Translate this page into:
Computed Tomography-guided Pulmonary Nodule Microcoil Localization Technique, Misplacement Errors, and Complications: A Pictorial Essay
Address for correspondence: Dr. Sultan R Alharbi, Department of Radiology and Medical Imaging, College of Medicine, King Saud University, P.O. Box 7805, Riyadh 11472, Kingdom of Saudi Arabia. E-mail: drsultan000@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Computed tomography-guided pulmonary nodule microcoil localization is done preoperatively to fluoroscopic-guided video-assisted thoracoscopic surgical resection. This pictorial essay explains and illustrates the microcoil localization technique, various microcoil placement errors, intraoperative fluoroscopy-guided resection, and postmicrocoil localization complications.
Keywords
Computed tomography-guided microcoil localization
pulmonary nodule
video-assisted thoracoscopic lung resection

INTRODUCTION
Recently, video-assisted thoracoscopic surgery (VATS) has become the choice in the workup of small pulmonary nodules. VATS can be diagnostic and therapeutic, and it can prevent the potential sampling error inherent with a fine-needle aspiration.[1] However, VATS is limited because the surgeon is unable to palpate the lung tissue during operation, which may render the intraoperative identification of small pulmonary nodules difficult.[2] Thus, failure to visualize or palpate small pulmonary nodules has resulted in conversion thoracotomy rates of up to 54%.[3]
Pulmonary nodule localization techniques have been previously described and can be classified into three major types: image-guided surgery, injection of liquid materials through fine needles, and placement of percutaneous wires.[4] Microcoil localization technique to fluoroscopically guided VATS excision of small lung nodules increased the success rate of VATS excision to 97% compared with the reported 54% success rate with the nonguided approach.[5]
MICROCOIL PLACEMENT
A 10-cm-long 21G Chiba needle is loaded with a 7-cm-long, 0.018-inch-diameter fiber-coated platinum microcoil by a microcoil pusher. Using a sterile surgical marker pen, two measurements are marked on the same needle stylet [Figure 1]. Under computed tomography (CT) guidance, the loaded Chiba needle is pushed through and just deeper to the nodule. The premeasured needle stylet is advanced into the Chiba needle deploying about 3 cm of the microcoil into the lung parenchyma just deeper to the nodule [Figure 2]. A second localizer CT scan is obtained to confirm the microcoil deployment and measure the distance necessary to withdraw the tip of the Chiba needle back to the pleural space. After that, the Chiba needle is pulled back to the pleural surface while the needle stylet is held against the end of the microcoil. Then, the needle stylet is advanced completely deploying the remaining microcoil at the visceral pleural surface. After deployment, the Chiba needle is removed from the chest wall [Figure 3].
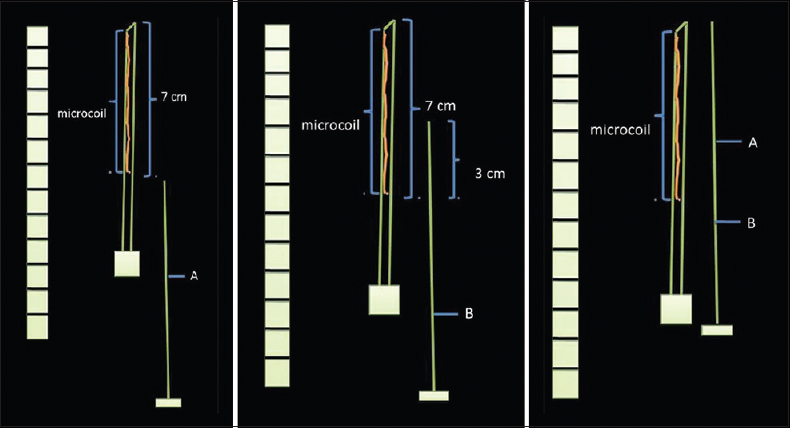
- Diagrammatic scheme of predeployment measurement: After loading the 7-cm microcoil into 10-cm 21G Chiba needle by microcoil pusher, two marks were put by a sterile surgical marker pen on the needle stylet. Mark A: The length enough to push the microcoil to the tip of the needle. Mark B: The length enough to eject 30 mm of the microcoil.
