Translate this page into:
Dedicated Three-dimensional Breast Computed Tomography: Lesion Characteristic Perception by Radiologists
Address for correspondence: Dr. Cherie Marie Kuzmiak, Department of Radiology, University of North Carolina, Physicians Office Building, 170 Manning Drive, Room No. 118, Chapel Hill, NC 27599-7510, USA. E-mail: cherie_kuzmiak@med.unc.edu
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives:
To assess radiologist confidence in the characterization of suspicious breast lesions with a dedicated three-dimensional breast computed tomography (DBCT) system in comparison to diagnostic two-dimensional digital mammography (dxDM).
Materials and Methods:
Twenty women were recruited who were to undergo a breast biopsy for a Breast Imaging-Reporting and Data System (BI-RADS) 4 or 5 lesion evaluated with dxDM in this Institutional Review Board-approved study. The enrolled subjects underwent imaging of the breast(s) of concern using DBCT. Seven radiologists reviewed the cases. Each reader compared DBCT to the dxDM and was asked to specify the lesion type and BI-RADS score for each lesion and modality. They also compared lesion characteristics: Shape for masses or morphology for calcifications; and margins for masses or distribution for calcifications between the modalities using confidence scores (0–100).
Results:
Twenty-four biopsied lesions were included in this study: 17 (70.8%) masses and 7 (29.2%) calcifications. Eight (33.3%) lesions were malignant, and 16 (66.7%) were benign. Across all lesions, there was no significant difference in the margin/distribution (Δ = −0.99, P = 0.84) and shape/morphology (Δ = −0.10, P = 0.98) visualization confidence scores of DBCT in relation to dxDM. However, analysis by lesion type showed a statistically significant increase in reader shape (Δ =11.34, P = 0.013) and margin (Δ =9.93, P = 0.023) visualization confidence with DBCT versus dxDM for masses and significant decrease in reader morphology (Δ = −29.95, P = 0.001) and distribution (Δ = −28.62, P = 0.002) visualization confidence for calcifications.
Conclusion:
Reader confidence in the characterization of suspicious masses is significantly improved with DBCT, but reduced for calcifications. Further study is needed to determine whether this technology can be used for breast cancer screening.
Keywords
Breast cancer
computed tomography
diagnostic imaging
mammography
INTRODUCTION

Breast cancer is the most common female cancer, except for skin cancer, in the United States for every major ethnic group and the second most common cause of cancer death in women.[1] Mammography continues to be the Gold Standard of screening women for breast cancer.[234] Even with the development of full-field digital mammography, the main limitation of mammography is its decreased sensitivity in women with dense breast tissue.[234567] Dense breast tissue is present in 40-60% of all women.[8910]
In reaction to this limitation, researchers have been investigating digital breast tomosynthesis (DBT).[11121314151617] Published literature has demonstrated that DBT in combination with a conventional digital mammogram has demonstrated improved mass detection, decreased recall rates, and increased cancer detection.[1112131415] However, DBT has not eliminated mammographic breast compression.
Dedicated breast computed tomography (DBCT) is a new imaging modality that provides three-dimensional (3D) data that can be reconstructed into multiple imaging planes. DBCT can be performed without breast compression and is not limited by breast density.[18192021] The radiation dose level of DBCT is similar to the dose of a conventional two-view mammogram.[171819202122] There is limited published data on DBCT breast lesion conspicuity and no published data on radiologist reader lesion confidence in clinical trials.[1920212223] Therefore, the objective of our study is to assess radiologist confidence in the characterization of suspicious breast lesions in a population of women going to biopsy with a DBCT system in comparison to diagnostic two-dimensional (2D) full-field digital mammography (dxDM).
MATERIALS AND METHODS
Subjects
The procedures followed in this study were in accordance with the ethical standards of our Institutional Review Board (IRB) and with the Helsinki Declaration of 1975, as revised in 2000. In our IRB approved and Health Insurance Portability and Accountability Act (HIPPA)-compliant study, all study subjects provided informed written consent after the nature of the study had been explained. In this prospective study, we recruited twenty consecutive women from our breast clinic who were scheduled to undergo a breast biopsy for a mammographically detected lesion that was evaluated with diagnostic 2D full-field digital mammography (dxDM) from January 1, 2011 to October 1, 2011. The inclusion criteria consisted of 40-year-old or older women, who were able to provide informed consent, had at least one detected mammographic abnormality that was confirmed as a Breast Imaging-Reporting and Data System (BI-RADS®) assessment category 4 or 5 lesion after completion of diagnostic workup, and who were scheduled to undergo a core needle biopsy at our institution.[24] Women were not eligible for this study if they were under 40 years of age, weighed >350 pounds, were pregnant or lactating, had no mammographically evident lesion, or had a preexisting back, neck, shoulder, or general mobility difficulties. The enrolled subjects could have any breast composition category. After the DBCT imaging was complete, each subject was given a questionnaire to complete in order to evaluate her comfort level during DBCT imaging to that of other breast imaging scans on a continuous scale of 1 (much more comfortable) to 5 (much less comfortable).
Dedicated breast computed tomography scanner
The DBCT scans were performed using a prototype cone-beam DBCT system designed and developed by ZumaTek, Inc. (Research Triangle Park, NC, USA). The system uses an ergonomically designed bed where the subject scanned lies prone, which is shown in Figure 1. The head of the scan bed consists of a custom formed patient support that allows for full breast and chest wall access while maximizing subject comfort and consequently, minimizing subject motion. The design of the scan bed allows one breast to be imaged at a time. The diameter of the patient table opening allows for a cylindrical imaging volume of 20 cm in diameter × 20 cm in height or 6283 cm3. The breast to be imaged is noncompressed and hangs pendant through the opening of the table in the imaging field below the scan bed, as denoted by the arrow in Figure 1. In addition, there are radiation shielded panels all around the bed that can be opened below the head of the scanning bed that can allow the imaging technologist direct visualization if further positioning of the subject as needed. Besides direct visualization, there is also a laser site that can aid with positioning. There is an enclosure containing the imaging hardware also beneath the bed.
