Translate this page into:
Computed Tomography-based Diagnosis of Post-laparoscopic Sleeve Gastrectomy Gastric Leak

*Corresponding author: Sultan R. Alharbi, Department of Radiology, College of Medicine, King Saud University, P.O. Box 145111, Riyadh 4545, Saudi Arabia. drsultan000@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Alharbi SR. Computed tomography-based diagnosis of post-laparoscopic sleeve gastrectomy gastric leak. J Clin Imaging Sci 2020;10:8.
Abstract
Objective:
Gastric leak post-laparoscopic sleeve gastrectomy may appear as a variety of computed tomography (CT) findings. We aimed to review the various CT findings sensitivity and specificity in confirmed cases of gastric leak.
Materials and Methods:
A retrospective review was performed for all patients who underwent sleeve gastrectomy, CT, and endoscopy for suspected leak between 2011 and 2018. All patients with positive CT findings for gastric leak were included in the study.
Results:
A total of 152 consecutive patients underwent CT for suspected post-sleeve gastrectomy gastric leak. Out of 152 patients, 88 had positive CT findings for gastric leak and underwent endoscopy. The CT findings sensitivity and specificity of perigastric collection without oral contrast leak were 61% and 88.8%, oral contrast leak were 28% and 100%, and gas leak were 10% and 77.7%, respectively.
Conclusions:
Perigastric fluid collection without contrast leak and with variable wall enhancement and gas content is the most common CT findings of post-sleeve gastrectomy gastric leak. Among various CT findings, it exhibits good diagnostic accuracy with 61% sensitivity and 88.8% specificity.
Keywords
Gastric leak
Laparoscopic sleeve gastrectomy
Computed tomography
INTRODUCTION
Laparoscopic sleeve gastrectomy is by far the most performed bariatric surgery worldwide. Its widespread adoption is due to its simplicity and excellent weight reduction outcomes, compared to more invasive bariatric surgeries requiring gastrointestinal anastomoses.[1-6] Although uncommon, post-sleeve gastrectomy gastric leak is the most feared complication due to its morbidity and the need for prolonged hospital stay, extensive resource use, and multidisciplinary team management.[2,5,7]
Imaging is an important diagnostic tool for the evaluation of post-operative complications in clinically suspected symptomatic patients. However, the value of its routine use in the early post- operative period is controversial.[8,9] Multiple studies investigating routine post-operative upper gastrointestinal contrast studies performed before patient discharge did not reveal any value of early gastric leak detection.[10-12] Routine early computed tomography (CT) using an oral contrast agent done on post-operative day 2 also has a limited role in the detection of asymptomatic gastric leak due to the fact that gastric leak usually occurs 1–2 weeks post-sleeve gastrectomy.[13] Normal post-operative CT shows a residual gastric sleeve with a staple line along with the transaction site. No contrast leak, gas leak or collection in contact with the staple line [Figure 1].[8] This study aimed to review the various CT findings sensitivity and specificity in patients with confirmed post-sleeve gastrectomy gastric leak.

- A 29-year-old female patient presented with abdominal pain, enhanced axial computed tomography image showing a normal post-operative gastric sleeve filled with oral contrast. No extraluminal gas or contrast. No perigastric fluid collection.
MATERIALS AND METHODS
Study design
The data from patients who underwent sleeve gastrectomy and presented with a suspected gastric leak at our institution between September 2011 and September 2018 were retrospectively reviewed. Our institution is the center of excellence for bariatric surgery and the primary referral site for gastric leak in the country. The Institutional Review Board approval was obtained. Given the retrospective nature of this study and the use of anonymized patient data, the requirement for obtaining informed consent was waived.
The patients who underwent sleeve gastrectomy, had positive CT findings, and underwent confirmation by endoscopy were included in the study. Endoscopy is performed at our institution after CT diagnosis of gastric leak for stent placement. Individuals with negative CT findings for gastric leak or did not undergo endoscopy were excluded as well as those who underwent invasive procedure(s) for gastric leak management before CT (surgery, surgical, percutaneous or endoscopic drainage, and endoscopic stenting).
