Translate this page into:
Dedicated Cone-beam Breast Computed Tomography and Diagnostic Mammography: Comparison of Radiation Dose, Patient Comfort, And Qualitative Review of Imaging Findings in BI-RADS 4 and 5 Lesions
Address for correspondence: Dr. Avice M. O’Connell, Department of Imaging Sciences, University of Rochester Medical Center, Highland Breast Imaging Center, 500 Red Creek Drive, Rochester, NY 14623, USA. avice_oconnell@urmc.rochester.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
This pilot study was undertaken to compare radiation dose, relative visibility/conspicuity of biopsy-proven lesions, and relative patient comfort in diagnostic mammography and dedicated cone-beam breast computed tomography (CBBCT) in Breast Imaging-Reporting and Data System (BI-RADS)® 4 or 5 lesions.
Materials and Methods:
Thirty-six consecutive patients (37 breasts) with abnormal mammographic and/or ultrasound categorized as BI-RADS® 4 or 5 lesions were evaluated with CBBCT prior to biopsy. Administered radiation dose was calculated for each modality. Mammograms and CBBCT images were compared side-by-side and lesion visibility/conspicuity was qualitatively scored. Histopathology of lesions was reviewed. Patients were administered a survey for qualitative evaluation of comfort between the two modalities.
Results:
CBBCT dose was similar to or less than diagnostic mammography, with a mean dose of 9.4 mGy (±3.1 SD) for CBBCT vs. 16.9 mGy (±6.9 SD) for diagnostic mammography in a total of 37 imaged breasts (P<0.001). Thirty-three of 34 mammographic lesions were scored as equally or better visualized in CBBCT relative to diagnostic mammography. Characterization of high-risk lesions was excellent. Patients reported greater comfort in CBBCT imaging relative to mammography.
Conclusion:
Our experience of side-by-side comparison of CBBCT and diagnostic mammography in BI-RADS® 4 and 5 breast lesions demonstrated a high degree of correlation between the two modalities across a variety of lesion types. Owing to favorable radiation dose profile, excellent visualization of lesions, and qualitative benefits including improved patient comfort, excellent field-of-view, and more anatomical evaluation of lesion margins, CBBCT offers a promising modality for diagnostic evaluation of breast lesions.
Keywords
Breast CT
mammography
radiation dose
INTRODUCTION

Breast cancer is most commonly diagnosed nonskin cancer in women and represents the second leading cause of cancer death in women of all ages and the leading cause of cancer mortality in women between 20 and 59 years of age.[1] Early detection of breast cancer has been demonstrated to significantly decrease breast cancer mortality, even in women 40-49 years of age, despite the lower incidence of disease in younger cohorts.[2] Although the mortality benefits of early cancer detection by screening mammography are indisputable, quantitative and qualitative limitations of mammographic technique, including the large size of lesions at initial detection and challenges of resolving subtle soft-tissue changes suggestive of cancer, are well documented in the literature.[34]
In order to improve sensitivity and specificity of detecting and characterizing breast cancer, breast-specific imaging modalities are rapidly evolving. Technologies as varied as digital breast tomosynthesis[56] and molecular breast imaging techniques such as positron emission mammography[78] are presently under development, as are improvements in existing modalities such as ultrasound.[9] Cone-beam breast computed tomography (CBBCT) provides an additional imaging technique with a unique subset of advantages for diagnostic breast imaging.
Our initial experiences with CBBCT have been previously reported.[10] This study represents a continuation of our earlier investigation, now turning our attention to the imaging of biopsy-proven pathology in mammographic lesions with high probability of malignancy by accepted mammographic and/or sonographical criteria. All lesions in this study were categorized under the Breast Imaging Reporting and Data System (BI-RADS®) as category 4 or 5 lesions.[11]
In the present study, our minimum acceptable benchmark in terms of radiation dose and lesion visualization is diagnostic mammography. To this end, we defined three key areas of interest in evaluating CBBCT. Firstly, the radiation dose administered by the device and our protocol needs to be no greater than the dose from diagnostic mammography, the present standard of care in evaluation of lesions detected during screening mammography or clinically suspected in women over the age of 40. Secondly, as a roentgenographic technique, CBBCT must offer, at a minimum, equivalent visualization of lesions identified in standard-of-care diagnostic mammography. We did not limit our evaluation to mammographic lesions; however, several patients with similarly high-risk sonographical lesions not identified in diagnostic mammography were also included in our analysis. Thirdly, if CBBCT is to have a role in further evaluating mammographical lesions, it must be capable of providing additional advantages to the mammographer and the patient in the evaluation of breast disease to warrant continued development of a new technology. In addition to noting perceived advantages in the use of CBBCT in the evaluation of a variety of breast lesions in a range of breast compositions, we surveyed patients on the relative comfort of CBBCT relative to conventional mammography.