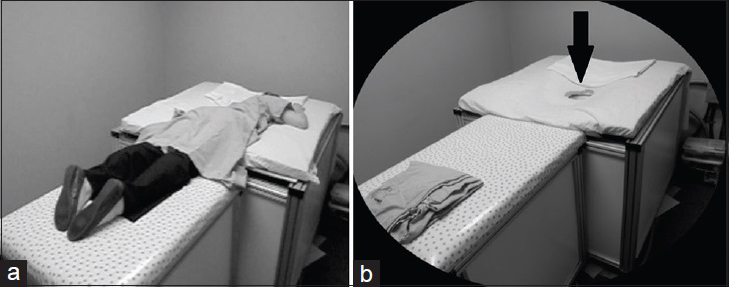
- Three-dimensional dedicated breast computed tomography prototype system. (a) Ergonomically designed bed where the subject scanned lies prone. (b) The noncompressed breast to be imaged hangs pendant through the opening of the table (arrow) below the scan bed.
This cone-beam CT system features a single 30 cm × 30 cm, amorphous silicon flat-panel, digital detector with a Thallium-doped Cesium Iodide scintillator (PaxScan® 3030, Varian Medical Systems, Palo Alto, California, USA). The detector has 197-micron pixels, which can be binned in 2 × 2 or read out in 1 × 1 mode. The pixel depth is 14-bits. The system uses a rotating tungsten rotating anode (RAD-70B, Varian Medical Systems, Palo Alto, California, USA) with a tungsten filter. The nominal focal spot size is 0.3 mm. The tube is capable of an output to 49 kVp. The DBCT system is powered by a high-frequency X-ray generator (SEDECAL, Madrid, Spain), which allows for fast pulsed X-ray generation up to 30 frames per second. The X-ray tube and detector are fixed at a specific source-to-image distance of 70 cm; therefore, there is no contact with the breast being imaged. The scanner operates in step and shoot mode whereby it is preprogrammed to move and stop at 300 specific positions around the noncompressed, pendant breast as individual images are taken. The scan time for one breast is 1 min 40 s. The average radiation dose is <4.5 mGy for a bilateral DBCT scan.[21]
Motors in the system provide motion to allow the imaging components to be moved about a full 360° vertical rotation axis, and also 60° horizontal pivoting about the rotation axis is achieved around the noncompressed breast being imaged. This unique 3D orbiting capability allows for full breast and chest wall access with more complete cone beam sampling throughout the image volume.[21] In addition to a horizontal rotation, the system is also able to tilt. This is necessary in order to remove cone beam distortion artifacts. A third motion is possible to allow the system to be moved vertically up and down to position the system optimally below the bed.
At the end of the scan, the 300 images obtained for each breast are sent to a computer processing workstation and are automatically processed with an iterative reconstruction algorithm that reconstructs (768 × 768 × 14 bits/projection) the images into a 3D DBCT dataset. The measured isotropic reconstructed pixels are 197 microns, and the measured reconstructed resolution of the line pairs with a 20 cm diameter Catphan phantom (Phantom Laboratory, Salem, NY, USA) is 2.5 line pairs per millimeter. Prior to the reconstruction, motion correction software may be utilized. The resulting Digital Imaging and Communication in Medicine (DICOM) compliant images were viewed using ClearCanvas software (ClearCanvas, Toronto, Ontario, Canada). The DBCT data was displayed in three simultaneous imaging planes (coronal, sagittal, and axial planes), Figure 2. In addition, the slice thickness and other viewing features, such as window and leveling, could be adjusted on the viewing workstation.
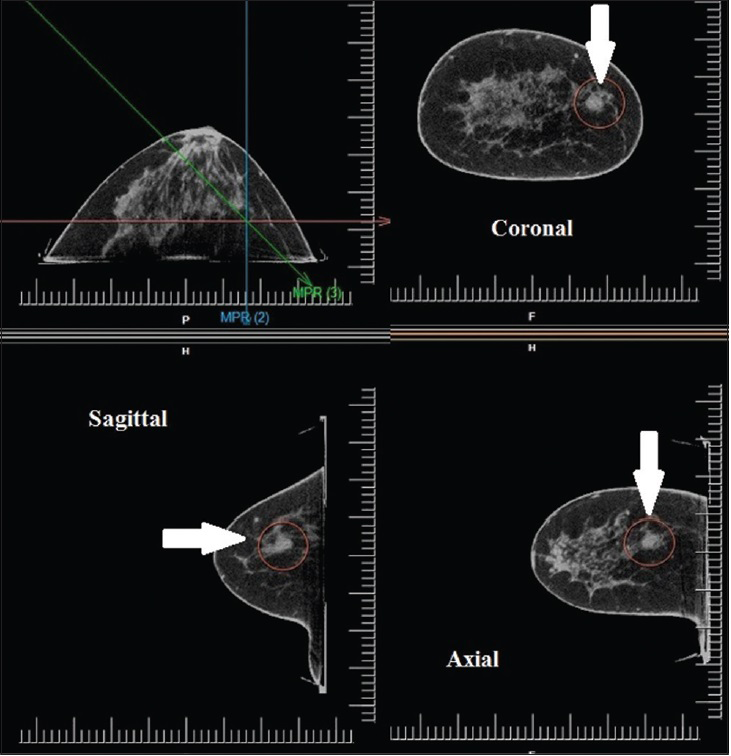
- 54-year-old women with a mass in the medial right breast diagnosed with a fibroadenoma. Dedicated breast computed tomography images viewed as three-dimensional data sets in multiple imaging planes (coronal, sagittal and axial planes) on a softcopy workstation demonstrate a 1 cm, oval, predominately circumscribed, noncalcified mass (arrow).
Training and start up
The principal investigator (PI) and the research technologist, certified in mammography, were both trained on the 3D DBCT system and workstation by application and technical supervising personnel from ZumaTek, Inc., including how to use, acquire and transmit the DBCT images. For training purposes in this internal IRB approved and HIPPA-compliant study, five healthy volunteers were recruited prior to study accrual. The healthy volunteers had to be at least 40 years old, able to provide informed consent, and had a normal current (<60 days) mammogram. A healthy volunteer was excluded if she was <40 years of age, weighed >350 pounds, pregnant or lactating, had preexisting back, neck, shoulder, or general mobility difficulties, and did not have a mammogram within 60 days or the recent mammogram study was abnormal. All of the healthy volunteers provided informed consent. If the healthy volunteer was of childbearing age and not surgically sterile, a urine pregnancy test was performed to exclude the possibility of pregnancy prior to DBCT imaging. The healthy volunteers underwent bilateral imaging with the DBCT system only to test the operation of the system, to make any necessary adjustments to the system, and to train the technologist who operated the system. Images of all healthy volunteers were reviewed jointly by our study investigators and sponsor quality control personnel to review image quality.
