Translate this page into:
Comparative Performances of Dipyridamole and Regadenoson to Detect Myocardial Ischemia using Cardiac Cadmium-Zinc-Telluride Single-Photon Emission Computerized Tomography
Address for correspondence: Dr. Fayçal Ben Bouallègue, Department Nuclear Medicine, Montpellier University Hospital, 371 Av. du Doyen Gaston Giraud, 34090 Montpellier, France. E-mail: faybenb@hotmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
We evaluated the relative performances of dipyridamole (Dip) and regadenoson (Reg) in a cohort of patients referred for coronary artery disease diagnosis or follow-up using myocardial perfusion imaging.
Materials and Methods:
We retrospectively included 515 consecutive patients referred for 99mTc-sestamibi myocardial perfusion single-photon emission computerized tomography (SPECT) on a cadmium-zinc-telluride (CZT) camera after pharmacologic stress. About three quarters (n = 391, 76%) received Dip. Reg was administrated to patients with chronical respiratory disease or with body mass index (BMI) over 38 kg/m2 (n = 124, 24%). Patients with an abnormal stress scan (92%) underwent a rest imaging on the same day. Qualitative interpretation of perfusion images was achieved using QPS software, and the ischemic area was assessed using the 17-segment model. In patients undergoing a stress-rest protocol, perfusion polar plots were postprocessed using automated in-house software to quantify the extension, intensity, and location of the reversible perfusion defect. Statistical comparison between groups was performed using univariate and multivariate analysis.
Results:
Qualitative analysis concluded to myocardial ischemia in 70% of the patients (69% in the Dip group, 76% in the Reg group, P = ns). In those patients, the number of involved segments (Dip 2.5 ± 1.6, Reg 2.7 ± 1.6, P = ns) and the proportion of patients with an ischemic area larger than two segments (Dip 30%, Reg 37%, P = ns) were comparable. Automated quantification of the reversible perfusion defect demonstrated similar defect extension, intensity, and severity in the two groups. Defect location was identical at the myocardial segment and vascular territory scales.
Conclusions:
Reg and Dip showed equal performances for ischemic burden characterization using myocardial CZT SPECT.
Keywords
Cadmium-zinc-telluride camera
dipyridamole
myocardial perfusion single-photon emission computerized tomography
pharmacologic stress
regadenoson

INTRODUCTION
Myocardial perfusion imaging (MPI) by means of single-photon emission computerized tomography (SPECT) using 99mTc-labeled tracers is a reference tool for diagnosing and monitoring coronary artery disease (CAD).[1] Pharmacologic stress is performed whenever the patient cannot exercise, cannot achieve adequate exercise end points, or has a left bundle branch block or electronically paced rhythm.[23] Dipyridamole (Dip) is a nonselective adenosine agonist that has been widely employed since the mid90s as a vasodilator stress agent owing to its satisfying tolerance profile, adapted pharmacokinetic characteristics, and affordability.[4] Regadenoson (Reg) is a selective A2a adenosine agonist available for stress MPI.[567] Its advantages over nonselective agonists include less side effects,[8] quick injection, a fixed dose of 400 μg independent of patient's weight,[9] and a prompt hyperemic response,[6] which translates into the higher efficiency of use and patient and clinician satisfaction.[1011] Several studies have explored the relative performances of Dip and Reg in the frame of myocardial perfusion positron emission tomography (PET) using 82Rb or 13N-ammonia. Most studies concluded to the equivalency of the results obtained with both vasodilator agents in terms of total perfusion deficit and left ventricular function,[12] as well as absolute myocardial blood flow and flow reserve.[1314] In a recent study, Johnson and Gould reported a slightly reduced hyperemic flow using Reg (80%–90% depending on tracer injection timing) compared to Dip.[15] Conversely, using magnetic resonance imaging, Vasu et al. found minimal superiority of Reg in terms of vasodilator efficacy.[16] As concerns SPECT MPI, although Reg has been proved to yield similar diagnostic information compared to adenosine,[817] no systematic analysis of the relative performances of Reg and Dip has been carried out to date. The aim of the present study was to explore these relative performances in a retrospective cohort of patients referred for pharmacologic SPECT MPI on a dedicated cardiac cadmium-zinc-telluride (CZT) camera.[18] Stress and rest perfusion images obtained using standard commercial software were qualitatively rated by expert physicians, then postprocessed in a fully automated way to quantify the reversible perfusion defect in terms of location, extension, and intensity.