MATERIALS AND METHODS
Patients
This study was conducted at the University of Rochester Medical Center (URMC) - Highland Breast Imaging Center, Rochester, NY, from July 2006 to August 2008 under an IRB approved protocol with informed consent from each patient prior to CBBCT imaging and inclusion in this study.
This was a prospective study in which patients undergoing diagnostic breast imaging for abnormal screening mammograms or palpable breast abnormalities were invited to undergo CBBCT in addition to standard-of-care diagnostic mammography or ultrasound. Thirty-six consecutive subjects with ages ranging from 41 to 77-year old (mean, 56.0 yrs ± 9.8 SD) with BI-RADS® 4 or 5 findings on diagnostic mammography or ultrasound underwent CBBCT in addition to the standard additional diagnostic mammographic views, where appropriate. Most patients received CBBCT scan the same day as diagnostic mammography, and all were scanned within one week. Thirty-five (35) subjects had unilateral findings and one (1) had bilateral findings, resulting in a total of 37 breasts studied. A variety of breast densities (as defined by BI-RADS®) and types of mammographic and/or sonographic abnormalities were represented. The number and type of additional mammographic views and use of ultrasound varied according to the patient's presentation and screening findings. Each patient subsequently underwent percutaneous stereotactic or ultrasound-guided biopsy and the pathology reports were reviewed and correlated with the imaging findings.
CBBCT protocol
Images were obtained according to our standard CBBCT protocol, as previously reported.[10] In brief, the real time flat panel detector (FPD)-based CBBCT system consists of the following: A CT gantry (geometrically optimized for breast imaging), a special high-power mammography X-ray tube (with a 0.3-mm focal spot size) (Rad71SP, Varian Medical System, Salt Lake City, UT), an X-ray flat panel detector (FPD) (PaxScan 4030CB, Varian Medical System, Salt Lake City, UT) mounted on the gantry, an ergonomically designed patient table, and a personal computer (PC). The FPD is designed especially for cone-beam CT applications with a real-time dynamic gain mode with 0.388-mm pixel pitch (2×2 binning) and an image acquisition rate of 30 frames per second (fps). The panel has an inherent pixel depth of 14- bits that is extended to >16-bits in the dynamic gain mode.
The diameter of the patient table opening is 39 cm with a maximum imaging volume of 28 × 28 × 16 cm; various inserts are used to optimize patient comfort and positioning. The subject was placed on the imaging table in the prone position in a left or right anterior oblique position so that the targeted breast was suspended through the table opening into the image acquisition field with no external compression. A radiological technologist, registered in radiography and mammography through the American Registry of Radiologic Technologists (ARRT) and trained in CBBCT acquisition, positioned the subject using laser cross-hairs.
For a single continuous acquisition scan, the real time FPD-based prototype acquires 300 two-dimensional projection images (1024 × 768 × 14 bits/projection) by rotating the X-ray tube and the FPD 360° around the breast located at the rotation center in 10 seconds. X-ray pulses are 8 milliseconds in duration at 30 Hertz (Hz). A PC computer controls the operation of the prototype, including the gantry rotation, kVp, mA, X-ray pulse width, and projection data acquisition. The PCI-bus-based frame grabber is synchronized to the FPD and programmed to allow the image data to flow directly into memory for real–time data acquisition. Once all of the projection data are acquired from a single scan, the two-dimensional projection images are stored on the hard drive for subsequent image processing, 3D reconstruction, and visualization.
Reconstructed CBBCT matrices of the breast images were loaded into the specialized 3D visualization software (Visage CS Thin Client/Server, Visage Imaging, Carlsbad, CA) for 3D rendering, visualization, and display. The 3D reconstructed images can be visualized in three orthogonal planes (transverse, sagittal, and coronal) as well as with 3D rendering. CBBCT transverse and sagittal views correspond to the mammographical craniocaudal (CC) and mediolateral-oblique (MLO) views, respectively. The system also includes noise reduction (smoothing) software. Postacquisition image processing and reconstruction to achieve isotropic reconstructed volumes are performed with a soft tissue filter and (0.273 mm) 3 voxel size (standard mode). Regions with calcifications were reconstructed with the volume-of-interest higher resolution mode with a sharp ramp filter at (0.155 mm) 3 as a standard post-processing protocol.
Dose measurement and comparison
For each patient, we obtained dose measurements for both CBBCT and routine digital diagnostic mammography. The average glandular radiation dose (mGy) as a function of X-ray tube current (mA) [when voltage (kVp) and time (ms) are constant] was determined from prior dose phantom studies.[12] The mA-to-mGy relationship was verified using an FDA-approved 16-cm PMMA head dose phantom to measure the weighted computer tomography dose index (CTDIw).
CTDIw = 8 mGy +/- 20% with one 360° scan at 49 kVp, 100 mA, and 8 ms.