Image acquisition
Eligible subjects were identified by research staff review of the clinical reports of women who were scheduled for at least one image-guided needle core breast biopsy. All diagnostic 2D digital mammographic images (dxDM) with additional magnification views as clinically needed (Senographe Essential, General Electric Medical, Milwaukee, WI, USA) of all the eligible subjects were reviewed by the PI of the study prior to contacting potential subjects to ensure that the lesion recommended for biopsy was visualized on the dxDM exam.
All eligible women who agreed to participate in the study were asked to come to our imaging research laboratory prior to their scheduled biopsy appointment to complete the informed consent process and to undergo the study DBCT scan. For subjects of childbearing age, a negative urine pregnancy test was required prior to enrollment. The enrolled subjects subsequently underwent imaging of the breast(s) recommended for biopsy using the DBCT system.
The subjects were imaged in the prone position. One breast at a time was placed in the table opening near the head of the table, and the noncompressed breast was allowed to hang pendant for the scan in the imaging field of view. Prior to starting the scan, the technologist confirmed that the subject's breast to be imaged was centered in the device from below the table. The technologist then closed the observation panels, asked the subject to relax and remain still, and commenced with the DBCT scan. The actual scan time was 1 min 40 s per breast. During imaging, the patient was allowed to breathe normally. If the patient had a qualifying lesion in the contralateral breast that breast was also positioned and scanned in the same manner. The procedure to scan the opposite breast was performed without the subject having to leave the scanning bed. Once DBCT imaging was finished, the study procedure was complete. The DBCT images were reviewed by the PI of the study and research technologist to ensure image quality. Afterward, the enrolled study subjects were asked to complete a questionnaire about the comfort of the DBCT machine.
Postimaging
Subsequently, the breast biopsy took place as clinically indicated. The research DBCT exam was not interpreted prior to the conductance of the breast biopsy and, therefore, did not influence clinical decision-making.
Data submission
The research technologist electronically submitted to our medical imaging laboratory all de-identified clinical report forms as well as the de-identified breast CT exams, mammograms, breast ultrasounds (if available), and breast magnetic resonance imaging (MRI) (if available) of all eligible enrolled subjects that were obtained and contributed to the ultimate diagnosis leading to biopsy. The transmitted de-identified data were reviewed and correlated with the imaging findings, entered, and prepared for inclusion in the reader study.
Reader study
A reader study was conducted after the completion of patient accrual to the study to compare the visibility of lesion characteristics with the DBCT compared to 2D full-field digital screening mammography and diagnostic mammography images. Seven breast imaging radiologists reviewed the cases in the reader study. For training purposes, each radiologist was initially presented with four cases in order to become familiar with the workstation design, image display, and lesion examples. The training cases consisted of a mixture of benign and malignant cases with different lesion types with lesion descriptors. The study cases were presented in random order for each reader. The breast lesions were annotated on all images of each case for each modality for the readers by the PI of the study. The DBCT data was displayed in coronal, sagittal, and axial planes, and the dxDM data were displayed on dedicated workstations. The radiologists were allowed to roam, zoom, window, and level all the images in either modality if desired. In addition, the viewing software for DBCT allowed the radiologist to adjust slice thickness of the images and multi-intensity projection images could also be used as part of the software display for interpretation.
The study consisted of the DBCT and mammography exams presented side-by-side for a given case. All lesions in this study regardless of lesion type were visible on both modalities. Each reader was asked to compare side-by-side the DBCT exam to the dxDM exam including the lesion recommended for biopsy. Each reader was asked to specify the lesion type and BI-RADS® assessment category for each lesion for each modality and to compare the lesion characteristics: Shape for masses or morphology for calcifications and margins for masses or distribution for calcifications between the two modalities using confidence scores (0–100). The specific descriptors that were used for lesion characteristics were consistent with the BI-RADS® mammography lexicon and were used consistently amongst the readers.[24]
Statistical analysis
Statistical analysis was performed with SAS statistical software, version PC 9.2 (SAS Institute, Inc., Cary, NC, USA). The average confidence scores of each modality over the seven readers for each condition were calculated, and a linear mixed effects model was used to analyze the data. A random intercept was used in the model to account for the correlation among readers when reading the images from the same subject. The Wald's test, based on the model fit, was used to test whether the grand mean parameter was larger than zero. P < 0.05 was considered to indicate statistically significant differences.
RESULTS
There were a total of 24 biopsied lesions in 20 subjects included in this study.