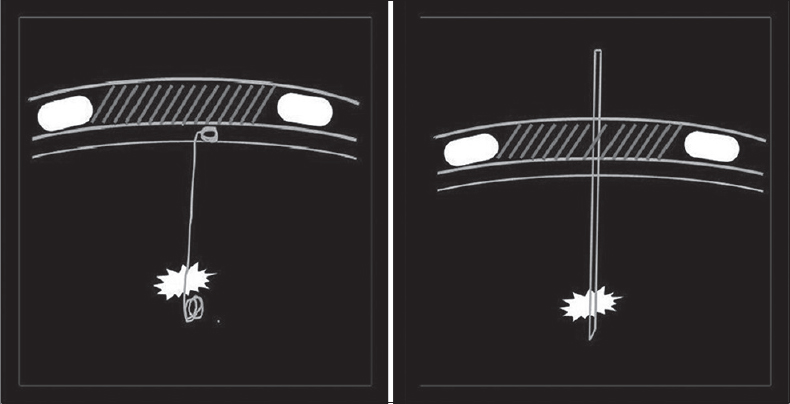
- Diagrammatic scheme of deployment location A, a microcoil-loaded Chiba needle was pushed through and just beneath the pulmonary nodule. Location B: The deeper microcoil end tightly coiled deep to the nodule while the superficial end loosely coiled on the visceral pleural surface.
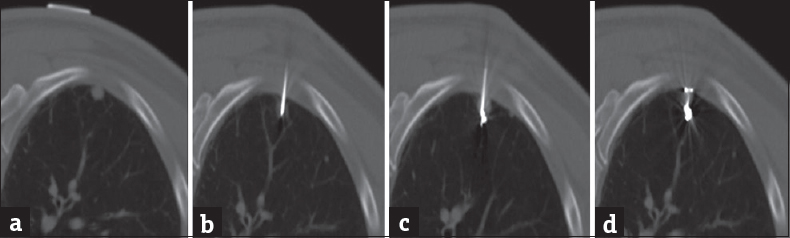
- (a) Preprocedural computed tomography with skin localization showing pulmonary nodule. (b) A loaded Chiba needle passed through the pulmonary nodule. (c) The microcoil pushed out and tightly coiled deep to the nodule. (d) The Chiba needle was removed and the proximal microcoil end coiled on the visceral pleural surface.
INTRAOPERATIVE FLUOROSCOPIC GUIDANCE
Under general anesthesia, a double-lumen endotracheal tube is inserted and the involved lung is deflated. Three thoracoscopic ports are made. Wedge resection of the lung nodule and microcoil is done using grasping instrument and stapling device. Fluoroscopy is used to aid and confirm microcoil and complete resection of the nodule. The resected specimen is sent for frozen section [Figures 4 and 5].[67] A 24G chest tube is insertwed at the end of the procedure [Figure 6].[8]
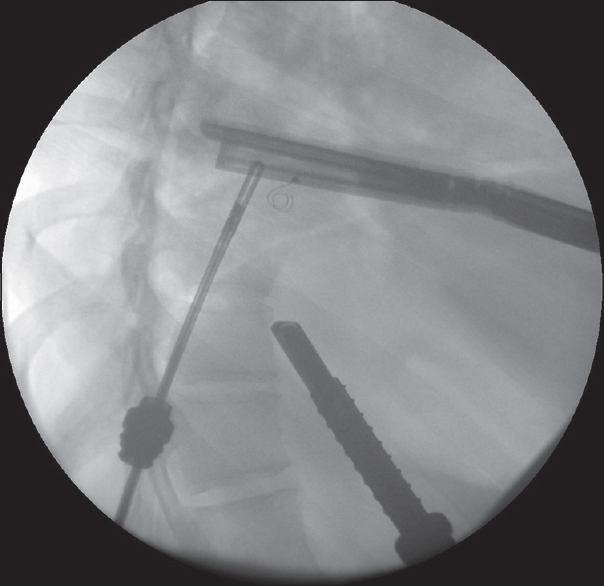
- Fluoroscopic image during the video-assisted thoracoscopic lung resection, showing the microcoil within the lung parenchyma. A thoracoscopic port, grasping instrument, and linear stapling devices are noted.