CT protocol
Patients undergoing abdominal CT were administered 1 cup (approximately 60 ml) of water-soluble oral contrast while on the CT table followed by 80–100 ml of intravenous (IV) contrast. The amount of oral contrast on CT is reduced from 1 L over 1 to 2 h on routine abdominal CT to 60 ml on the CT table since the procedure aims to evaluate esophagus and stomach leak, and post-sleeve gastrectomy patients cannot tolerate large fluid volumes. CT data acquisition was performed in one portal venous phase 70 s after IV contrast injection, with slice thickness of 2 mm. The coronal and sagittal reformatted images along with the axial images were prepared for radiological interpretation. All CT studies were performed using the GE LightSpeed VCT 64-slice CT scanner (GE Healthcare, USA).
RESULTS
Of 152 consecutive symptomatic patients who underwent CT for suspected post-sleeve gastrectomy gastric leak, a total of 88 patients were included (38 women and 50 men; mean age, 34 years; mean body mass index 46 kg/m2) with CT findings positive for gastric leak after sleeve gastrectomy confirmed by endoscopy and without previous invasive intervention for such leaks. Positive CT findings included oral contrast leak, gas leak only, and perigastric fluid collection. Out of 88 patients, 8 patients (2 gas leaks and 6 perigastric fluid collections) had negative endoscopy for gastric leak. The sensitivity and specificity of these findings are summarized in Table 1.
| Findings | Sensitivity | Specificity |
|---|---|---|
| Contrast leak | 28% (25/88) | 100% (25/25) |
| Gas leak | 10% (9/88) | 77.7% (7/9) |
| Perigastric fluid collection without contrast leak | 61% (54/88) | 88.8% (48/54) |
CT: Computed tomography
Contrast leak was detected along the gastroesophageal junction in 28% (25 of 88) of patients with 100% specificity [Figure 2]. Gas leak only was detected adjacent to stable line of proximal gastric pouch in 10% (9 of 88) of patients with 77.7% specificity [Figure 3]. Perigastric fluid collection without oral contrast leak was found in 61% (54 of 88) of patients with 88.8% specificity, mainly at the proximal gastric pouch [Figure 4]. Other complications seen in our patients are post-operative intra-abdominal hematoma (5/152), splenic infarction (9/152), and portal vein thrombosis (6/152).

- A 25-year-old male patient presented with repeated vomiting, enhanced axial computed tomography scan image showing oral contrast leak with gas contrast level.
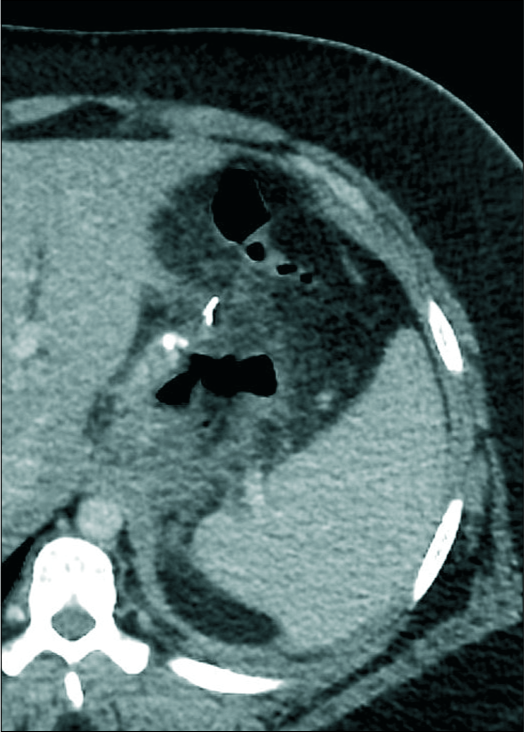
- A 34-year-old female patient presented with the left shoulder and chest pain, enhanced computed tomography scan image showing a gas leak only adjacent to the proximal gastric ruminant pouch.
