Translate this page into:
Computed tomography imaging findings of nivolumab-induced thyroid dysfunction

*Corresponding author: Akitoshi Inoue, Department of Radiology, Shiga University of Medical Science, Otsu, Shiga, Japan. akino@belle.shiga-med.ac.jp
-
Received: ,
Accepted: ,
How to cite this article: Oki T, Inoue A, Nagatani Y, Oki M, Watanabe Y. Computed tomography imaging findings of nivolumab-induced thyroid dysfunction. J Clin Imaging Sci 2022;12:22.
Abstract
The thyroid gland is most frequently involved in immune-related adverse events (irAEs) by nivolumab. We reviewed the thyroid function and thyroid gland volume and volume change ratio between baseline and follow-up CT (volume follow-up/volume baseline) in 24 patients treated with nivolumab for lung cancer and renal cell carcinoma. Among them, four (16.7%) demonstrated nivolumab-induced thyroid dysfunction that shows either hypothyroidism or hyperthyroidism. Three and one cases were treated with nivolumab for lung cancer and renal cell carcinoma, respectively. Two patients with hypothyroidism (cases 1 and 2) showed reduced thyroid volume (volume change ratio: 0.80 and 0.84) on computed tomography (CT) images. Besides, remarkably diminished CT attenuation of the thyroid gland was observed in a patient with hypothyroidism (case 2). One of the two patients with hyperthyroidism showed increased thyroid volume (volume change ratio: 1.32) (case 3), whereas no difference in the thyroid gland volume was observed between the previous and follow-up CT in another patient with hyperthyroidism (case 4). Thyroid volume change ratio >0.1 was observed even in 6 of 20 (30%) patients without thyroid dysfunction. Considering the wide use of nivolumab in cancer treatment, radiologists should be aware that changes in the thyroid volume and attenuation on CT are associated with thyroid dysfunction caused by nivolumab, as well as thyroid volume may change even in patients with normal thyroid function during nivolumab therapy.
Keywords
Thyroid gland
Nivolumab
Immune checkpoint inhibitor
Computed tomography
Volumetry
INTRODUCTION
Nivolumab is a specific monoclonal antibody of the anti-programmed death protein-1.[1] Nivolumab was originally used for malignant melanoma and has recently played an important role in the treatment of malignant neoplasms, such as Hodgkin’s lymphoma, lung cancer, renal cell carcinoma, head and neck, breast, esophageal, gastric, colorectal, and bladder cancers.[2]
However, various immune-related adverse events (irAEs) associated with nivolumab, including dermatologic disease, colitis, hepatitis, pneumonitis, cardiovascular disease, and endocrine disease have been known.[3] These irAEs may result in visits to the emergency department.[4] Among irAEs of the endocrine system, thyroid irAE is defined as new laboratory abnormalities indicating thyroid dysfunction after starting nivolumab is the most frequent adverse event.[5] Hypothyroidism is the most prevalent pathology followed by hyperthyroidism and thyroiditis. Symptomatic thyroid irAE is required to be treated by medication.
The clinical courses of thyroid irAE during nivolumab therapy were well-documented in several articles, and most oncologists are expected to be familiar with it.[6] However, only a few articles reported qualitative or quantitative imaging findings including the volume changes of the thyroid gland during nivolumab therapy.[7,8] Similarly, tyrosine kinase inhibitors induce thyroid dysfunction and atrophy in the thyroid,[9] and nivolumab causes changes in the thyroid gland volume.[7,8] We reported CT imaging findings of nivolumab-induced thyroid dysfunction and frequency in this case series.
METHODS
We screened the patients who took immunotherapy using nivolumab for advanced lung cancer or renal cell carcinoma and those who underwent CT scans using radiology information system and reviewed if the CT scan covered the entire thyroid gland between July 2014 and December 2018. We focused on these two neoplasms because physicians treating patients with them always addressed “nivolumab” in the radiology information systems and it was thought to collect patients without screen bias. Patients were included if they met the following criteria: (1) CT images (thickness = 1 mm) that covered the entire thyroid gland were available before and during nivolumab therapy, (2) the level of serum-free thyroxine (FT4) and thyroid-stimulating hormone (TSH) in the blood test were available before and during nivolumab therapy for at least 2 months, (3) normal thyroid function was assessed before nivolumab therapy, and (4) nivolumab therapy and clinical follow-up were performed at our institution. Patients who did not match these inclusion criteria were excluded.