Two orthogonal low-dose scout images of the breast were obtained prior to the scan. The optimal tube current (mA) to obtain a sufficient contrast-to-noise ratio in the reconstructed cross-sectional images at a minimum dose was determined from these scout images. In this way, the dose was tailored to each individual breast, depending on breast size and density. The dose for each breast scanned was documented based on the mA-to-mGy relationship as mentioned above, in which the dose (CTDIw) is scaled to mA linearly by a factor of 0.08 (Dose = mA × 0.08). Dose from the CBBCT scan was then compared to the dose of each subject's digital mammogram.
Student's paired t-test with two-tailed distribution was used to test for differences between the conventional mammography dose and the CBBCT dose.
Image analysis
Diagnostic mammograms for BI-RADS® 4 and 5 patients were obtained and patients subsequently received CBBCT scans, usually on the same day as the diagnostic exam and all within one week. Patients subsequently underwent image-guided percutaneous core needle and/or excisional biopsy with tissue samples submitted for pathology. Image analysis was not blinded; CBBCT image data sets (transverse, sagittal, coronal, and 3D views) were compared to the prebiopsy diagnostic mammograms (CC and MLO views with additional views as required).
A total of 37 CBBCT scans of 36 patients were obtained. The average number of images generated in each of the three planes (axial, sagittal, and coronal) for one breast on CBBCT is ~500-1000 slices depending on the breast size and the plane viewed. The average time required to scroll through these images is about 5 minutes. The imaging software enables a reader to target a finding of interest in one plane or in 3D and the finding is automatically displayed in the other planes.
Image analysis was performed by two board- and Mammography Quality Standards Act (MQSA)-certified radiologists with 5 and 25 years of experience reading mammography, respectively. The radiologists independently compared the mammographical and CBBCT images side-by-side at a workstation and scored the CBBCT findings relative to the mammographic findings as “not visualized”, “less distinct/conspicuous”, “equally distinct/conspicuous”, or “more distinct/conspicuous”, and were given the opportunity to comment on additional considerations as they deemed appropriate. A third radiologist, similarly certified and with 20 years of experience reading mammography, was available to cast a deciding opinion on lesions scored as “not visualized” or “less distinct/conspicuous” by one reader and “equally distinct/conspicuous” or “more distinct/conspicuous” by the second reader. Inter-observer agreement was tested using Cohen's unweighted Kappa analysis.
Histopathological correlation
Each patient underwent percutaneous stereotactic (8 g or 11 g vacuum-assisted) or ultrasound-guided (9 g or 11 g vacuum-assisted, or 14 g mechanical) core needle biopsy and all malignant or high-risk lesions also underwent surgical excision. Biopsy samples were submitted for standard surgical pathology analysis.
Patient comfort survey
All of the patients were administered a brief paper questionnaire after completing the CBBCT exam. Patients were asked to choose a single best response for “Comfort of Exam vs. Mammogram” by marking one of the following options: “Better”, “Equal”, or “Worse”.
RESULTS
Dose measurement and comparison
Radiation dose resulting from CBBCT was compared with dose resulting from diagnostic mammography for each patient [Figure 1]. Diagnostic mammography was highly variable in dose, ranging from 6 to 36 mGy with a mean of 16.9 mGy (±6.9 SD) ; CBBCT was less variable, ranging from 6.4 to 16, with a mean of 9.4 mGy (±3.1 SD). The number of views taken during the mammographic exam ranged from 2 to 11 in this study with a mean of 5 and standard deviation of 1.94.The difference between total mammography dose (screening and diagnostic) and CBBCT dose was statistically significant in favor of CBBCT (P<0.001). Even when removing the dose attributable to the screening mammography views, difference between CBBCT and diagnostic mammography alone (mean 13.7 mGy, ±3.1 SD) remained statistically significant (P=0.02; 95% confidence interval 0.77-7.1).
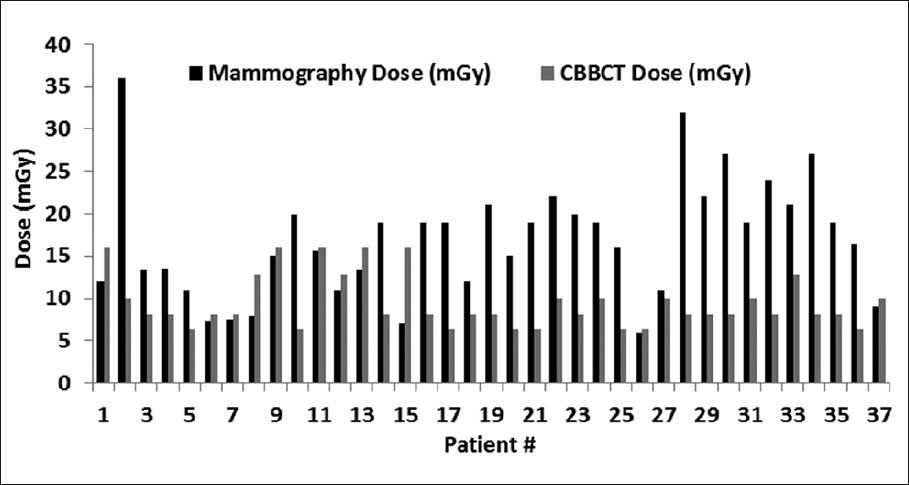
- Dose comparison between diagnostic mammography and CBBCT.