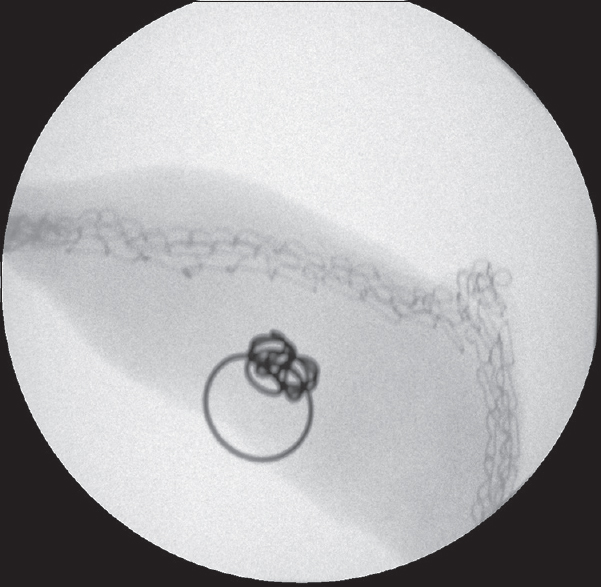
- Surgically resected wedge of the lung containing the microcoil.
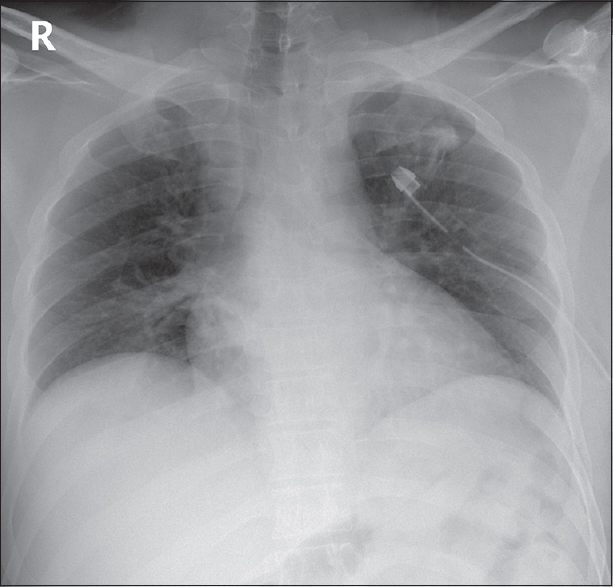
- Postoperative chest image showing left-sided chest tube.
MICROCOIL MISPLACEMENT
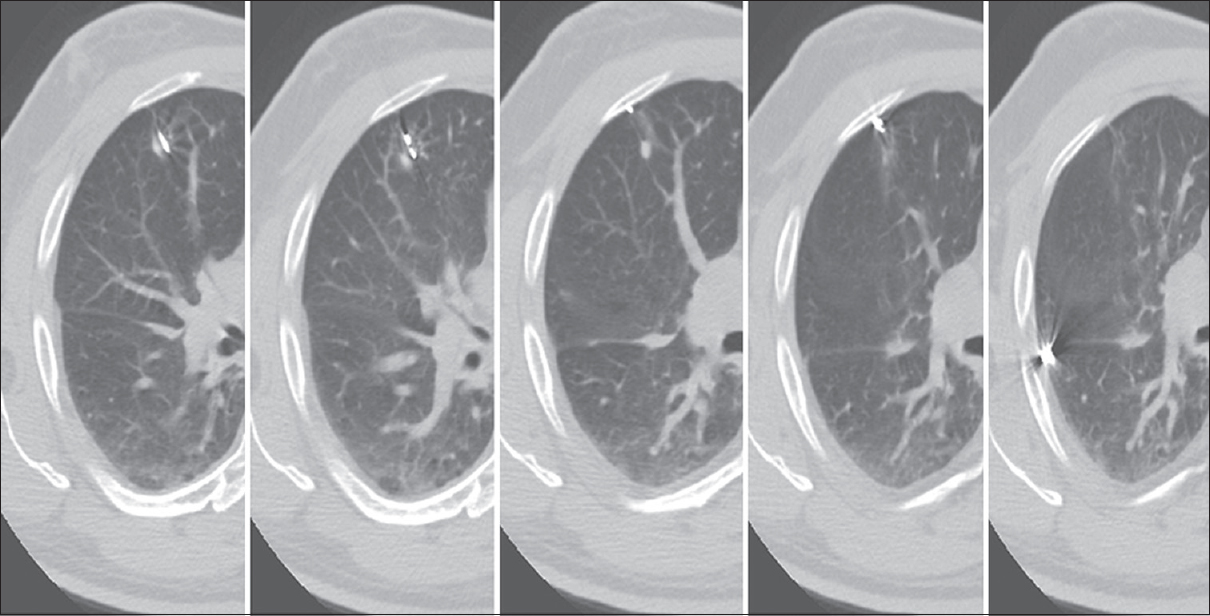
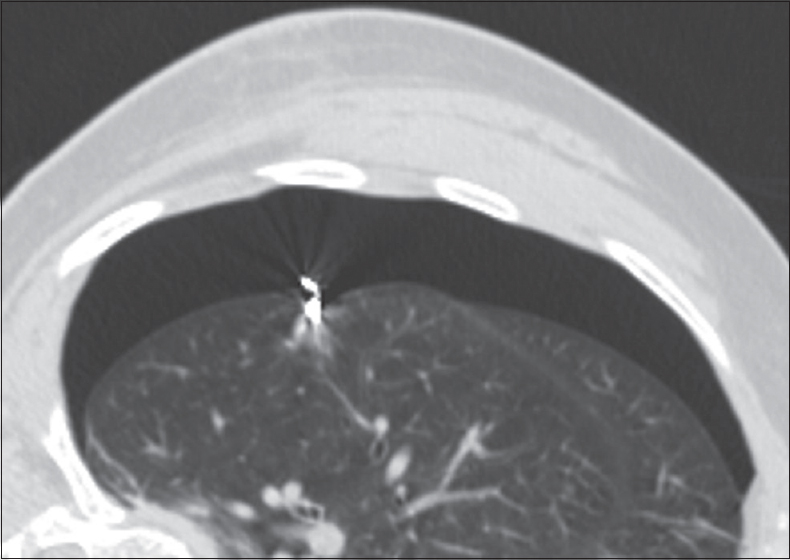
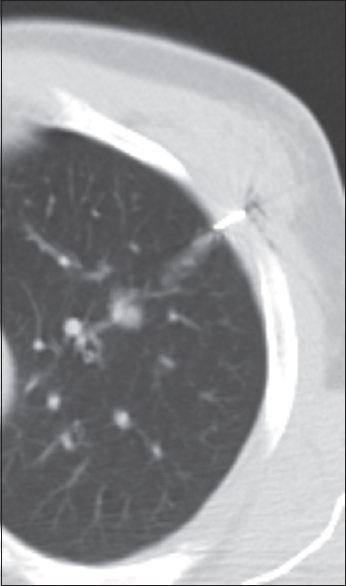
Ideal microcoil placement requires proper predeployment measurements and frequent CT scanning for needle placement and withdrawal guidance. There are two crucial steps to avoid microcoil misplacement: first, good deep anchoring of distal microcoil end to avoid dislodgment and second, CT scan guidance for needle withdrawal to deploy proximal microcoil end on the pleural surface and to avoid chest wall or lung parenchymal misplacement. Although the microcoil is ideally placed through the nodule, it can be placed close to the nodule since the surgeon can see the relationship between the coil and the nodule on postlocalization CT scan [Figures 7 and 8]. Insufficient distal anchoring may allow the microcoil to be displaced into the chest wall or reformed in the pleural space [Figures 9 and 10]. Placement of the proximal end of microcoil on the pleural surface is done under CT guidance. Therefore, the microcoil can be misplaced in the chest wall or completely placed in the lung parenchyma [Figures 11 and 12].[56] Subpleural nodules are often pushed away rather than transgressing by needle. Thus, if microcoil is deployed, it will retract on the plural surface after needle withdrawal [Figure 13].[9]
- Microcoil placed just adjacent to the pulmonary nodule.