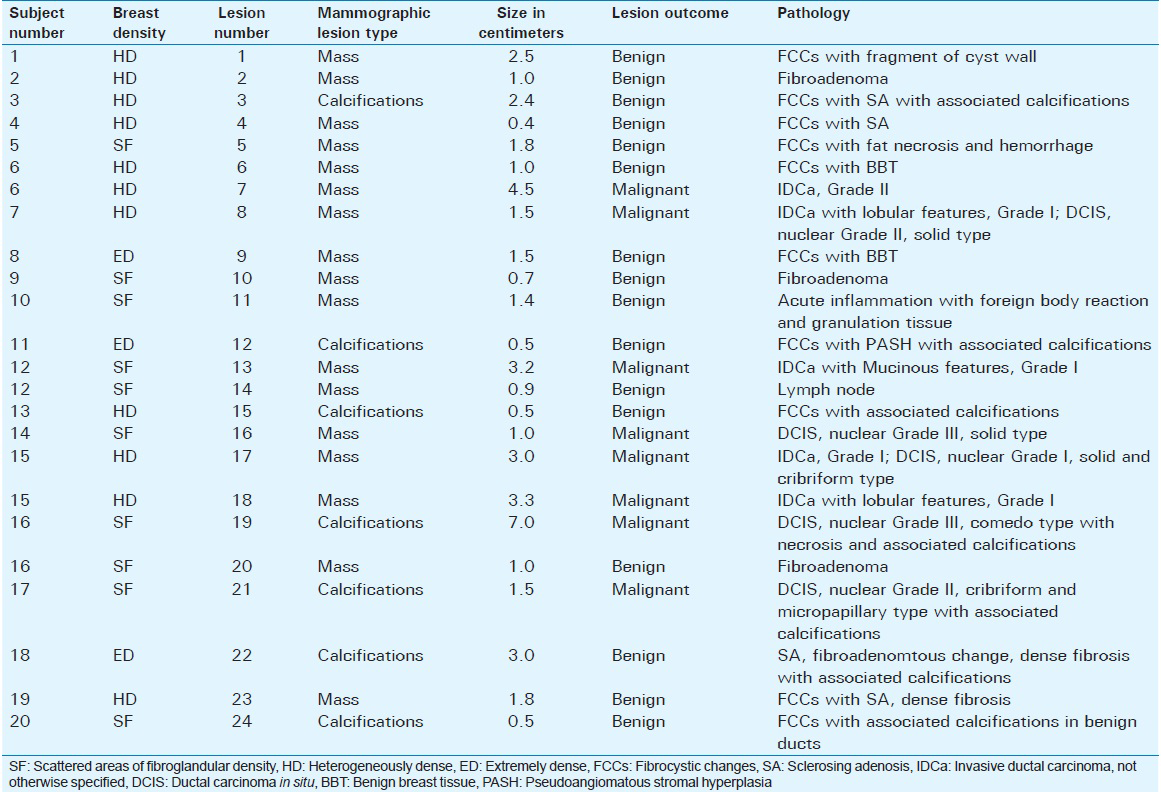
Each patient underwent percutaneous biopsy, and the pathology reports were reviewed and correlated with the imaging findings. The mammographic findings of the biopsied lesions consisted of 17 (70.8%) masses and 7 (29.2%) calcifications. Overall, 8 (28.6%) lesions were malignant, and 16 (71.4%) were benign. Six (75.0%) of the malignant lesions (5 invasive cancers and 1 ductal carcinoma in situ [DCIS]) were presented as masses. Only 2 (28.6%) of the 7 cases of calcifications were malignant, both DCIS. The mean size of a malignant mass case and a malignant calcification case was 2.8 cm (range 1.0–4.5 cm) and 4.3 cm (range 1.5–7.0 cm), respectively. The mean size of a benign mass case was 1.5 cm (range 0.4–2.5 cm), and the mean size of a benign calcification case was 1.8 cm (range 0.5–3.0 cm). Mammographic lesion type, size, and pathology are listed in Table 1.
Three (15%) subjects had bilateral lesions and 1 (5.0%) subject had 2 lesions in the same breast. Of the 3 subjects with bilateral lesions, 1 (33.3%) subject had bilateral invasive cancer, and the other 2 (66.7%) subjects had unilateral cancer (1 case invasive and 1 case DCIS) with a contralateral benign lesion. The one (5.0%) subject with 2 lesions in the same breast had both a malignant lesion (DCIS) and a benign lesion (fibroadenoma). With regard to breast side of the lesion, 10 (41.7%) were located in the right breast, and 14 (58.3%) were located in the left breast. Three (37.5%) malignant lesions were located in the right breast, and 5 (62.5%) were located in the left breast.
The 20 subjects enrolled and imaged in the study consisted of 12 (60.0%) Caucasian and 8 (40.0%) African American women with a mean age of 58.0 years (range 41–75 years). The mean age of a subject with a malignant lesion was 56.5 years and the mean age of a subject with a benign lesion was 58.0 years. Six (30.0%) of the subjects had a history of a benign biopsy: 3 (50.0%) core needle biopsy and 3 (50.0%) open surgical excision. One (5.0%) subject had a prior breast cancer history of DCIS that had been treated with a mastectomy. None of the subjects had a family history of breast cancer.
The BI-RADS® mammographic breast composition categories for the enrolled subjects were 8 (40.0%) with scattered areas of fibroglandular density, 9 (45.0%) with heterogeneously dense, and 3 (15.0%) with extremely dense breasts, Table 1. When the latter two categories are combined, 60.0% of the cases were in subjects with dense breast tissue. None of the subjects had almost entirely fatty breast composition. For the 7 (35.0%) subjects diagnosed with at least 1 cancer (1 subject had a bilateral invasive cancer), the BI-RADS® mammographic breast composition categories were 3 (42.9%) with scattered areas of fibroglandular density, 3 (42.9%) heterogeneously dense, and 1 (14.2%) with extremely dense breasts. The one (14.3%) subject with the bilateral breast cancer had heterogeneously dense breasts. The two (28.6%) subjects that had cancer (DCIS) present as calcifications had the mammographic breast composition of scattered areas of fibroglandular density. For the 13 (65.0%) subjects with benign only pathology, 5 (38.5%) had scattered areas of fibroglandular density, 6 (46.2%) had heterogeneously dense breasts, and 2 (15.3%) had extremely dense breasts mammographically.
A total of seven radiologists reviewed the cases in a reader's study. All radiologists were fellowship trained in breast imaging. Their mean years of experience interpreting mammography was 8 (range 3–14 years). All radiologists were certified by the American Board of Radiology and met accreditation standards mandated by the Mammography Quality Standard Act and Program. None of the radiologists had prior DBCT research experience or clinical experience in interpretation of DBCT.