Thereafter, we reviewed medical records of patients to investigate the free thyroxine (FT4) and thyroid-stimulating hormone (TSH) levels before initiating the nivolumab therapy and at subsequent follow-ups. The dates of nivolumab therapy initiation and computed tomography (CT) examination were recorded. A radiologist with 4 years of experience in imaging diagnosis (T.O.) manually segmented the thyroid grand in the axial planes to obtain areas (mm2) using the open-source image processing software ImageJ (version 1.51, National Institute of Health, Bethesda, MD, USA). The volumes of the thyroid gland (mm3) were calculated by adding all the areas of the thyroid gland traced in all axial CT images.
The results of FT4 and TSH before nivolumab therapy were considered as the baseline levels. The thyroid function blood tests were regularly monitored every 1 to 2 months during nivolumab therapy, and additional tests were performed in patients who were suspected to have thyroid dysfunction based on physical examinations. Thyroid dysfunction was defined if the laboratory tests of FT4 (normal range: 0.82-1.63 ng/dl) and TSH (normal range: 0.38-4.31 μIU/mL) were outside the normal ranges. Hyperthyroidism was considered in the cases of increased FT4 and decreased TSH levels, and hypothyroidism was considered in the cases of decreased FT4 and increased TSH levels.[10]
RESULTS
We identified 56 potential patients treated with nivolumab for advanced lung cancer and renal cell carcinoma and 32 patients were excluded for the following reason: (1) CT images with 1 mm thickness that covered the entire thyroid gland both before and during nivolumab therapy were not available (n = 14), (2) The results of the level of FT4 and TSH were not available (n = 15), (3) abnormal thyroid function before nivolumab therapy (n = 2), and (4) nivolumab therapy was initiated in other institution (n = 1) [Figure 1]. Finally, 24 patients (mean age: 64.8 ± 7.9 years