- Microcoil placed about 1 cm beside the pulmonary nodule.
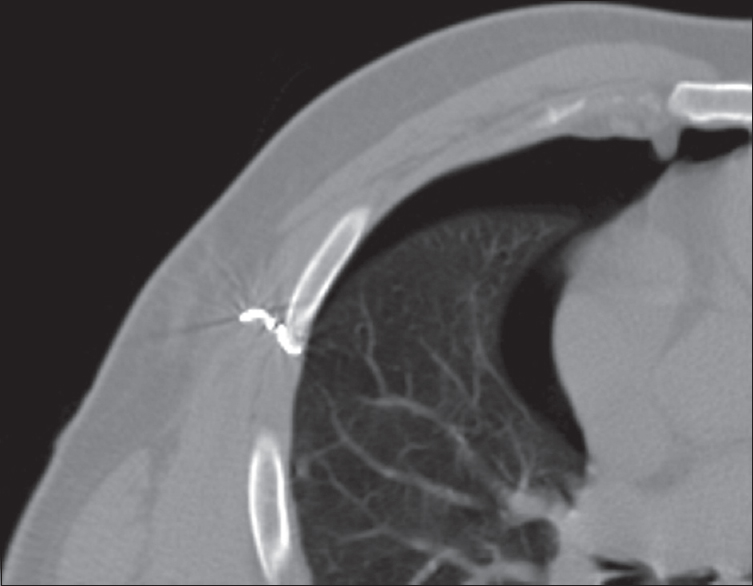
- Microcoil misplaced completely within the chest wall. Moderate amount of pneumothorax is noted.
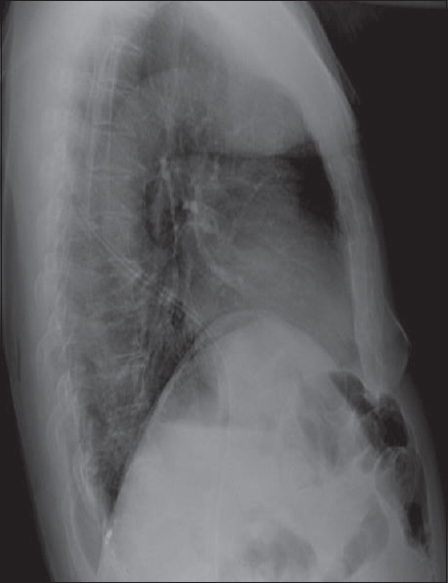
- Lateral chest X-ray showing the microcoil fallen into the pleural space at the posterior costophrenic angle.
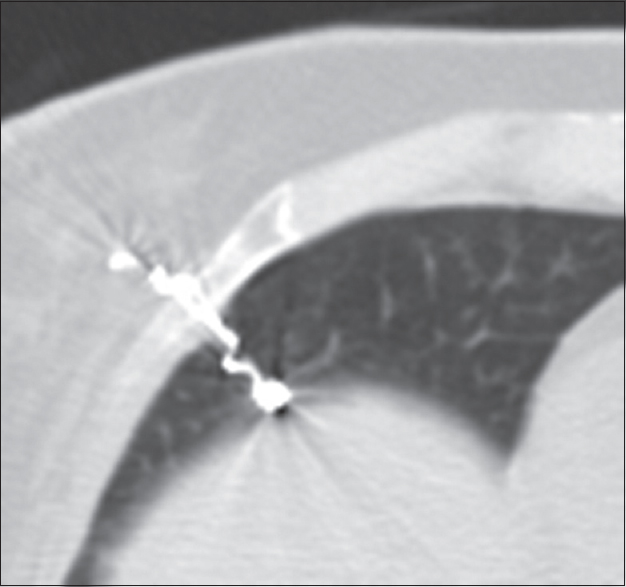
- Proximal microcoil end misplaced into the chest wall.