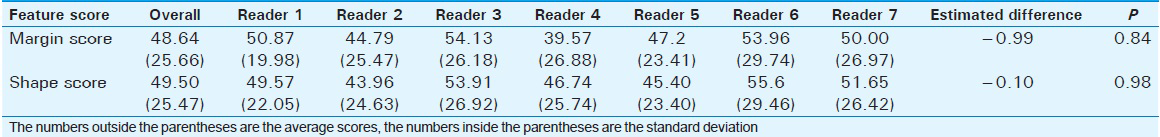
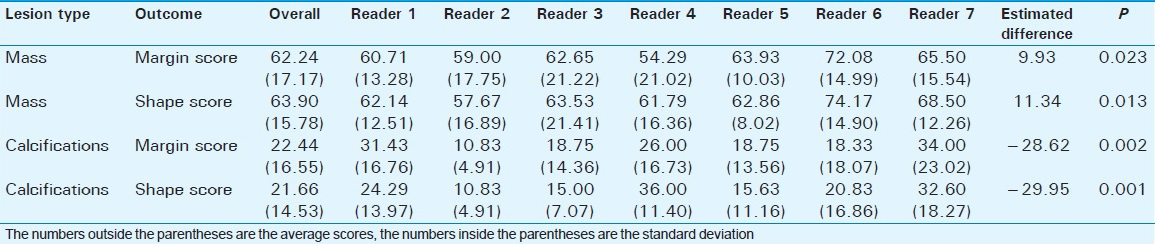
Mean confidence radiologist reader scores of DBCT compared to dxDM for the two conditions for all lesions regardless of lesion type, lesion pathology, and subject breast density are shown in Table 2. Across all lesions, there was no significant difference in the margin/distribution (Δ = −0.99, P = 0.84) and shape/morphology (Δ = −0.10, P = 0.98) visualization confidence scores of CT in relation to dxDM. However, analysis by lesion type showed a statistically significant increase in reader shape (Δ =11.34, P = 0.013) and margin (Δ =9.93, P = 0.023) visualization confidence with CT versus dxDM for masses and significant decrease in reader morphology (Δ = −29.95, P = 0.001) and distribution (Δ = −28.62, P = 0.002) visualization confidence for calcifications, Table 3. The reader visualization confidence scores of benign and malignant lesions between the two modalities for subjects with dense breast tissue were not significantly different (P > 0.1). There was no significant difference (P > 0.1) between the two modalities in the readers’ BI-RADS assessment scores across all lesions, regardless of size or final pathology or subject breast density. Examples of a benign and a malignant mass with mammographic and DBCT correlation images are shown in Figures 3 and 4, respectively. In addition, mammographic and DBT correlation images for benign and malignant calcifications cases are demonstrated in Figures 5 and 6.
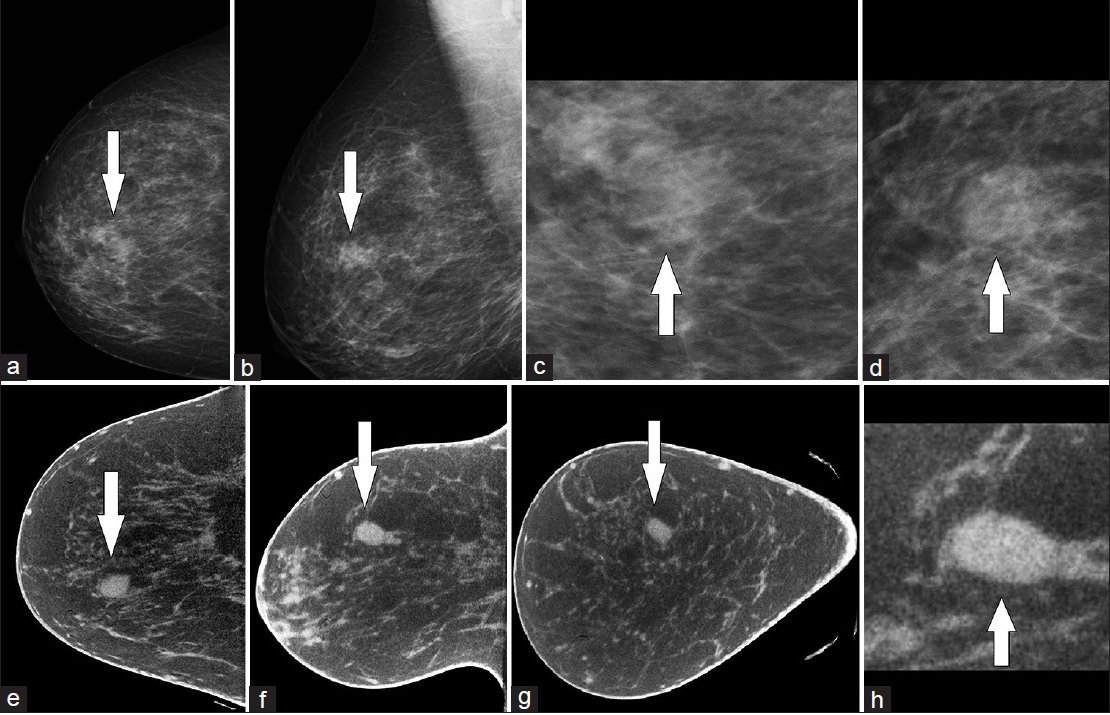
- 49-year-old women with a mass in the medial right breast diagnosed with a fibroadenoma. Mammographic images of the right breast: (a) craniocaudal, (b) mediolateral oblique, (c) spot compression magnification craniocaudal view, (d) spot compression magnification mediolateral oblique view. The mammographic images demonstrate a 1 cm, oval, obscured mass (arrow) in the upper inner quadrant. Dedicated breast computed tomography slice images of the right breast: (e) axial, (f) sagittal, (g) coronal, (h) enlarged sagittal image. The dedicated breast computed tomography images of the mass (arrow) show a circumscribed margin since there is no overlap of breast tissue.