old; male:female = 19:5, lung cancer (n = 22), renal cell carcinoma (n = 2)) were enrolled. CT examination was carried out at 65.8 α 24.0 days after nivolumab therapy. As a result, four patients demonstrated thyroid dysfunction (hyperthyroidism (n = 2) and hypothyroidism (n = 2)). Although the other 20 patients did not show thyroid dysfunction, 6 (30%) demonstrated over 0.1 thyroid volume change ratio [Table 1]. The patient demographic in the six patients who had over 0.1 of thyroid volume change ratio but no thyroid disfunction is following: mean age: 66.3 α 7.8 years old; male: female = 4:2, lung cancer (n = 5): renal cell carcinoma (n = 1) similar to other 14 patients neither over 0.1 of thyroid volume change ratio nor thyroid dysfunction [mean age: 65.9 α 8.0 years old; male: female = 11:3; lung cancer (n = 14)].
| Serial number | Age | Sex | Category | CT exam days after nivolumab | Thyroid gland volume change ratio |
|---|---|---|---|---|---|
| 1 | 56 | M | Normal | 63 | 1.00 |
| 2 | 73 | M | Normal | 70 | 1.06 |
| 3 | 74 | M | Normal | 56 | 1.06 |
| 4 | 77 | M | Normal | 61 | 1.11 |
| 5 | 57 | M | Normal | 54 | 0.98 |
| 6 | 65 | M | Normal | 54 | 0.96 |
| 7 | 69 | M | Normal | 51 | 1.04 |
| 8 | 69 | F | Normal | 70 | 0.98 |
| 9 | 56 | M | Normal | 81 | 1.15 |
| 10 (Case 1) | 52 | M | Hypothyroidism | 143 | 0.8 |
| 11 | 68 | F | Normal | 56 | 1.08 |
| 12 | 65 | M | Normal | 54 | 0.9 |
| 13 (Case 3) | 57 | M | Hyperthyroidism | 63 | 1.32 |
| 14 | 60 | F | Normal | 38 | 0.97 |
| 15 | 60 | M | Normal | 35 | 1.05 |
| 16 | 75 | M | Normal | 42 | 1.07 |
| 17 | 59 | M | Normal | 128 | 0.79 |
| 18 | 68 | F | Normal | 53 | 1.12 |
| 19 | 69 | F | Normal | 59 | 0.94 |
| 20 (Case 2) | 71 | M | Hypothyroidism | 49 | 0.84 |
| 21 | 75 | F | Normal | 70 | 1.32 |
| 22 (Case 4) | 70 | M | Hypothyroidism | 84 | 0.98 |
| 23 | 63 | M | Normal | 77 | 0.84 |
| 24 | 47 | M | Normal | 56 | 0.94 |
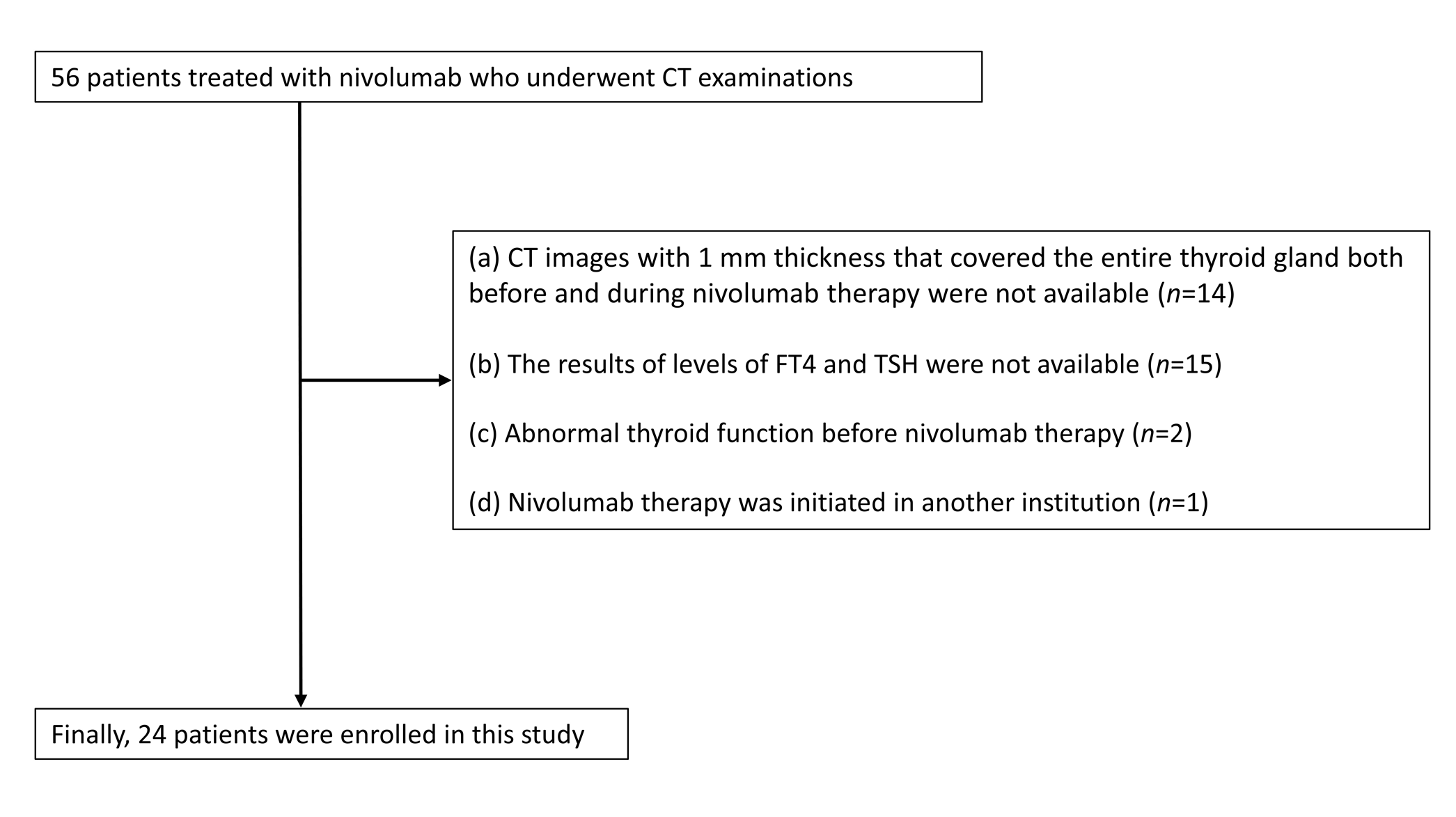
- Patient enrollment.