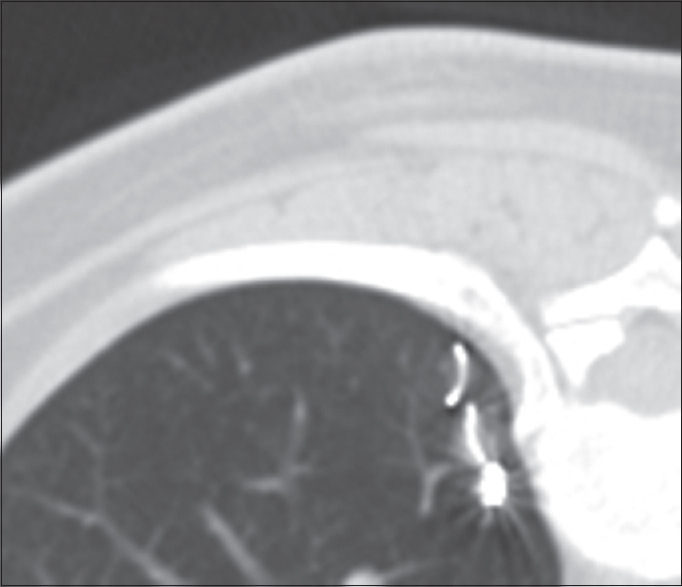
- Microcoil misplaced completely within the lung parenchyma.
- Chiba needle tip pushed the pulmonary nodule. After deploying the microcoil and withdrawing the needle, it retracted into the pleural surface and fell in the pleural cavity laterally.
In case of misplacement, surgeons could adjust the thoracoscopic surgery by knowing the relationship of the microcoil location to the nodule on postplacement CT scan. Surgeons can also adjust by removing the misplaced proximal end from the chest wall before deflating the lung or using the fluoroscopy for misplaced microcoil placed completely inside the lung parenchyma. In case of complete dislodgment, another microcoil could be placed properly. Misplaced microcoil in the chest wall, plural space, or lung parenchyma could be removed during surgery or kept in place and is associated with little damage.[56]
MICROCOIL PLACEMENT COMPLICATIONS
CT-guided microcoil localization results in a similar complication profile and rate as has been reported for CT-guided, fine-needle aspiration biopsy, mainly pneumothorax and hemorrhage. Emphysema is a well-known risk factor of increased risk for pneumothorax during percutaneous lung microcoil placement, and CT-guided, fine-needle aspiration biopsy that if symptomatic may necessitate insertion of a chest tube [Figure 14].[691011] Postprocedural hemorrhage is manifested by new airspace consolidation [Figure 15]. Wires in the chest wall are not associated with increased patient discomfort or pain.[5]
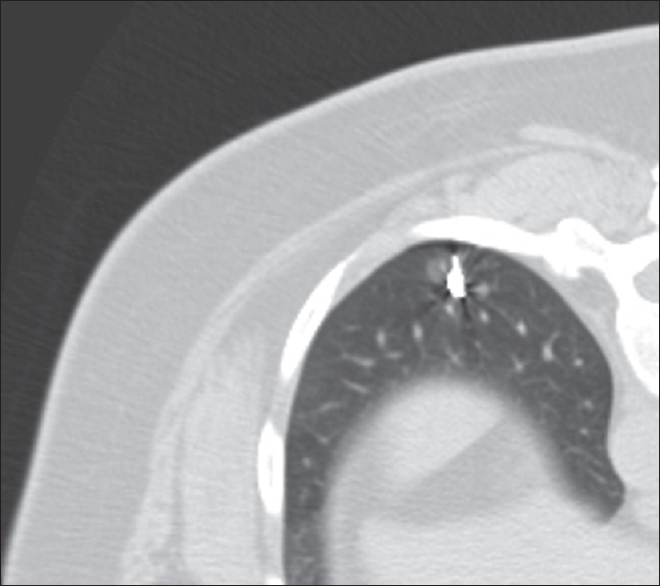
- Postlocalization computed tomography image demonstrates moderate amount of pneumothorax.