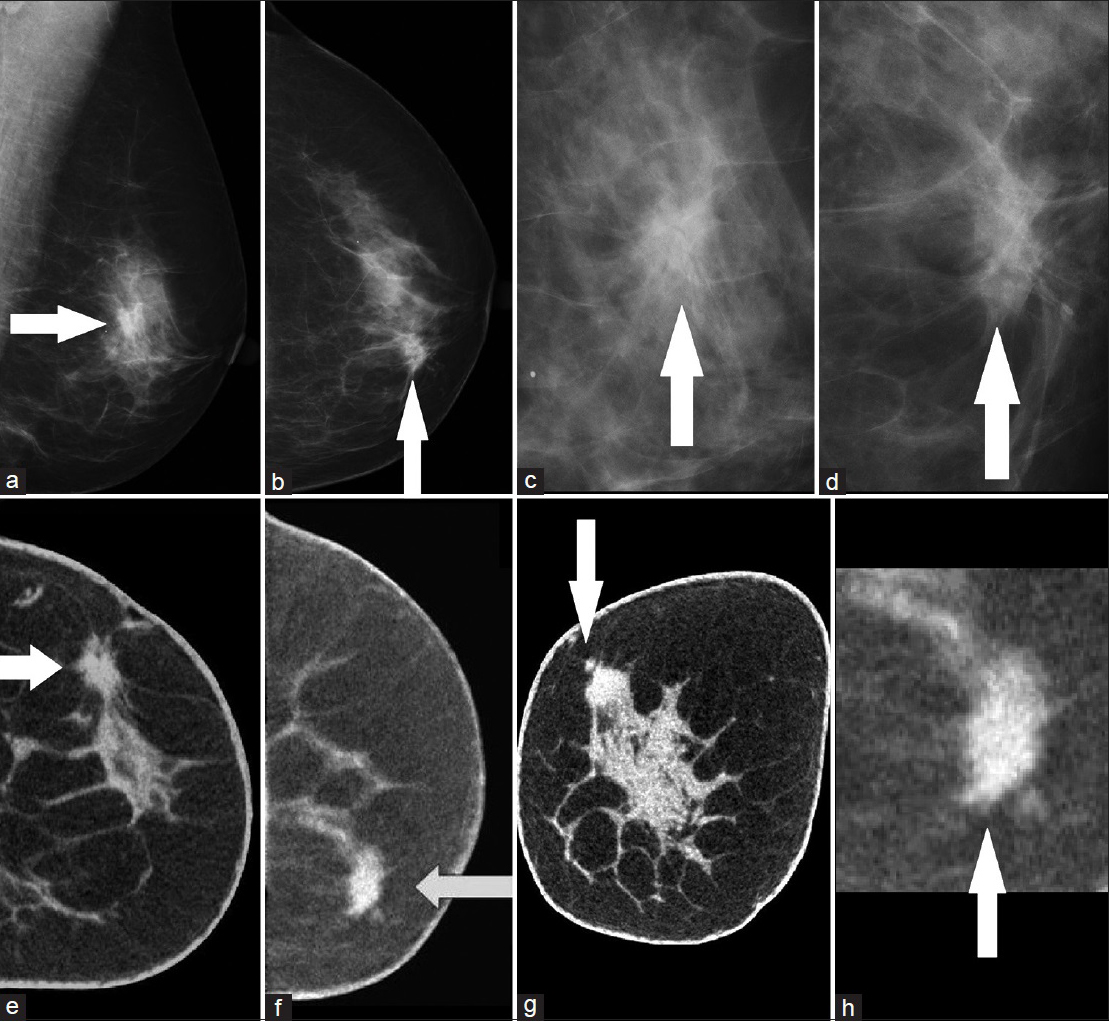
- 72-year-old women with a mass in the medial left breast diagnosed with invasive ductal carcinoma. Mammographic images of the left breast: (a) mediolateral oblique, (b) craniocaudal, (c) spot compression magnification mediolateral oblique view, (d) spot compression magnification craniocaudal view. The mammographic images show a 1.5 cm, irregular, partially obscured mass (arrow) in the medial aspect. Dedicated breast computed tomography slice images of the left breast: (e) sagittal, (f) axial, (g) coronal, (h) enlarged axial image. The dedicated breast computed tomography images of the mass (arrow) demonstrate that the margins of the mass to be spiculated.
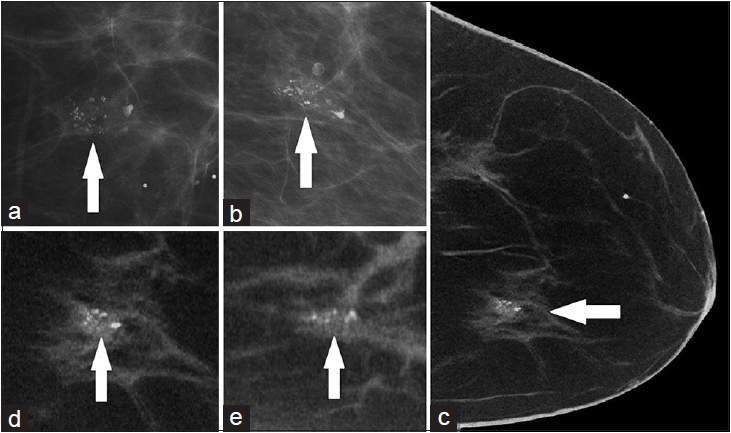
- 48-year-old women with grouped calcifications in the medial left breast diagnosed with fibrocystic changes with associated calcifications. Mammographic images of the left breast: (a) spot compression magnification craniocaudal view, (b) 90° spot compression magnification view. The mammographic images demonstrate 1.5 cm, grouped, coarse heterogeneous and round calcifications (arrow). Dedicated breast computed tomography slice images: (c) axial image, (d) enlarged axial image, (e) enlarged sagittal image. The dedicated breast computed tomography images of the calcifications (arrow) demonstrate a similar appearance as the mammographic images.
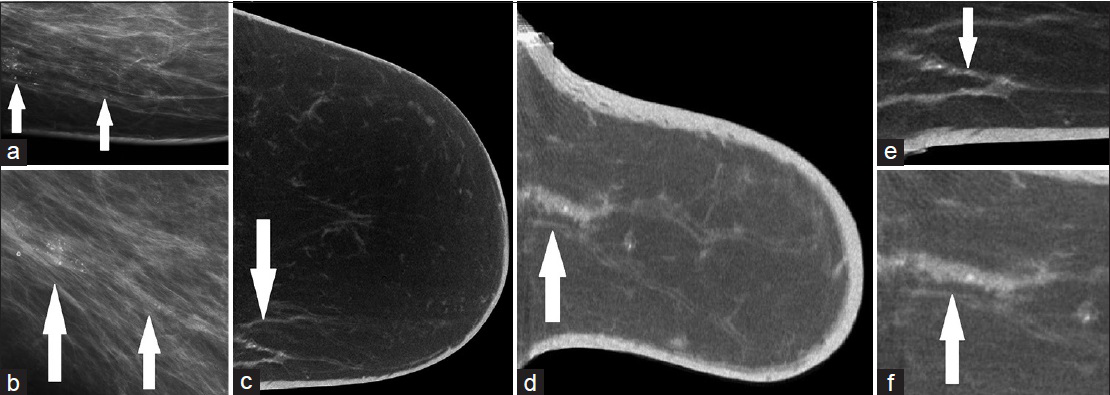
- 60-year-old women with calcifications in the medial left breast diagnosed with ductal carcinoma in situ. Mammographic images of the left breast: (a) spot compression magnification craniocaudal view, (b) 90° spot compression magnification view. The mammographic images show fine linear calcifications in a segmental distribution spanning 7 cm (arrow). Dedicated breast computed tomography slice images: (c) axial, (d) sagittal, (e) enlarged axial view, (f) enlarged sagittal view. The dedicated breast computed tomography images also demonstrate the same abnormal calcifications and distribution (arrow) as the mammographic images.