CASE REPORTS
Case 1
A 52-year-old man was treated with thoracoscopic radical resection for the right lower lobe tumor 7 years ago. He was histopathologically diagnosed with adenocarcinoma mixed type (T1N1M0; Stage IIA) and treated with postoperative adjuvant chemotherapy. However, mediastinal lymph node metastasis and carcinomatous pleurisy recurred 4.5 years postoperatively. He underwent subsequent chemotherapy and molecular targeted therapy [carboplatin and nab-paclitaxel (1st line), crizotinib (2nd line), and alectinib (3rd line)]. Afterward, he received nivolumab therapy (180 mg/body and 3 mg/kg, alternatively) biweekly. Laboratory tests exhibited normal levels of FT4 (1.06 ng/mL) and TSH (1.08 μIU/mL) 16 days before nivolumab therapy. A laboratory follow-up test at 47 days after starting nivolumab therapy demonstrated high FT4 (1.56 ng/mL) and low TSH (0.01 μIU/mL) levels, which were compatible with hyperthyroidism. However, patients did not complain of any associated symptoms. Conversely, other follow-up laboratory analyses on 75 days after starting nivolumab therapy demonstrated low FT4 (0.43 ng/mL) and high TSH level (14.63 μIU/mL), and physical examination revealed fatigue and eyelid edema, which were compatible with hypothyroidism. Thyroid hormone replacement therapy using levothyroxine was initiated at the dose of 25 μg/day 131 days after starting nivolumab therapy [Figure 2a]. Compared with the baseline CT [Figure 2b], follow-up CT 143 days after starting nivolumab therapy demonstrated reduced thyroid gland volume [Figure 2c] with a volume change ratio of 0.80.

- Decreased thyroid gland volume in hypothyroidism. A 52-year-old man with advanced lung cancer exhibited normal levels of FT4 (1.16 ng/mL) and TSH (1.08 uIU/mL) 16 days before nivolumab therapy. (a) The chart displaying the levels of free thyroxine (T4) and thyroid-stimulating hormone (TSH) showed an increased FT4 (1.56 ng/mL) level and decreased TSH (0.01 uIU/mL) level at 47 days after beginning nivolumab therapy and decreased FT4 level (0.43 ng/mL) and increased TSH level (14.63 uIU/mL) at 75 days after beginning nivolumab therapy. (b) Compared with the baseline CT. (c) Follow-up CT 143 days after beginning nivolumab therapy demonstrated reduced thyroid gland volume. The volume change ratio was 0.80, respectively. T4; free thyroxine, TSH; thyroid-stimulating hormone
Case 2
A 71-year-old man underwent retroperitoneal laparoscopic radical nephrectomy for left renal cell carcinoma 5 years and 3 months ago. Histopathological analysis showed papillary renal cell carcinoma (T3aN0M0, Stage I). Lung metastasis in the left upper lobe and right middle lobe was suspected at 3 years and 3 months postoperatively. He underwent thoracoscopic resection of the left upper lobe, and postoperative pathological analysis revealed lung metastasis. He was treated with the following molecular targeted therapy: pazopanib (1st line) and axitinib (2nd line). Eventually, he received nivolumab therapy (171 mg/body and 3 mg/kg) biweekly. His FT4 (1.43 ng/mL) and TSH (1.43 μIU/mL) levels were normal on a baseline laboratory test seven days before starting nivolumab therapy. The laboratory test showed 3.99 ng/mL of FT4 and 0.01 μIU/mL of TSH. These findings were compatible with hyperthyroidism despite the lack of associated symptoms 35 days after starting nivolumab therapy. Approximately 4 months later, the patient was asymptomatic, but a blood test showed hypothyroidism (FT4: 0.89 ng/mL, TSH: 11.74 μIU/mL) 133 days after starting nivolumab therapy. Hormone replacement therapy using levothyroxine was initiated with oral levothyroxine 25 μg/day at the same time [Figure 3a]. Compared with baseline CT [Figure 3b], follow-up CT at 49 days after starting nivolumab therapy demonstrated a slightly decreased thyroid gland volume [Figure 3c] with a volume change ratio of 0.84.