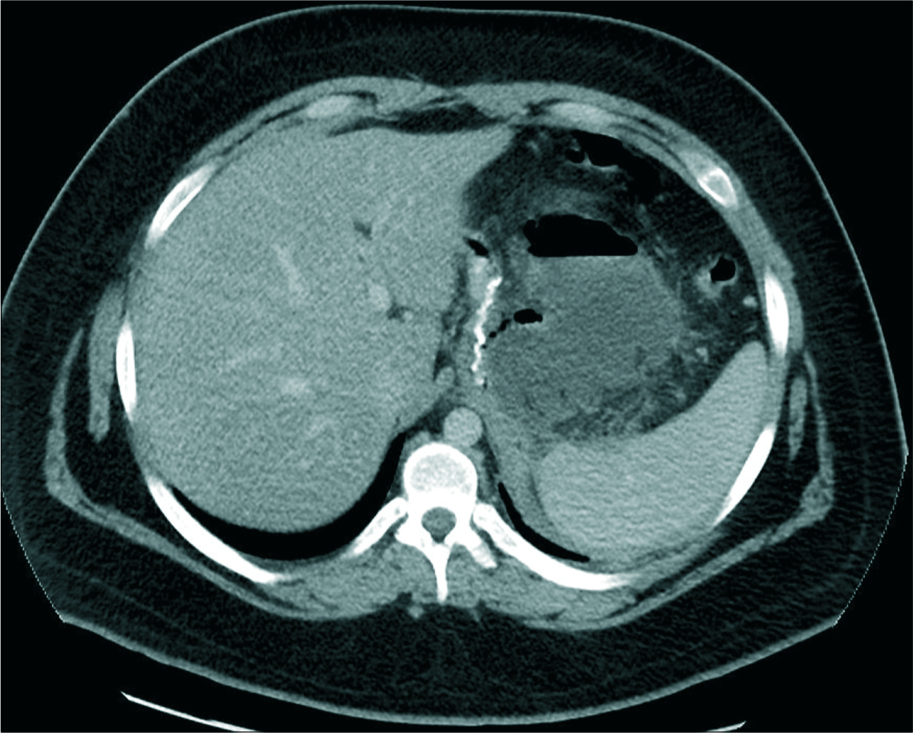
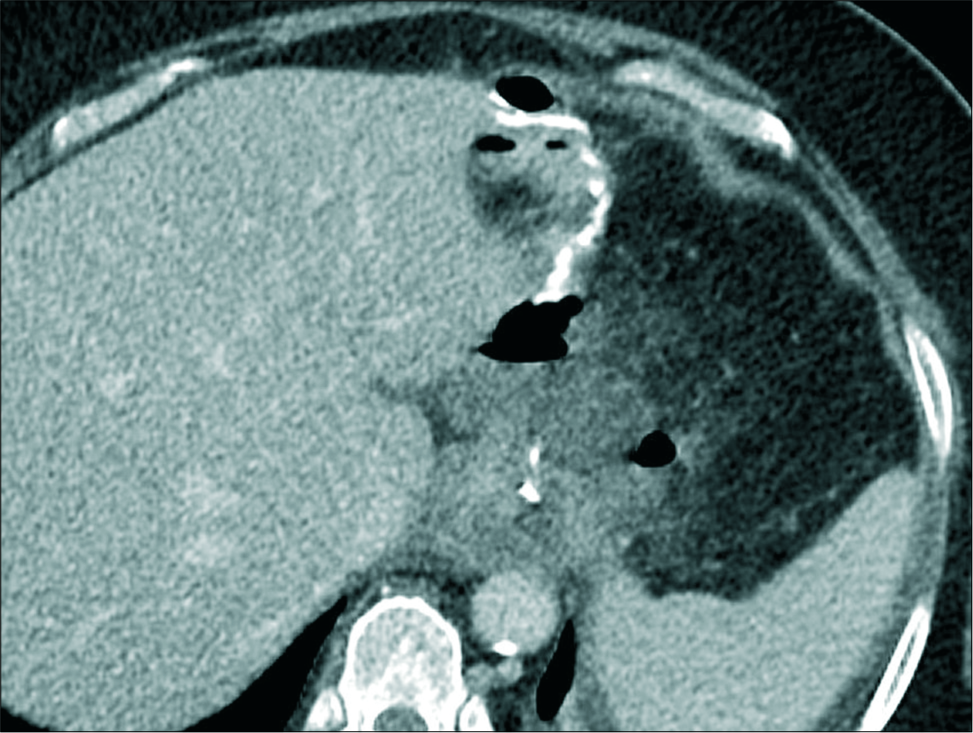
- A 19-year-old male patient presented with fever, enhanced axial computed tomography scan image showing perigastric collection without oral contrast leak with a gas fluid level and enhancing wall.