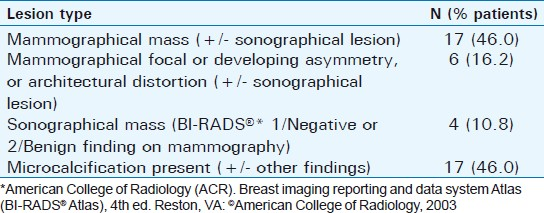
Image analysis and histopathological correlation
CBBCT images of BI-RADS® 4 and 5 lesions were reviewed following mammography and prior to definitive histopathological diagnosis by percutaneous core needle or excisional biopsy. Thirty-three (33) of 37 breasts demonstrated a mammographic abnormality. The classification of the abnormal lesions at time of initial imaging evaluation by mammography with or without ultrasound is summarized in Table 1. A range of breast compositions were represented and are summarized in Table 2.
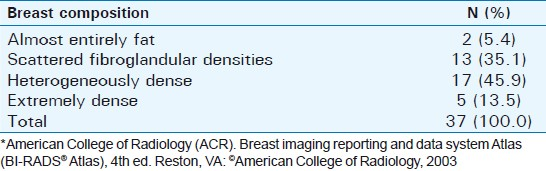
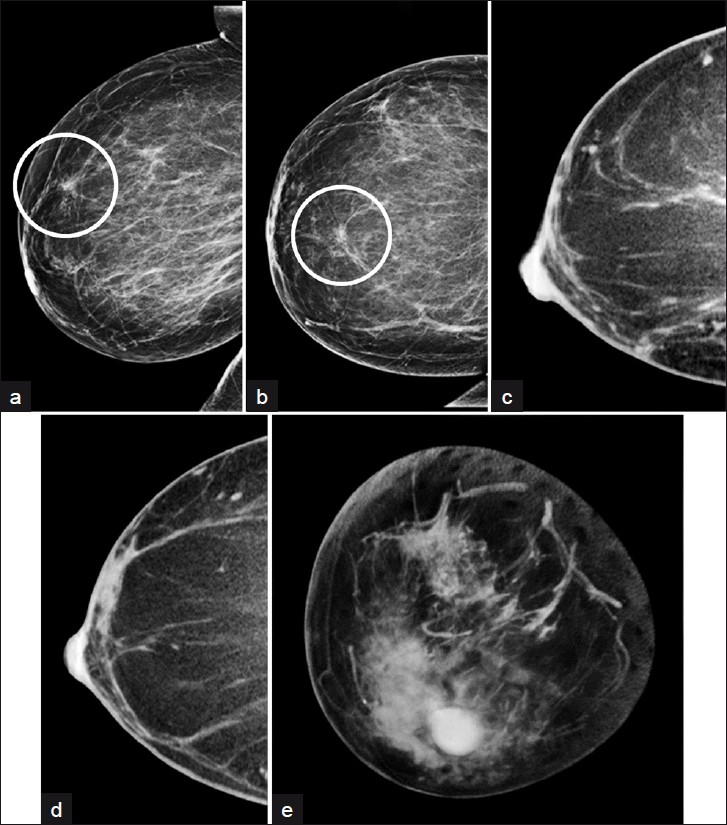
Four BI-RADS® 4 and 5 lesions were identified by diagnostic breast ultrasound and were not seen in conventional mammography, although 2/4 of these were subsequently identified by CBBCT. One of these lesions and the corresponding mammographic and ultrasound findings is depicted in Figure 2.
- A forty-two-year-old woman with palpable lump in upper outer breast. No abnormality was present on mammographical (a) R CC (b) R MLO views (c) biopsy of sonographical mass demonstrated invasive ductal carcinoma. CBBCT demonstrates mass with convex margins arising from glandular tissue in the posterior lateral breast/axilla in both (d) transverse (e) sagittal 1-mm thick sections, which approximate CC and MLO views, respectively.