- Decreased thyroid gland volume and density in hypothyroidism. A 71-year-old man with renal cell carcinoma was treated with nivolumab after standard treatment. (a) The chart displaying free thyroxine (T4) and thyroid-stimulating hormone (TSH) levels exhibited normal FT4 (1.43 ng/mL) and TSH (1.43 uIU/mL) levels on a baseline laboratory test seven days before starting nivolumab therapy. The laboratory test yielded 3.99 ng/mL of FT4 and 0.01 uIU/mL of TSH on day 35 days after the beginning of nivolumab therapy. A laboratory test at 133 days after starting nivolumab therapy demonstrated decreased FT4 (0.89 ng/mL) and increased TSH (11.74 uIU/mL) levels. Hormonal replacement therapy using levothyroxine was initiated with the use of oral levothyroxine at 25 ug/day simultaneously. (b) Compared with baseline CT. (c) Follow-up CT at 49 days after the beginning of nivolumab therapy demonstrated a slightly decreased thyroid gland volume and remarkably diminished thyroid gland density. The volume change ratio was 0.84. T4; free thyroxine, TSH; thyroid-stimulating hormone.
Case 3
A 57-year-old man with advanced lung cancer received neoadjuvant chemoradiation therapy using nedaplatin and docetaxel and subsequent thoracoscopic radical resection for left lower lobe lung cancer 5 years ago. He was pathologically diagnosed with adenocarcinoma mixed type (T1aN2M0, Stage IIIA), for which he received postoperative adjuvant chemotherapy using carboplatin and pemetrexed. Mediastinal nodal recurrence was found at 3 years and 6 months postoperatively. He was treated with carboplatin, pemetrexed, bevacizumab (1st line), and pemetrexed (2nd line). Thereafter, he received nivolumab therapy (240 mg/body and 3 mg/kg) biweekly. He exhibited normal FT4 (1.03 ng/mL) and TSH (0.83 μIU/mL) levels on a baseline laboratory test 14 days before starting nivolumab therapy. The laboratory test revealed elevated FT4 (2.48 ng/mL) and TSH (0.02 μIU/mL) levels that indicated hyperthyroidism despite the lack of associated symptoms 44 days after starting nivolumab therapy [Figure 4a]. Compared with baseline CT [Figure 4b], follow-up CT 63 days after starting nivolumab therapy demonstrated an enlarged thyroid gland [Figure 4c] with a volume change ratio of 1.32.

- Increased thyroid gland volume in hyperthyroidism A 57-year-old man was treated with nivolumab for lung cancer after standard chemotherapy. (a) The medical chart showed normal levels of FT4 (1.03 ng/mL) and TSH (0.83 uIU/mL) on a baseline laboratory test 14 days before starting nivolumab therapy and increased FT4 (2.48 ng/mL) and TSH (0.02 uIU/mL) levels at 44 days after starting nivolumab therapy. (b) Compared with baseline CT. (c) Follow-up CT 63 days after starting nivolumab therapy demonstrated an enlarged thyroid gland. The volume change ratio was 1.32. T4; free thyroxine, TSH; thyroid-stimulating hormone.
Case 4
A 70-year-old man was clinically diagnosed with advanced lung cancer in the right upper lobe associated with multiple intrapulmonary metastases, right hilar nodal metastasis, and pleural dissemination (T4N1M1a, stage IV). He was treated with the following chemotherapy for 18 months: cisplatin and gemcitabine (1st line), and carboplatin and nab-paclitaxel (2nd line). Next, he received nivolumab therapy (184 mg/body and 3 mg/kg) biweekly. He exhibited normal FT4 (1.18 ng/mL), and TSH (1.56 μIU/mL) levels on a baseline laboratory test 3 days before starting the nivolumab therapy. The laboratory test revealed increased FT4 (2.32 ng/mL) and TSH (0.04 μIU/mL) levels that indicated hyperthyroidism despite the lack of associated symptoms 29 days after starting nivolumab therapy [Figure 5a]. Follow-up CT 84 days after starting nivolumab therapy showed progressive disease in multiple lesions, after which the therapy was discontinued. The laboratory test 105 days after the onset of nivolumab therapy exhibited normal FT4 (0.92 ng/mL) and TSH (0.74 μIU/mL) levels. Compared with baseline CT [Figure 5b], follow-up CT 84 days after starting nivolumab therapy demonstrated that the volume of the thyroid gland had slightly changed with a volume change ratio of 0.98 [Figure 5c].

- No volume change of the thyroid gland in hyperthyroidism A 70-year-old man with advanced lung cancer was treated with nivolumab. (a) Normal FT4 (1.18 ng/mL) and TSH (1.56 uIU/mL) levels on a baseline laboratory test 3 days before starting nivolumab therapy and increased FT4 (2.32 ng/mL) and TSH (0.04 uIU/mL) levels at 29 days after starting nivolumab therapy. (b) Compared with baseline CT. (c) Follow-up CT 84 days after starting nivolumab therapy demonstrated that the thyroid gland volume slightly changed. The volume change ratio was 0.98. CT findings also showed progressive disease of multiple lesions, after which the therapy was discontinued. Afterward, a laboratory test 105 days after starting nivolumab therapy exhibited normal FT4 (0.92 ng/mL) and TSH (0.74 uIU/mL) levels. T4; free thyroxine, TSH; thyroid-stimulating hormone.