DISCUSSION
Early detection of gastric leak is crucial because it enables early management, leads to decreased morbidity, and improves patient outcomes.[6,13-15] A high clinical index of suspicion is the most sensitive approach to detect gastric leak.[16-18] The clinical presentation is highly variable, ranging from asymptomatic to septic shock.[19] However, tachycardia, fever, and abdominal or left shoulder pain are the most common clinical signs.[20]
Abdominal CT with IV and oral contrast in patients with suspected gastric leak is the best diagnostic tool not only for gastric leaks but also to detect associated complications and to generate other differential diagnoses.[21] To the best of our knowledge, there are few published articles describing the CT findings of post-sleeve gastrectomy gastric leak; these are mainly review articles. A few original articles exist, but these have small patient numbers due to the rare incidence ranging from 1% to 3%. The described CT findings suggestive of gastric leak in the literature include contrast leak, gas leak, staple line defects, and perigastric collection.[8,22-24]
In the largest available published study, Chivot et al. described the CT findings of post-sleeve gastrectomy gastric leak in 30 patients, perigastric abscess without contrast material leak in 17 patients (56.6%), contrast material leak in 5 patients (16.7%), gas leak without contrast material leak in 3 patients (10%), perigastric hematoma containing gas in 3 patients (10%), and blind gastric fistulas in 2 patients (6.7%).
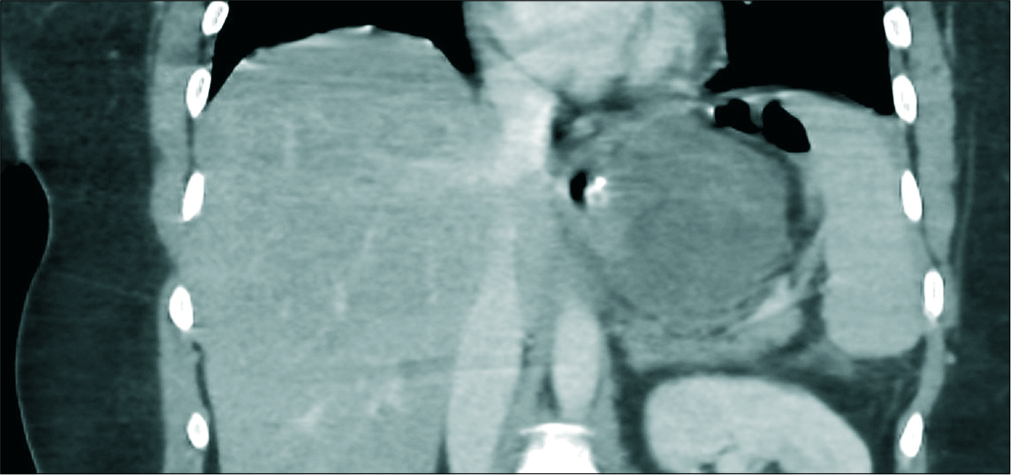
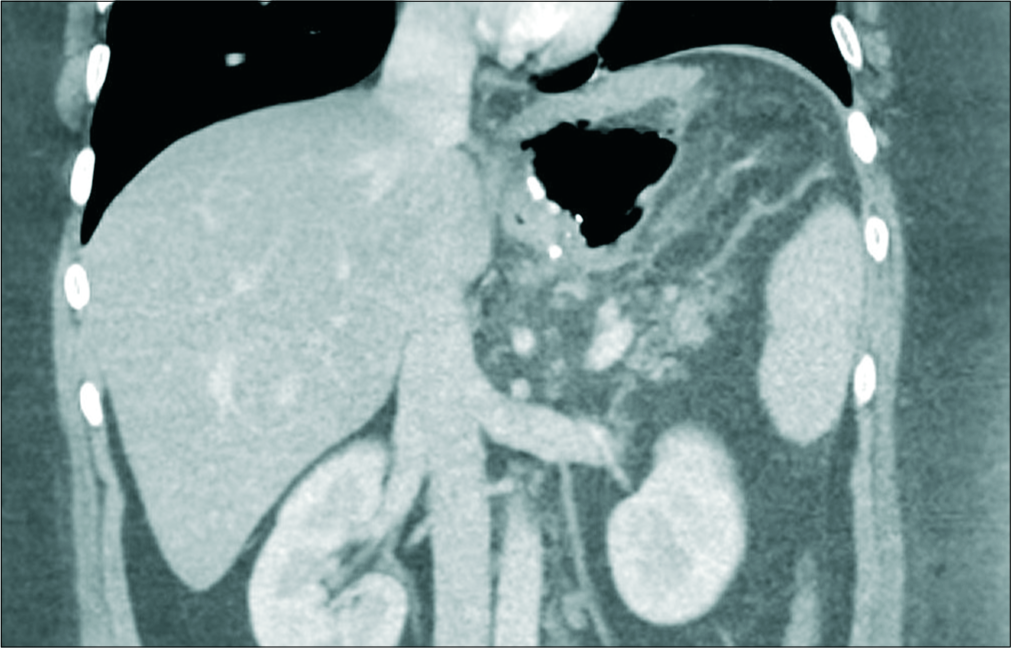
Our study examined the largest patient’s cohort including 88 patients, in whom gastric leak was confirmed by endoscopic examination while inserting an endoluminal stent. Among our cases, the most common finding was perigastric collection without contrast leak 61% (54/88) patients with 88.8% specificity, showing a variable amount of gas and peripheral contrast enhancement [Figures 5 and 6]. Although perigastric fluid collection classically shows enhancing wall and contains gas, it was often seen without enhancing wall or gas in our study [Figures 7 and 8]. For that reason, perigastric fluid collection adjacent to the gastric sleeve staple line should be recognized and treated as a gastric leak. Gas only leak is the least common findings 10% (9/88) of patients with 77.7% specificity. Gas leak in contrast to expected postoperative gas – which is seen in non-dependent upper abdomen – is seen along the stable line of residual