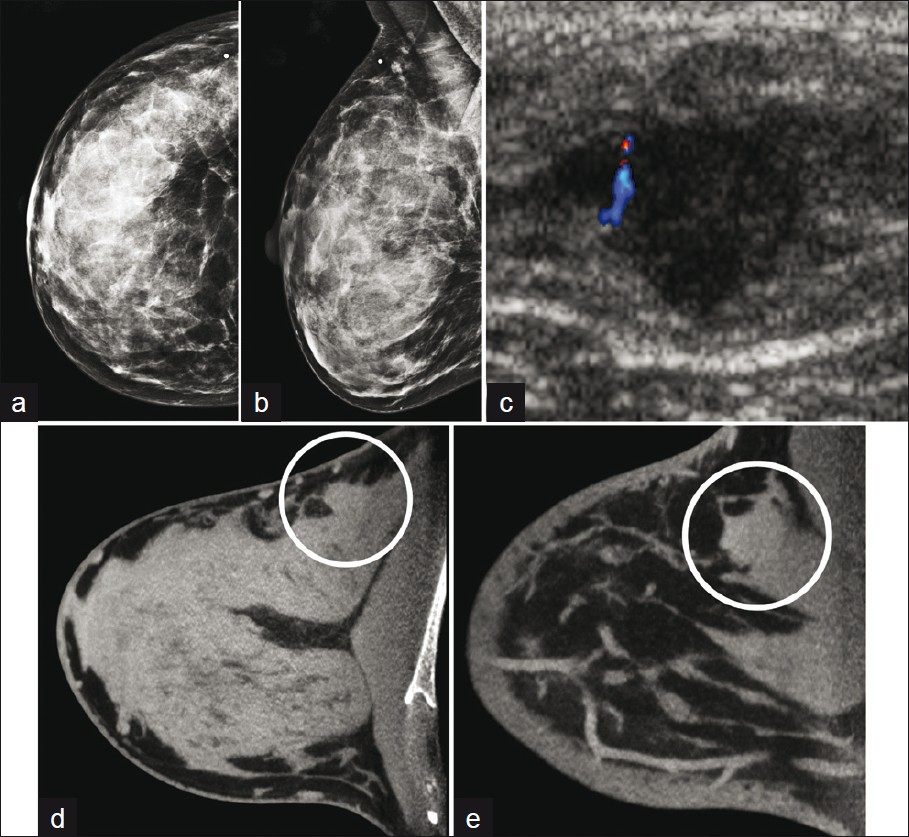
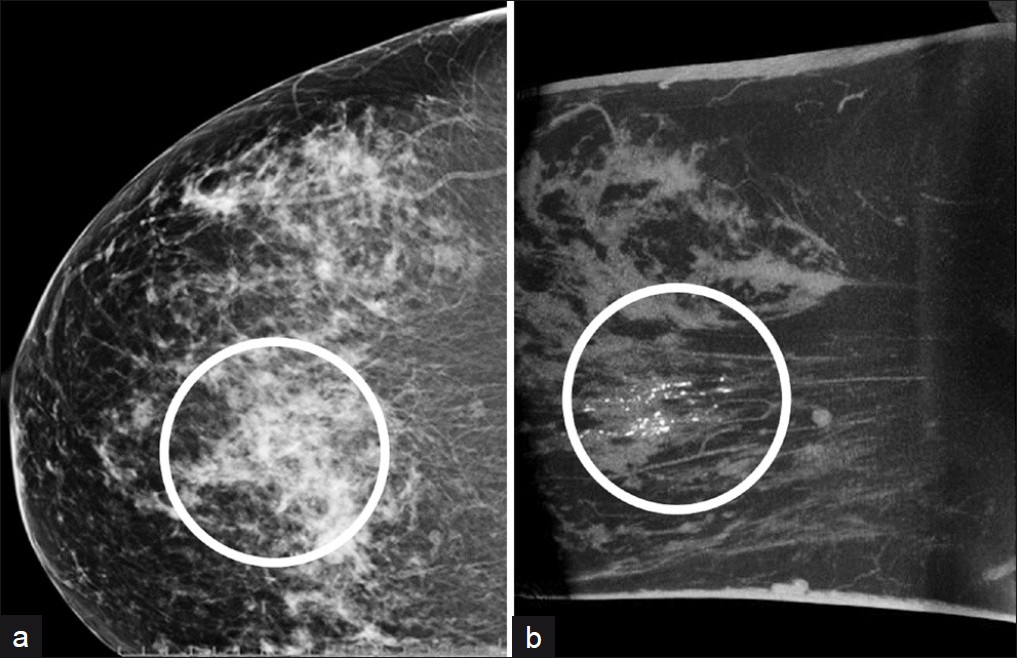
Agreement in conspicuity between lesions identified by diagnostic mammography and CBBCT was high. All but one mammographic abnormality were also seen in CBBCT. The single mammographic finding not identified in CBBCT, classified as a “developing asymmetry” was proven to be benign fibrocystic changes at time of biopsy and can be attributed to summation artifact, as seen in Figure 3. Even allowing for this discordant result, the observed agreement between mammography and CBBCT for lesions initially seen in mammography was 97.0% (32/33).