The total number of mammographic images was also recorded for this study. For the 20 subjects, the mean number of images obtained for each subject's diagnostic mammogram exam was 6 (range 2–10). Nine (45.0%) subjects initially underwent a diagnostic mammogram. For the 11 (55.0%) subjects that originally underwent a screening mammogram and were “recalled” for further diagnostic evaluation, the mean number of both mammographic exam images acquired were 10 (range 6–16). In contrast, only 1 DBCT scan was obtained per index breast per subject in this research study.
Results of the study subject questionnaire after completion of the DBCT portion of the study demonstrate that all 20 (100%) subjects were satisfied or very satisfied with the DBCT scan. Thirteen (65.0%) subjects reported no discomfort and 6 (30.0%) subjects reported minimal to mild discomfort during DBCT scanning. Only 1 (5.0%) subject reported moderate discomfort during the DBCT scanning. All discomfort that was reported was related to neck, back, or abdomen from the scanning table or arm positioning. In regard to scanning time and noise level of the DBCT device, 19 (95.0%) and 19 (95.0%) of the subjects were satisfied or very satisfied, respectively.
Questionnaire results of subject comfort of a DBCT scan versus a mammogram, handheld breast ultrasound (HHBUS), and contrast enhanced-MRI (CE-MRI) of the breasts were also collected. All 20 (100%) of the subjects reported the DBCT scan to be more comfortable than a mammogram. Sixty-five percent (13 subjects) reported the DBCT scan was more comfortable than HHBUS. Thirty-five percent (7 subjects) reported the DBCT scan and HHBUS to be equal in comfort. One (5%) subject reported the DBCT scan was less comfortable than a CE-MRI, and one (5%) subject reported the DBCT scan and the CE-MRI to be equal in comfort.
DISCUSSION
Our initial clinical experience with a prototype 3D DBCT system demonstrates that overall radiologist reader confidence in the characterization of suspicious lesions recommended for biopsy is similar to that of diagnostic 2D digital mammography. Radiologists were significantly more confident in mass shape and margin characterization on DBCT images compared to 2D digital diagnostic mammography. Even though all calcification lesions were visible on the DBCT, reader confidence in calcification lesion characteristics was significantly less than diagnostic mammography, and this may have been related to our prototype DBCT system. The DBCT system used 197-micron pixels in contrast to digital mammography that may have pixel sizes between 50 and 100 microns depending on the manufacturer. Our study used a digital mammography system with 100-micron pixels in addition to a magnification factor of ×1.8 for the spot compression magnification views. Thus, improvements in DBCT detector resolution and specific postprocessing algorithms could help radiologists improve calcification characterization.
The increase in reader confidence with masses on DBCT is most likely the result of DBCT's 3D imaging capability. With 3D imaging of the breast, DBCT has the advantage of being able to remove tissue overlap (masking) through the use of tomographic slice sections. In addition, the acquired image data obtained by DBCT is used to reconstruct a volume dataset for image display and can provide further diagnostic information for the radiologist. Since DBCT is true 3D imaging and does not require breast compression, it allows for registered orthogonal views of the breast in any projection for viewing, similar to MRI of the breast. The viewing software allows the radiologist to review images and lesions in multiple planes and adjust slice thickness of the images for interpretation. In addition, a multi-intensity projection image can also be visualized as part of the software display. Consequently, these advantages of DBCT may improve lesion characterization, which may aid in decreasing unnecessary biopsies and could possibly help in surgical planning in patients diagnosed with breast cancer.
The results of our study support the initial work by Lindfors et al., in which they evaluated BI-RADS® 4 and 5 lesions with their prototype DBCT system.[19] Their study consisted of 67 lesions: 52 (77.6%) masses, 12 (17.9%) calcifications, and 3 (4.5%) other types. However, 9 (13.4%) of 67 lesions in their study were not seen on DBCT. Overall, their results showed that breast CT was equal to screen film mammography for visualization of breast lesions. In addition, breast CT was significantly better than film-screen mammography for visualization of masses (P < 0.002) but film-screen mammography out-performed breast CT for visualization of calcifications (P < 0.006).[19] In contrast to their study, our subjects’ mammographic images were acquired with 2D full-field digital mammography, and we evaluated not only the reader confidence of lesion type but also confidence of lesion characteristics.
In the study by O’Connell and Kawakyu-O’Connor, two radiologists evaluated 36 patients with 37 abnormal mammographic and/or ultrasound categorized as BI-RADS® 4 or 5 lesions that were evaluated with their prototype DBCT system prior to biopsy.[22] Thirty-three (89.2%) of 37 breasts demonstrated a mammographic abnormality. Their results demonstrated a high degree of correlation between the DBCT and digital mammography across a variety of lesion types with 33 of 34 (97.1%) mammographic lesions being scored as equal or better visualized on breast CT relative to diagnostic mammography. Only one (2.9%) lesion in their study was not seen on DBCT and was attributed to be a mammographic summation shadow (22). Unlike their study criteria, all of our study lesions were visible with both diagnostic 2D digital mammography and DBCT. We did not include any lesions visible on sonography since we were comparing DBCT to diagnostic 2D digital mammography. In addition, our reader study included five more radiologists and also evaluated lesion features. The study by O’Connell et al., reported that 10.4% of their calcification findings were not seen on their prototype DBCT system.[20] All (100%) calcification lesions were visualized with DBCT in our study; however, radiologist confidence in calcification characterization was significantly better with digital diagnostic mammography.
3D DBCT may have several potential advantages compared to digital mammography in a diagnostic setting. The first advantage is radiation exposure during imaging. Currently, there is no maximum limit of breast radiation exposure with diagnostic mammography. Only screening 2D mammography and DBT have dose limits.[25] As with the prototype DBCT system we used, DBCT radiation doses similar to those with two-view mammography are being targeted.[18192021222325] The DBCT radiation dose is equivalent to about 2 months of natural background radiation exposure by a person in 1 year in the United States.[21] Comparable to mammographic doses, the radiation doses from DBCT are largely restricted to breast tissue.