DISCUSSION
Previous studies on thyroid irAE due to nivolumab investigated thyroid hormone levels only, and a few articles mentioned imaging findings including changes in the thyroid gland volume.[7,8] In the 24 patients who were screened, volumetry analysis revealed a >0.1 thyroid volume changes ratio (range: 0.79 to 1.32) in nine patients (37.5%), including those with and without thyroid dysfunction. This prevalence of thyroid volume change was slightly higher than that of thyroid dysfunction in previous reports (11.7-33.5%).[11-15]
Broad-spectrum clinical courses that indicated whether (1) cases were symptomatic or asymptomatic irrespective of whether hyperthyroidism or hypothyroidism occurred, and (2) whether treatment was necessary or unnecessary, had been reported in previous studies.[16] Two distinct clinical patterns of immune checkpoint inhibitor-induced hypothyroidism were documented: one was a case of hyperthyroidism followed by hypothyroidism (biphasic pattern) and the other was de novo hypothyroidism.[12]
CT revealed decreased thyroid gland volume before the hormone tests of hypothyroidism in cases 1 and 2 [Figures 2 and 3]. Therefore, CT volumetry might assist in the diagnosis of hypothyroidism in patients affected by hyperthyroidism. In addition, non-contrast CT revealed a low attenuated thyroid gland in the patient with hypothyroidism [Figure 3]. Given that, the onset of thyroid irAE induced by nivolumab is within 7-20 weeks.[5] A several months later follow-up, CT examination for the assessment of tumor response was potentially helpful in the early detection of developing hypothyroidism. In the case of hyperthyroidism, one patient demonstrated an increased thyroid gland volume ratio of >0.1 (case 3), whereas the other showed no significant changes (case 4). Itonaga et al. reported thyroid volume change ratio between baseline and follow-up within 1-4 months is higher in the irAE group than in the non-irAE one (median: 1.11 vs. 0.99; p = 0.122).[7] Given a wide range of CT scans (1-4 months after the beginning of the nivolumab therapy) as well as the fact that thyroid irAE is observed at different timing for each case (7-20 weeks), their study included a heterogeneous cohort (i.e., hypothyroidism (n = 3), hyperthyroidism (n = 4)). In our report, two hypothyroidism cases demonstrated a markedly decreased thyroid volume ratio (0.84 and 0.80) [Figures 2 and 3] and one hyperthyroidism case highly increased thyroid volume ratio (1.32) [Figure 4]. Based on the results, increasing and decreasing thyroid volume are associated with hyper and hypothyroidism in thyroid irAE, respectively. However, the other hyperthyroidism case showed almost normal (0.98) [Figure 5]. We speculated the reason why this case showed only a mild change in thyroid volume was hyperthyroidism evoked by the immune reaction was peaked out before CT scanning as shown in the time course in the graph [Figure 5a]. In this case series, >0.1 of increased thyroid volume ratio was associated with hyperthyroidism or 25% of those with normal thyroid function who do not require hormone suppression therapy. Given that the thyroid volume measurement revealed a marked volume change in the thyroid gland in some patients with normal FT4 and TSH levels during follow-up, a subclinical immune reaction in the thyroid gland may be more frequent than expected based on laboratory tests.
Interestingly, patients with thyroid irAE demonstrate longer median overall survival than those without it, and immune reaction in the thyroid gland might reflect anti-tumor effectiveness by nivolumab.[15] The role of imaging modalities is limited in the diagnosis of thyroid irAE due to nivolumab. However, some articles reported fluorodeoxyglucose (FDG) uptake in the thyroid gland based on positron emission tomography (PET) conducted before and during nivolumab therapy, indicating that nivolumab induced thyroid irAE.[15] CT is extensively employed as an imaging modality in the monitoring of response for treatment, and surveillance of adverse events during treatment for various malignant neoplasms. The marked thyroid volume changes, especially when the volume decreases, are clinically significant and similar to FDG uptake in the thyroid gland. On the other hand, an increased thyroid volume within 3 months of the beginning of nivolumab therapy can predict a higher possibility of complete response.[7] Regardless of the thyroid function, increased thyroid volume on CT might be predictive of a good prognosis.