- A fifty-two-year-old woman with developing focal asymmetry in screening mammography. (a) R ML (b)RCC mammographical views of focal asymmetry in 12 o’clock position in the anterior 1/3 of the right breast, which persisted in spot compression views (not shown). CBBCT (c) sagittal (d) transverse views in the expected location do not demonstrate any suspicious lesion. (e) Volume-rendered CBBT image demonstrates no evidence of mammographical lesion in the anterior breast. Stereotactic biopsy demonstrated benign histology (“fibrocystic changes”).
We anticipated a greater degree of discordance between mammographers in assessing the relative conspicuity of lesions between conventional mammography and CBBCT. In practice, mammographers were in complete agreement in ranking lesions as “not visualized” or in the aggregate category of “equally distinct/conspicuous” and “more distinct/conspicuous”. No lesions were ranked as “less distinct/conspicuous” in CBBCT by either examiner. Across all four categories, the observed Cohen's unweighted Kappa of 0.84 (95% CI: 0.66 – 1).
Examples of common mammographic and sonographical lesions with CBBCT correlation were identified, including palpable lump in extremely dense breast [Figure 2], developing asymmetry [Figure 3], mass with benign features [Figure 4], microcalcifications [Figure 5], and partially obscured mass in the posterior breast [Figure 6].

- A forty-five-year-old woman with mass on screening mammography with benign features. Diagnostic (a) RCC mammographical view transverse CBBCT 0.27-mm section image demonstrate circumscribed mass in the posterior breast (arrowheads). (c) Three-dimensional reconstruction from same CBBCT data set more clearly delineates lesion, demonstrated to be a fibroadenoma following ultrasound-guided biopsy.
- A fifty-five-year-old woman with microcalcifications in screening mammogram. (a) Diagnostic RCC demonstrates clusters of microcalcifications within overlapping glandular tissue. Despite small size, these calcifications are more conspicuous in (b) volume-rendered images at standard 0.27-mm3 resolution. Stereotactic biopsy demonstrated DCIS.
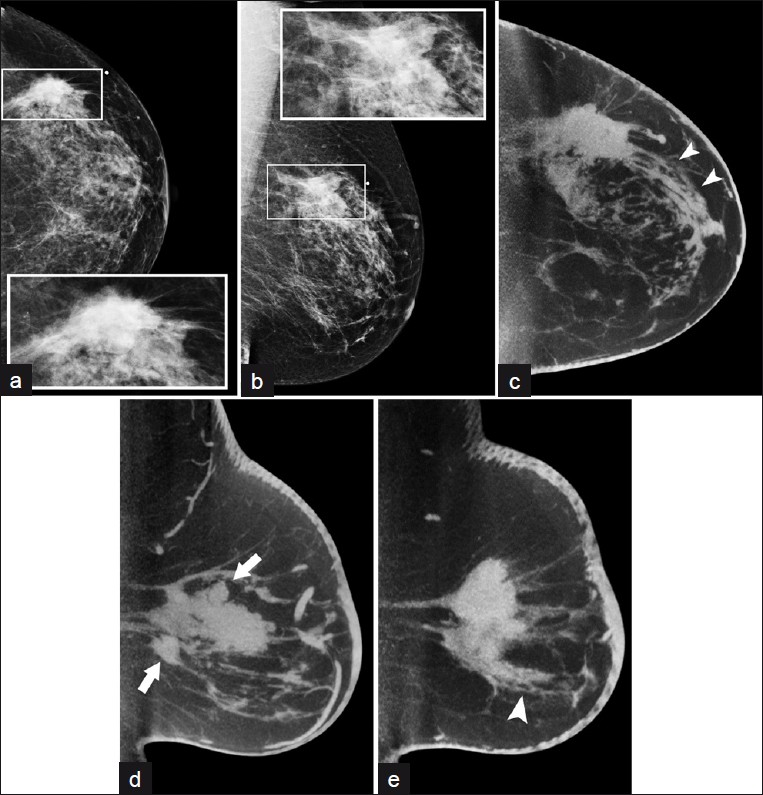
- A fifty-eight-year-old woman with mammographical mass in the posterior breast. Diagnostic (a) L CC (b) MLO views with detail of region of interest (inset); CBBCT images in (c) transverse and sagittal (through the d) medial and (e) lateral portions of the lesion, respectively) 3.0-mm sections demonstrate spicules extending from the mass anteriorly (arrowheads, c and e) and additional possible satellite nodules (arrows, d).
