.1 was evolved as a cutoff with 100% sensitivity and 100% specificity for PAD. Abnormal calcium scoring (cutoff >149.1) was seen in 42 (76.4%) cases, as shown in Table 5. On comparing it against DECT angiographic findings, it was found to detect all the positive and negative cases correctly. There were no false-positive or false-negative cases, thus calcium scoring could be projected to have 100% sensitivity and 100% specificity for the detection of PAD.
| Calcium scoring | Total | Abnormal (n=42) |
Normal (n=13) |
|||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Abnormal | 42 | 76.4 | 42 | 100 | 0 | 0 |
| Normal | 13 | 23.6 | 0 | 0 | 13 | 100 |
χ2=55; P<0.001
On receiver-operator characteristic curve analysis to derive a cutoff value of total calcium score for the prediction of atheromatous changes, the area, the projected total calcium score >842.2 was evolved as a cutoff with projected sensitivity and specificity of 75.9% and 80.8% for the prediction of atheromatous changes. Using calcium scoring cutoff value derived by ROC analysis, calcium scoring detected 27 (49.1%) cases to have atheromatous changes, as shown in Table 6. The proportion of calcium scoring detected atheromatous changes was significantly higher among those having DECT detected atheromatous changes (75.9%) as compared to those having normal DECT for atheromatous changes (19.2%) (P < 0.001). The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of calcium scoring for detection of atheromatous changes were 75.9%, 80.8%, 81.5%, 75%, and 78.2%, respectively.
| Calcium scoring | Total | DECT athero (n=29) |
DECT normal (n=26) |
|||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| >842.20 | 27 | 49.1 | 22 | 75.9 | 5 | 19.2 |
| <842.20 | 28 | 50.9 | 7 | 24.1 | 21 | 80.8 |
χ2=22.22; P<0.001. DECT: Dual-energy computed tomography
DISCUSSION
In our study, DECT angiography confirmed peripheral artery disease of lower extremity in 42 out of 55 (76.4%) of clinically suspect cases and majority (69%) showed atheromatous changes while remaining 31% showed narrowing of vessels. Contrary to this, Osama et al.[10] in their study showed atheromatous changes in 46.3% of cases only. The reason for the lower prevalence of atheromatous changes in their study could be attributable to the inclusion of patients at a lower risk of PAD as reflected by the lower prevalence of PAD in their study.
As compared to CT angiography assessment, Doppler assessment was 88.1% sensitive but only 69.2% specific. It had a true positive value of 90.2% and a true negative value of 64.3%. The accuracy of Doppler assessment was 83.6%. Although color Doppler is considered to be an initial imaging tool for the detection of PAD, yet it lacks adequate sensitivity as well as specificity. The findings of the present study were similar to those observed by Parikh et al.[11] who found the sensitivity of color Doppler to be ranging from 75 to 95%.
DECT detected atheromatous changes in 29 (52.7%) cases; however, color Doppler assessed atheromatous changes in 31 (56.4%) cases. However, there was an agreement with CTA in only 24/29 (86.2%) cases, thus showing that color Doppler had a sensitivity of 86.2% and specificity of 76.9% in detection of atheromatous changes. These findings are in agreement with the observations of Dev et al.[12] and Peedikayil et al.[13] who also found that USG has lower sensitivity and specificity as compared to CTA in detection of luminal narrowing, irregularity, calcification, and atheromatous changes.
Mean calcium scores for different arteries ranged from 183.95 ± 314.36 (iliac right) to 351.27 ± 272.46 (calf right) among cases with abnormal angiographic findings, whereas among those with normal angiographic findings, they ranged from 0 (iliac left and right and calf right and left) to 17.63 ± 33.50 (thigh left). The total calcium score was 1515.1 ± 1198.3 in patients with abnormal angiographic findings as compared to 30.18 ± 57.36 among those with normal angiographic findings. Calcification can be considered to be an integral part of the pathogenesis of atherosclerosis which might be associated with luminal obstruction, a decrease in arterial vessel wall elasticity could ultimately lead to atherosclerosis, reduced perfusion, and eventually, coronary artery disease and PAD.[14] Findings of the present study showed that in four out of six arteries, there was no calcification in cases where CTA did not diagnose PAD while in remaining two locations (right and left thigh), the mean calcification scores among those without PAD were almost 10–15 times lower as compared to those having PAD. These findings in effect show the essential role of calcification in causing atherosclerosis and narrowing of lumens and showed that calcification can be marked as a precursor to PAD. Consecutively, we derived total calcium scores and derived a cutoff value for differentiation between PAD and non-PAD cases. The derived cutoff value >149.1 was in 100% agreement with CTA detected PAD. Calcification is considered to be more widespread in the lower abdominal region, associated with PAD.[15-17] Findings of the present study showed that their measurement could be helpful in diagnosing the PAD.
As far as atheromatous changes are concerned, in the present study, we found mean total calcium scores to be significantly higher among those in whom CTA detected atheromatous changes, thus establishing a cause-effect relationship between calcification and atheromatous changes. Calcification, being a precursor to atherosclerosis, could itself be considered as a more sensitive criterion for tagging atheromatous changes, however, when CTA was considered as the gold standard, we found that total calcium score at a cutoff value of >842.2 had sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of 75.9%, 80.8%, 81.5%, 75%, and 78.2%, respectively, for the detection of atheromatous changes. Considering the fact that, no previous study has evaluated such association so far, we cannot comment over the empirical findings on this issue. However, given the conceptual role of calcification as a precursor to atherosclerosis/atheromatous changes, we are of the view that cutoff value of calcium scores for detecting atheromatous changes could be done only through the help of prospective study. Further studies to evaluate the role of calcium scoring as a precursor for atheromatous changes are also recommended to establish its role as an early marker of vascular atherosclerosis.