The second advantage of the DBCT system is that the automated images of the uncompressed breast are obtained in a standardized manner with a short acquisition time. The DBCT scan time was 1 min 40 s in our study and was comparable to other published studies.[1920212223] Another benefit of our system is that due to the design of the imaging device even subjects with a large breast size (EE cup size) can be imaged without excluding breast tissue. Finally, DBCT is well tolerated. Our results support other studies in which higher degrees of subject comfort in the DBCT examination relative to mammography were reported.[19202122]
Limitations
There were some limitations to our study. First, none of the readers had prior research or clinical experience in interpretation of DBCT images. Another limitation was that only a small sample size of different lesion types was included in this single site study in which enrolled subjects had undergone a standard of care 2D digital mammographic diagnostic workup prior to being enrolled in this research study. None of the subjects had DBT since this was not available at our institution at the time of this study. Moreover, the resolution of the detector used on our prototype DBCT system was less than a full-field digital mammogram. Finally, our DBCT images were obtained without contrast but rather with a beam to optimize contrast differences between adipose and glandular tissues. The results of the study may have differed if the radiologists had DBCT experience, a larger sample size, DBT use, a prototype DBCT system with a finer spatial resolution and dedicated image processing algorithms and possibly the administration of intravenous contrast.[23] Nevertheless, future studies are needed in evaluating noncontrast DBCT versus contrast DBCT and DBT.
CONCLUSION
Dedicated 3D breast computed tomography is a novel well-tolerated imaging modality that allows for true isotropic, 3D imaging of the breast without mammographic compression. DBCT is comparable to conventional mammography in terms of radiation dose and overall lesion visibility. DBCT is superior in radiologists’ visualization and characterization of masses, but inferior to diagnostic mammography for calcifications. Its application could help eliminate the 2D mammographic limitation of overlapping tissue. Technical challenges remain, but 3D DBCT may have potential clinical applications in breast cancer screening and diagnosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This work has been funded by the National Cancer Institute of the National Institutes of Health (R44-CA125924) and in partnership with ZumaTek, Inc. at 2 Davis Dr, #116, Research Triangle Park, NC 27709.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2016/6/1/14/179428
REFERENCES
- American Cancer Society. Breast Cancer Statistics. Available from: http://www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-key-statistics
- [Google Scholar]
- National Evaluation Team for Breast Cancer Screening (NETB). Decreased rates of advanced breast cancer due to mammography screening in the Netherlands. Br J Cancer. 2004;91:861-7.
- [Google Scholar]
- Decreased breast cancer tumor size, stage, and mortality in Rhode Island: An example of a well-screened population. Cancer Control. 2004;11:222-30.
- [Google Scholar]
- Breast cancer mortality trends in the United States according to estrogen receptor status and age at diagnosis. J Clin Oncol. 2007;25:1683-90.
- [Google Scholar]
- Factors contributing to mammography failure in women aged 40-49 years. J Natl Cancer Inst. 2004;96:1432-40.
- [Google Scholar]
- Individual and combined effects of age, breast density, and hormone replacement therapy use on the accuracy of screening mammography. Ann Intern Med. 2003;138:168-75.
- [Google Scholar]
- Breast density as a predictor of mammographic detection: Comparison of interval- and screen-detected cancers. J Natl Cancer Inst. 2000;92:1081-7.
- [Google Scholar]
- Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med. 2005;353:1773-83.
- [Google Scholar]
- Wolfe mammographic parenchymal patterns. A study of the masking hypothesis of Egan and Mosteller. Cancer. 1985;56:1280-6.
- [Google Scholar]
- Analysis of parenchymal density on mammograms in 1353 women 25-79 years old. AJR Am J Roentgenol. 1996;167:1261-5.
- [Google Scholar]
- Breast cancer screening using tomosynthesis in combination with digital mammography. JAMA. 2014;311:2499-507.
- [Google Scholar]
- Comparison of digital mammography alone and digital mammography plus tomosynthesis in a population-based screening program. Radiology. 2013;267:47-56.
- [Google Scholar]
- Digital breast tomosynthesis versus digital mammography: A clinical performance study. Eur Radiol. 2010;20:1545-53.
- [Google Scholar]
- Comparison of tomosynthesis plus digital mammography and digital mammography alone for breast cancer screening. Radiology. 2013;269:694-700.
- [Google Scholar]
- Digital breast tomosynthesis in the diagnostic setting: Indications and clinical applications. Radiographics. 2015;35:975-90.
- [Google Scholar]
- Digital breast tomosynthesis: Lessons learned from early clinical implementation. Radiographics. 2014;34:E89-102.
- [Google Scholar]
- ACR Appropriateness Criteria. Radiation Dose Assessment. Available from: http://www.acr.org/~/media/ACR/Documents/AppCriteria/RadiationDoseAssessmentIntro.pdf.
- [Google Scholar]
- Dedicated breast CT: Radiation dose and image quality evaluation. Radiology. 2001;221:657-67.
- [Google Scholar]
- Cone-beam CT for breast imaging: Radiation dose, breast coverage, and image quality. AJR Am J Roentgenol. 2010;195:496-509.
- [Google Scholar]
- Development and initial demonstration of a low. dose dedicated fully 3D breast CT system. In: Maidment AD, Bakic PR, Gavenonis S, eds. IWDM 2012, LNCS. Vol 7361. Springer: Heidelberg; 2012. p. :442-9.
- [Google Scholar]
- Dedicated cone-beam breast computed tomography and diagnostic mammography: Comparison of radiation dose, patient comfort, and qualitative review of imaging findings in BI-RADS 4 and 5 lesions. J Clin Imaging Sci. 2012;2:7.
- [Google Scholar]
- Contrast-enhanced dedicated breast CT: Initial clinical experience. Radiology. 2010;256:714-23.
- [Google Scholar]
- Breast imaging reporting and data system, BI-RADS: Mammography. Reston, VA: American College of Radiology; 2013.
- [Google Scholar]
- Radiation doses and cancer risks from breast imaging studies. Radiology. 2010;257:246-53.
- [Google Scholar]