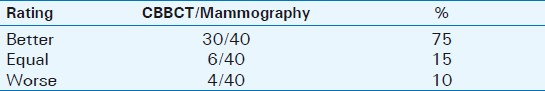
Patient comfort
Patients were administered a survey in order to assess the degree of comfort before and during the CBBCT exam relative to diagnostic mammography [Table 3]. Data from 40 survey participants are included, including four patients ultimately categorized as BI-RADS® 3 and not included in dose or histopathological correlation due to lack of biopsy data. In all, patients reported higher degrees of comfort in the CBBCT examination relative to diagnostic mammography. Thirty six out of forty patients (90%) indicated that the CBBCT examination was equal to or better than mammography in terms of comfort. Response rate was 100%.
DISCUSSION
In light of recent increased attention regarding the importance of radiation dose exposure to patients during imaging studies, the findings of comparable or lower administered dose from CBBCT relative to standard diagnostic mammography is a particularly promising result. As we have demonstrated here, in the diagnostic setting the cumulative dose from diagnostic mammography with spot compression and magnification can be considerable. The radiation dose range in diagnostic mammography was also greater than CBBCT in this pilot study, which accurately reflects the need for a variable number of mammographic views and/or magnification in the diagnostic evaluation of mammographic lesions. In CBBCT, all additional “views” are generated from a data set obtained in a single acquisition; additional scans are not required. Despite the small size of the patient group analyzed, a wide range of patient body types were included in the study and similar dose profiles were obtained in the use of CBBCT. In this regard, CBBCT met our goal of providing a potential alternative and/or complementary imaging modality at radiation dose levels less than that of diagnostic mammography.
While low dose is an attractive feature in isolation, the ability of CBBCT to demonstrate similar accuracy in detecting and depicting breast lesions relative to standard-of-care mammography was a second and equally critical feature that needed to be satisfied in order to consider CBBCT as a breast imaging modality. In a wide array of breast lesions assessed as BI-RADS® 4 or 5 by two experienced mammographers, CBBCT allowed equivalent or superior visualization of the lesion or lesions in question, with the notable exception of a lesion subsequently found to be benign (mammographic false positive) at biopsy. In addition, two malignant lesions identified with diagnostic ultrasound and not visualized with conventional mammography were identified with CBBCT. Because breasts in the study were predominantly heterogeneously or extremely dense [Table 2], we feel that these findings are representative of real-world cases in which mammographical abnormalities may be subtle or otherwise difficult to detect. Therefore, CBBCT met our goal of depicting mammographical abnormalities to a similar degree as diagnostic mammography, with the additional benefit of visualizing two additional malignant lesions not seen in mammography.
This particular CBBCT system acquires images more rapidly than other cone-beam-type scanners described in the literature. As previously described, this system acquires data in a single 10 sec scan, which compares favorably to other systems requiring 12 – 48 seconds, sometimes depending on the resolution of the images acquired.[1314] Short acquisition times are desirable as decreased imaging time results in less motion artifact to obscure fine structures, including but not limited to spiculations and microcalcifications. Microcalcifications were apparent in similar detail to digital mammography, an advantage over magnetic resonance imaging of the breast. Our mammographers felt that the distribution of microcalcifications was better characterized in CBBCT due to the anatomical positioning of the breast and the ability to remove overlapping soft tissue via reconstruction of the CT images, which more than offset the nominally lower spatial resolution of CBBCT relative to digital mammography.
The mammographers also noted that the lesion margins were often more conspicuous in CBBCT relative to conventional mammography, attributed primarily to the ability to exclude tissue outside the plane of interest which would otherwise be superimposed. We anticipate two primary advantages of being able to remove tissue overlap in the use of tomographic sections; firstly, features of benign lesions are identified with a higher degree of confidence, reducing or eliminating the need for biopsy for what would otherwise represent false positive mammographical findings. Secondly, improved characterization of margins and extent of disease may significantly reduce the need for repeat surgeries by improving preoperative evaluation of a lesion prior to excision. Conventional breast-imaging techniques have substantial room for improvement in depicting extent of disease; 30-50% of lumpectomies have positive margins at time of initial resection.[15]
The positioning of the breast during the CBBCT exam confers unique advantages over other imaging modalities. The pendant breast allows evaluation of potential breast lesions without the anatomic distortion intrinsic to techniques that require breast compression. It is reasonable to infer that the dimensions and geographical features of a surgical lesion are better assessed in the noncompressed state. In particular, compression views may lead to underestimation of the overall dimensions of a lesion and increase the likelihood of positive surgical margins at time of excision, as may have been the case for our patients [Figure 4]. CBBCT offers potentially improved presurgical planning that may result in a smaller number of positive margins at excision.
Additional advantages of CBBCT were evident. Patients reported improved subjective comfort relative to diagnostic mammography, which has been described in previous surveys.[14] In addition, acquisition of images in 360° eliminated the need for patient repositioning and additional views, all of which may be generated from the initial data set. No special or additional views are required to more completely visualize posterior lesions partly seen in digital mammography. Also, the lack of additional views contributed to the favorable dose profile of CBBCT relative to diagnostic mammography.