There are few limitations in our study. Not all patients can undergo Doppler examination due to ulceration, pain, swelling, heavily calcified arteries, and obesity. Furthermore, the Doppler examination is time consuming and requires trained personnel and therefore becomes unsuitable for certain patients. As far as role of calcium scoring is concerned, none of the previous studies has limited its role for the diagnosis of PAD or identification of atheromatous changes. Most of the previous studies have evaluated its role as a prognostic factor for adverse events. Owing to limitations of time and inability to carry out a prospective study in which we could identify the role of calcium scores for futuristic adverse events that could prove its usefulness as an auxiliary measurement during CT angiography, remains to be seen. Considering this limitation, we recommend further studies on a larger sample size on clinically suspect cases of PAD in whom calcium scoring should be done at baseline and they should be followed up for the development of PAD in future, adverse cardiovascular event and amputation as the outcomes. Further studies to evaluate the role of calcium scoring as a precursor for atheromatous changes are also recommended to establish its role as an early marker of vascular atherosclerosis.
CONCLUSION
The present study assessed the usefulness of color Doppler and calcium scoring assessment in evaluation of PAD and compared them with dual-energy computed tomographic angiographic evaluation. The findings of the present study thus showed that calcium scoring as compared to color Doppler had a higher diagnostic efficacy for the detection of DECT angiography confirmed PAD and it can be helpful in diagnosing PAD. Concerning evaluation of atheromatous changes, though calcium score lacked adequate sensitivity at the projected cutoff, however, keeping in view the fact, that calcium score in itself is a reflection of atheromatous change, the evaluation of atheromatous changes using calcium scoring needs to be assessed in prospective longitudinal clinical studies where the calcium scoring should be correlated with prospective clinical outcome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Functional status and mobility among elderly women with lower extremity arterial disease: The study of osteoporotic fractures. J Am Geriatr Soc. 1994;42:923-9.
- [CrossRef] [PubMed] [Google Scholar]
- Noninvasive diagnostic strategies for peripheral arterial disease. Cleve Clin J Med. 2006;73(Suppl 4):S22-9.
- [CrossRef] [PubMed] [Google Scholar]
- CT angiography after 20 years: A transformation in cardiovascular disease characterization continues to advance. Radiology. 2014;271:633-52.
- [CrossRef] [PubMed] [Google Scholar]
- Pathogenesis of atherosclerosis. J Am Coll Cardiol. 2006;18:C7-12.
- [CrossRef] [PubMed] [Google Scholar]
- ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: A report of the American college of cardiology foundation clinical expert consensus task force (ACCF/AHA writing committee to update the 2000 expert consensus document on electron beam computed tomography) developed in collaboration with the society of atherosclerosis imaging and prevention and the society of cardiovascular computed tomography. J Am Coll Cardiol. 2007;49:378-402.
- [CrossRef] [PubMed] [Google Scholar]
- Association of lower extremity arterial calcification with amputation and mortality in patients with symptomatic peripheral artery disease. PLoS One. 2014;9:e90201.
- [CrossRef] [PubMed] [Google Scholar]
- Dual energy CT angiography of peripheral arterial disease: Feasibility of using lower contrast medium volume. PLoS One. 2015;10:e0139275.
- [CrossRef] [PubMed] [Google Scholar]
- Dual energy computed tomography angiography in the peripheral arterial imaging: A systematic review of image quality, radiation dose and diagnostic value. Curr Med Imaging Rev. 2017;13:66-72.
- [CrossRef] [Google Scholar]
- Role of multi-slice CT angiography versus Doppler ultrasonography and conventional angiography in assessment of aorto-iliac arterial disease. Egypt J Radiol Nucl Med. 2012;43:561-73.
- [CrossRef] [Google Scholar]
- Efficacy of color Doppler imaging over CT angiography in peripheral artery disease. J Integr Health Sci. 2017;5:45-52.
- [CrossRef] [Google Scholar]
- Comparative analysis of colour Doppler ultrasonography and CT angiography in peripheral arterial disease: Studying the effects of vessels wall calcification on diagnostic evaluation. J Clin Diagn Res. 2018;12:TC01-6.
- [CrossRef] [Google Scholar]
- Multidetetor CT angiography versus colour Doppler ultrasonography in the diagnosis of peripheral arterial diseases of lower extremities. J Evol Med Dent Sci. 2016;6:4457-61.
- [CrossRef] [Google Scholar]
- Peripheral arterial calcification: Prevalence, mechanism, detection and clinical implications. Catheter Cardiovasc Interv. 2014;83:E212-20.
- [CrossRef] [PubMed] [Google Scholar]
- Peripheral arterial disease: Morbidity and mortality implications. Circulation. 2006;114:688-99.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of and risk factors for peripheral arterial disease in the United States. Results from the national health and nutrition examination survery 1999-2000. Circulation. 2004;110:728-43.
- [CrossRef] [PubMed] [Google Scholar]
- Critical issues in peripheral arterial disease detection and management: A call to action. Arch Intern Med. 2003;163:884-92.
- [CrossRef] [PubMed] [Google Scholar]