gastric sleeve [Figures 9 and 10]. Gas leak is mostly due to minute and early gastric leak. Contrast leak was detected in only 28% (25 of 88) of patients with 100% specificity. There are several possible explanations for this observation, including the presence of a small gastric leak, fast passage, insufficient volume of ingested contrast material, and compression of the gastric pouch by a previously formed collection.[22]

- A 46-year-old male patient presented with abdominal pain and tachycardia, enhanced coronal computed tomography image showing perigastric fluid collection with a small amount of gas and well-defined enhancing wall.

- A 26-year-old male patient presented with tachycardia, enhanced axial CT image showing large perigastric fluid collection with multiple air pockets displacing the gastric remnant anteriorly.
- A 34-year-old male patient presented with tachycardia, enhanced axial computed tomography image showing perigastric fluid collection without an enhancing peripheral wall or gas.
- A 60-year-old male patient presented with repeated vomiting, an enhanced axial computed tomography image showing perigastric fluid collection associated with fat stranding and a small pocket of air but no enhancing peripheral wall.
- A 30-year-old male patient presented with the left shoulder pain and vomiting, enhanced coronal CT image showing extraluminal large gas pocket adjacent to gastric sleeve indicating a gas leak.

- A 29-year-old male patient developed tachycardia and abdominal pain immediately after sleeve gastrectomy surgery, enhanced axial CT image showing post-operative expected multiple small air pockets in the non-dependent upper abdomen. No gas pocket has seen adjacent to gastric sleeve.
The limitations of the present study include its retrospective design and the fact that most of our patients were referred relatively late from another institution.
CONCLUSIONS
Perigastric fluid collection without contrast leak and with variable wall enhancement and gas content is the most common CT findings of post-sleeve gastrectomy gastric leak. Among various CT findings, it exhibits good diagnostic accuracy with 61% sensitivity and 88.8% specificity.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on justified request.
References
- Diagnosis and management of gastric leaks after laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg. 2010;20:403-9.
- [CrossRef] [PubMed] [Google Scholar]
- Gastric leaks post sleeve gastrectomy: Review of its prevention and management. World J Gastroenterol. 2014;20:13904-10.