History of radiation to the neck is significantly associated with thyroid irAE caused by immune checkpoint inhibitors.[16] In this case series, only one case (serial 11) underwent radiation therapy to the neck region for metastasis for the cervical spine and upper rib, and thyroid irAE was not observed. In four cases with thyroid irAE, two patients underwent neoadjuvant chemoradiation therapy for lung cancer in the lower lobe, which did not include the neck region in the irradiation area. Radiation to the neck region is not associated with thyroid irAE in this cohort. As the previous article reported, the frequency of thyroid irAE is 35% and 33% in lung cancer and malignant melanoma, underlying cancer type does not seem to change the frequency of thyroid irAE.[15]
There are several limitations to this case series. Firstly, the numbers of enrolled patients were relatively small and focused on lung cancer and renal cell carcinoma. Secondly, the follow-up timings of the CT and laboratory tests were not restricted. The thyroid gland volume was measured only on the initial follow-up CT approximately 2-3 months after nivolumab therapy because of the retrospective nature. Finally, patient outcomes such as treatment response and overall survival were not evaluated.
Conclusion
Decreased thyroid volume and attenuation were observed in nivolumab-induced hypothyroidism, whereas increased thyroid volume was observed in nivolumab-induced hyperthyroidism. Any obvious changes in the thyroid volumes are not only linked to thyroid irAE but also are common even in patients with normal thyroid function during nivolumab therapy.
Declaration of patient consent
Institutional Review Board (IRB) permission has been obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Endocrine-related adverse events associated with immune checkpoint blockade and expert insights on their management. Cancer Treat Rev. 2017;58:70-6.
- [CrossRef] [PubMed] [Google Scholar]
- Thyroid disorders induced by checkpoint inhibitors. Rev Endocr Metab Disord. 2018;19:325-33.
- [CrossRef] [PubMed] [Google Scholar]
- Immune-related adverse events (irAEs): Diagnosis, management, and clinical pearls. Curr Oncol Rep. 2020;22:39.
- [CrossRef] [PubMed] [Google Scholar]
- Adverse effects of immune checkpoint therapy in cancer patients visiting the emergency department of a comprehensive cancer center. Ann Emerg Med. 2019;73:79-87.
- [CrossRef] [PubMed] [Google Scholar]
- Immune checkpoint inhibitors: Review and management of endocrine adverse events. Oncologist. 2016;21:804-16.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Rapid evolution of thyroid dysfunction in patients treated with nivolumab. Endocr Pract. 2017;23:1223-31.
- [CrossRef] [PubMed] [Google Scholar]
- Morphological changes of the thyroid gland as a new radiographic marker for lung cancer treatment efficacy of immune checkpoint inhibitors. Acta Radiol. 2021;62:42-50.
- [CrossRef] [PubMed] [Google Scholar]
- Acute inflammatory thyromegaly following checkpoint inhibition: A new imaging entity? Radiol Case Rep. 2018;13:89-91.
- [CrossRef] [PubMed] [Google Scholar]
- Organ atrophy induced by sorafenib and sunitinib - quantitative computed tomography (ct) evaluation of the pancreas, thyroid gland and spleen. Pol. J Radiol. 2016;81:557-65.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- How to interpret thyroid function tests. Clin Med (Lond). 2013;3:282-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Incidence of thyroid dysfunctions during treatment with nivolumab for non-small cell lung cancer: Retrospective study of 105 patients. Presse Med. 2019;48:e199-e207.
- [CrossRef] [PubMed] [Google Scholar]
- Two distinct clinical patterns of checkpoint inhibitor-induced thyroid dysfunction. Endocr Connect 2020:318--.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Potential risk factors for nivolumab-induced thyroid dysfunction. In Vivo. 2017;31:1225-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Thyroid dysfunction induced by nivolumab: Searching for disease patterns and outcomes. Endocrine. 2019;64:605-13.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence, features, and prognosis of immune-related adverse events involving the thyroid gland induced by nivolumab. PLoS One. 2019;14:e0216954.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Nivolumab-induced thyroid dysfunction. Jpn J Clin Oncol. 2016;46:575-9.
- [CrossRef] [PubMed] [Google Scholar]