The relative ease of positioning the patient and the natural pendant positioning of the breast limits the opportunity for operator variability and/or error. Images were acquired rapidly and in the span of a single breath-hold, decreasing the potential for motion artifacts, which may seriously compromise the depiction of lesions and microcalcifications in standard mammography. With the exception of a single patient with breast tissue too extensive to be fully visualized in a single field of view , the same imaging protocol and “projection” was obtained for all patients in the study. Neither radiologist felt that there was appreciable motion artifact to degrade image quality.
The field-of-view from a single prone CBBCT examination was excellent. Unlike conventional mammography, which include a portion of the pectoralis major in only 30% of exams performed,[16] readers routinely visualized portions of the anterior chest wall including ribs. Although CBBCT scans the breast in 360°, the breast is fixed and for some subjects the axillary tail is not included in the field of view to the same degree as in standard MLO views. We attribute this to two factors. Firstly, the current table top design limits excursion of the lateral soft tissue of the breast. Secondly, the body habitus of some patients prevents the portions of the lateral breast to be positioned in the imaging field. Further development in our lab in enhancing axillary coverage is currently underway.
Provisions for the use of standard stereotactic and CT-guided biopsy equipment with CBBCT are presently under development. MRI requires dedicated coils with limited access to the breast and requires MR-specific nonferromagnetic biopsy devices. Stereotactic biopsy, while utilizing similar imaging principles as diagnostic mammography, presents unique challenges in identifying and localizing abnormal findings evident in standard mammography. CBBCT may allow the use of the same technology and positioning for both characterization and biopsy of breast lesions.
CONCLUSIONS
Our initial experiences with CBBCT have been promising. At the expense of similar radiation exposure to the patient, this pilot study of patients with a variety of high-risk findings demonstrated CBBCT to be similar to the standard-of-care diagnostic mammography in depicting lesions. Added benefits in this small group of patients included visualization of additional malignant lesions not identified in diagnostic mammography, excellent characterization of lesion margins, and a high degree of patient comfort. Posterior breast tissues were well visualized, as were microcalcifications. We also saw potential for improved characterization of pathology-proven lesions due to true three-dimensional visualization of the breast and lack of compression-related distortion and tissue overlap. These findings are encouraging and we believe that CBBCT clearly warrants additional investigation as an alternative or adjunct to conventional diagnostic mammography in the characterization of high-risk breast lesions identified in screening mammography or ultrasound.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/7/93274
REFERENCES
- American Cancer Society. In: Cancer Facts and Figures 2010. Atlanta, GA: American Cancer Society; 2010. p. :9.
- [Google Scholar]
- Effectiveness of population-based service screening with mammography for women ages 40 to 49 years: Evaluation of the Swedish Mammography Screening in Young Women (SCRY) cohort. Cancer. 2011;117:714-22.
- [Google Scholar]
- Benefit of screening mammography in women aged 40-49: A new meta-analysis of randomized controlled trials. J Natl Cancer Inst Monogr. 1997;22:87-92.
- [Google Scholar]
- Long-term effects of mammography screening: Updated overview of the Swedish randomised trials. Lancet. 2002;359:909-19.
- [Google Scholar]
- Digital breast tomosynthesis in the diagnostic environment: A subjective side-by-side review. AJR Am J Roentgenol. 2010;195:W172-6.
- [Google Scholar]
- High-resolution fluorodeoxyglucose positraon emission tomography with compression (“positron emission mammography”) is highly accurate in depicting primary breast cancer. Breast J. 2006;12:309-23.
- [Google Scholar]
- Breast-specific gamma imaging as an adjunct imaging modality for the diagnosis of breast cancer. Radiology. 2008;247:651-7.
- [Google Scholar]
- Ultrasonic viscoelasticity imaging of nonpalpable breast tumors: Preliminary results. Acad Radiol. 2008;15:1526-33.
- [Google Scholar]
- Cone-beam CT for breast imaging: Radiation dose, breast coverage, and image quality. AJR Am J Roentgenol. 2010;195:496-509.
- [Google Scholar]
- American College of Radiology. In: Breast imaging reporting and data system (BI-RADS) (4th ed). Reston, VA: American College of Radiology; 2003.
- [Google Scholar]
- Evaluation of flat panel detector cone beam CT breast imaging with different sizes of breast phantoms. Proc SPIE. 2005;5745:626-36.
- [Google Scholar]
- Dedicated cone-beam breast CT: Feasibility study with surgical mastectomy specimens. AJR Am J Roentgenol. 2007;189:1312-5.
- [Google Scholar]
- Factors associated with re-excision in patients with early-stage breast cancer treated with breast conservation therapy. Am Surg. 2010;76:331-4.
- [Google Scholar]
- Breast Imaging (3rd ed). Baltimore, MD: Lippincott Williams and Wilkins; 2006.