- [CrossRef] [PubMed] [Google Scholar]
- Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23:427-36.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg. 2010;252:319-24.
- [CrossRef] [PubMed] [Google Scholar]
- Survey on laparoscopic sleeve gastrectomy (LSG) at the fourth international consensus summit on sleeve gastrectomy. Obes Surg. 2013;23:2013-7.
- [CrossRef] [PubMed] [Google Scholar]
- Sleeve gastrectomy and the risk of leak: A systematic analysis of 4,888 patients. Surg Endosc. 2012;26:1509-15.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of leaks following sleeve gastrectomy by endoscopic internal drainage (EID) Obes Surg. 2015;25:1293-301.
- [CrossRef] [PubMed] [Google Scholar]
- Laparoscopic sleeve gastrectomy: A radiological guide to common postsurgical failure. Can Assoc Radiol J. 2018;69:184-96.
- [CrossRef] [PubMed] [Google Scholar]
- ASMBS position statement on prevention, detection, and treatment of gastrointestinal leak after gastric bypass and sleeve gastrectomy, including the roles of imaging, surgical exploration, and nonoperative management. Surg Obes Relat Dis. 2015;11:739-48.
- [CrossRef] [PubMed] [Google Scholar]
- Upper gastrointestinal swallow study following bariatric surgery: Institutional review and review of the literature. Obes Surg. 2012;22:1039-43.
- [CrossRef] [PubMed] [Google Scholar]
- Is routine postoperative gastrografin study needed after laparoscopic sleeve gastrectomy? Experience of 712 cases. Obes Surg. 2013;23:1711-7.
- [CrossRef] [PubMed] [Google Scholar]
- Routine upper gastrointestinal swallow studies after laparoscopic sleeve gastrectomy are unnecessary. Am J Surg. 2014;207:897-901.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective evaluation of routine early computed tomography scanner in laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016;12:1483-90.
- [CrossRef] [PubMed] [Google Scholar]
- The utility of routine postoperative upper gastrointestinal swallow studies following laparoscopic sleeve gastrectomy. Obes Surg. 2014;24:1415-9.
- [CrossRef] [PubMed] [Google Scholar]
- C-reactive protein, white blood cells, and neutrophils as early predictors of postoperative complications in patients undergoing laparoscopic sleeve gastrectomy. Surg Endosc. 2013;27:864-71.
- [CrossRef] [PubMed] [Google Scholar]
- Management of leaks after laparoscopic sleeve gastrectomy in patients with obesity. J Gastrointest Surg. 2010;14:1343-8.
- [CrossRef] [PubMed] [Google Scholar]
- Back to basics--Clinical diagnosis in bariatric surgery. Routine drains and upper GI series are unnecessary. Surg Endosc. 2007;21:2268-71.
- [CrossRef] [PubMed] [Google Scholar]
- The utility of radiological upper gastrointestinal series and clinical indicators in detecting leaks after laparoscopic sleeve gastrectomy: A case-controlled study. Surg Endosc. 2016;30:2266-75.
- [CrossRef] [PubMed] [Google Scholar]
- New CT scan classification of leak after sleeve gastrectomy. Obes Surg. 2013;23:1341-3.
- [CrossRef] [PubMed] [Google Scholar]
- Gastric leak after laparoscopic-sleeve gastrectomy for obesity. Obes Surg. 2009;19:1672-7.
- [CrossRef] [PubMed] [Google Scholar]
- Eliminating routine upper gastrointestinal contrast studies after sleeve gastrectomy decreases length of stay and hospitalization costs. Surg Obes Relat Dis. 2017;13:553-9.
- [CrossRef] [PubMed] [Google Scholar]
- Value of routine upper gastrointestinal swallow study after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2017;13:758-65.
- [CrossRef] [PubMed] [Google Scholar]
- Multidetector CT imaging of bariatric surgical complications: A pictorial review. Abdom Radiol (NY). 2016;41:174-88.
- [CrossRef] [PubMed] [Google Scholar]
- Laparoscopic sleeve gastrectomy: Imaging of normal anatomic features and postoperative gastrointestinal complications. Diagn Interv Imaging. 2013;94:823-34.
- [CrossRef] [PubMed] [Google Scholar]