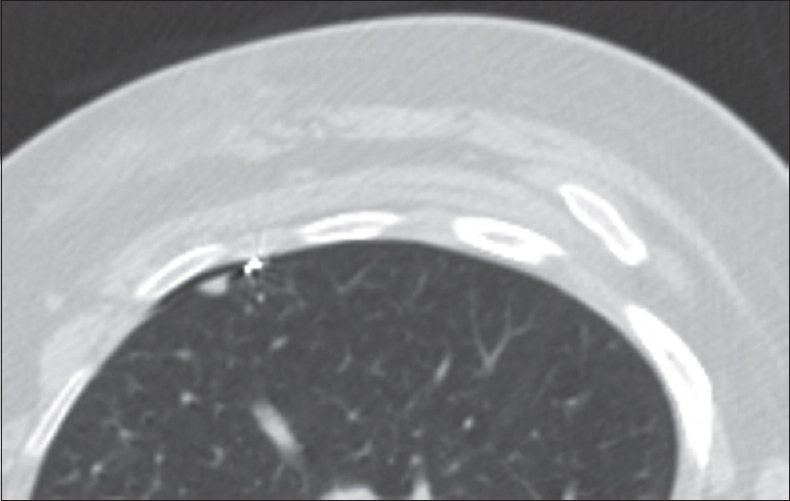
- Postlocalization computed tomography image demonstrates mild parenchymal lung hemorrhage in the tract of microcoil localization needle.
CONCLUSION
VATS is diagnostic and therapeutic of small pulmonary nodules. Preoperative pulmonary nodule localization is required to decrease the rate of conversion to thoracotomy. Various localization techniques were described in the literature. Microcoil localization to fluoroscopically guided VATS excision of small lung nodules increased its success rate of excision.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/8/227043.
REFERENCES
- Percutaneous localisation of pulmonary nodules prior to video-assisted thoracoscopic surgery using methylene blue and TC-99. Eur J Cardiothorac Surg. 2010;37:237-8.
- [Google Scholar]
- Video-assisted thoracoscopic resection of a small pulmonary nodule after computed tomography-guided localization with a hook-wire system. Experience in 45 consecutive patients. World J Surg. 2007;31:575-8.
- [Google Scholar]
- Video-assisted thoracoscopic surgery for small indeterminate pulmonary nodules: Indications for preoperative marking. Chest. 1999;115:563-8.
- [Google Scholar]
- Preoperative localization of small pulmonary lesions with a short hook wire and suture system: Experience with 168 procedures. Radiology. 2002;225:511-8.
- [Google Scholar]
- Lung nodules: CT-guided placement of microcoils to direct video-assisted thoracoscopic surgical resection. Radiology. 2009;250:576-85.
- [Google Scholar]
- Peripheral lung nodules: Fluoroscopically guided video-assisted thoracoscopic resection after computed tomography-guided localization using platinum microcoils. Ann Surg. 2004;240:481-8.
- [Google Scholar]
- Computed tomography guided microcoil localization for pulmonary small nodules and ground-glass opacity prior to thoracoscopic resection. J Thorac Dis. 2015;7:1580-7.
- [Google Scholar]
- Percutaneous localization of pulmonary nodules prior to thoracoscopic surgery by CT-guided hook-wire. Anticancer Res. 2006;26:3123-6.
- [Google Scholar]
- Percutaneous lung biopsy: Technique, efficacy, and complications. Semin Intervent Radiol. 2013;30:121-7.
- [Google Scholar]
- Transthoracic needle aspiration biopsy: Variables that affect risk of pneumothorax. Radiology. 1999;212:165-8.
- [Google Scholar]
- Transthoracic needle biopsy: Factors effecting risk of pneumothorax. Eur J Radiol. 2003;48:263-7.
- [Google Scholar]