MATERIALS AND METHODS
Patient population
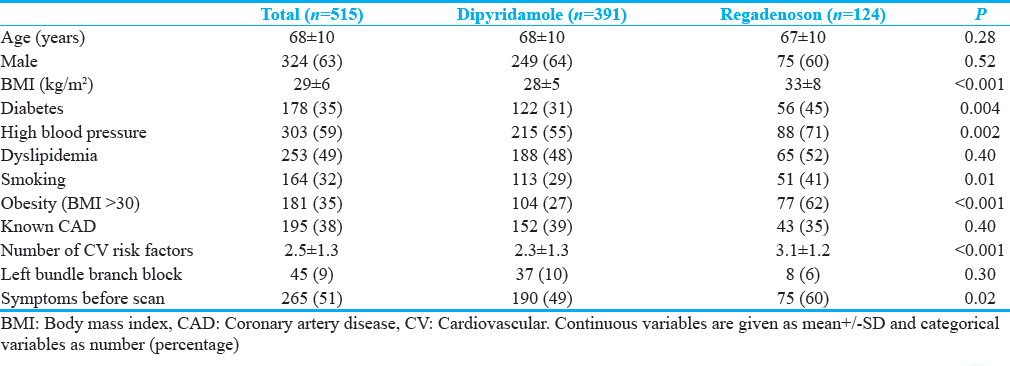
A retrospective study was conducted in outpatients with known or suspected CAD referred to the nuclear medicine department at Caen University Hospital from June to August 2016 for myocardial perfusion evaluation after pharmacologic stress. This study was approved by the local ethics committee, and the requirement for individual informed consent was waived. Five hundred and fifteen consecutive patients were included aged 68 ± 10 years, among which 265 (51%) were symptomatic and 195 (38%) had a known history of documented CAD. The clinical characteristics of the study population are summarized in Table 1. Pharmacologic stress was performed using Dip in 391 patients (76%) and Reg in 124 patients (24%).
Pharmacologic stress
Patients were asked to refrain from caffeine and methylxanthine-containing substances and drugs for at least 24 h before their scan. In the absence of contraindication, vasodilator stress was performed using Dip which was administrated through a slow IV injection of 0.56 mg/kg over 4 min. Radiopharmaceutical injection was performed 7 min after the beginning of the Dip infusion. Reg was used in patients suffering from asthma, chronic obstructive pulmonary disease, or respiratory failure from any cause (including pulmonary hypertension). Due to its administration at a fixed-dose independent of patient's weight, Reg was also used in patients with a body mass index (BMI) equal or exceeding 38 kg/m2. Reg was administrated through rapid IV injection over 10 s at a fixed dose of 400 μg. Radiotracer injection was performed 20 s after Reg injection.
Single-photon emission computerized tomography acquisition and expert reading
All SPECT acquisitions were carried out using a dedicated CZT cardiac SPECT camera (D-SPECT; Spectrum Dynamics, Biosensors, Caesarea, Israel) with the patient in the upright position. Stress acquisition was performed within 20 min after IV injection of 2.5 MBq/kg of 99mTc-sestamibi. If necessary, rest acquisition was performed 90 min later using 7 MBq/kg of 99mTc-sestamibi. Acquisition was stopped when 800 103 counts were recorded in a cardiac volume of interest encompassing the whole heart. Tomographic images were reconstructed using the manufacturer's dedicated software and postprocessed using commercially available software (QPS, Cedars-Sinaï Medical Center, Los Angeles, CA, USA).[19] Qualitative assessment was carried out jointly by two expert physicians (DA and AM) who concluded consensually to the absence or the presence of an ischemic area which extent was described in terms of the number of myocardial segments involved using the standard 17-segment nomenclature.[20] Myocardial scar from prior infarction was defined as the presence of a significant nonreversible perfusion defect along with clinical arguments (known prior myocardial infarction), electrical anomalies (Q wave), or functional anomalies (regional hypokinesia at echography or gated SPECT).
Automated postprocessing
In patients who underwent both stress and rest imaging, the polar plots of the relative perfusion map provided by QPS for rest and stress studies were exported to in-house software allowing automated accurate quantification of the reversible perfusion defect. The reversibility map was computed as the difference between rest and stress relative perfusion polar plots. Based on a five-point scale,[221] the reversible perfusion defect was defined as the area which reversibility was above 10% and a stress relative perfusion below 70%. Defect extension (in % of the myocardial surface) was computed on a pixel-basis postulating that each pixel accounts for the same proportion of the myocardial surface. Defect intensity (in %) was computed as the mean reversibility over the segmented area. Defect severity (in %) was defined as the product of defect extension by defect intensity. The partition of the reversible defect was evaluated by computing its number of connected components (components with a surface below 1% were discarded). Last, defect location was assessed in terms of myocardial segment and vascular territory. A myocardial segment was considered affected if the reversible defect covered at least one half of its surface. A vascular territory (left anterior descending artery, left circumflex artery [LCX], and right coronary artery [RCA]) was considered affected when at least one of its constitutive segments[20] was affected.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation. Categorical variables are described as number (percentage). Comparison between the two groups in terms of the observed clinical characteristics, technical parameters, and results of the qualitative assessment was performed using a Z-test, except the distributions of the number of ischemic segments that were compared through a Wilcoxon rank-sum test. The quantitative parameters provided by the automated reversible defect characterization and the distributions of affected segments and vascular territories were compared using a Wilcoxon rank-sum test. A two-sided P < 0.05 was regarded as statistically significant.
The influence of the potential confounding factors which distribution differed significantly between the two groups (number of cardiovascular [CV] risk factors, obesity defined as a BMI >30 kg/m2, and the presence of symptoms) was evaluated using a linear regression model. As regards the multivariate analysis, P values were corrected for multiple comparisons using the Dunn–Šidák correction: pcorrected= 1−(1 − p)m with m the number of comparisons (here we set m = 7 as the number of times the linear model was run).
Basic statistical computations were carried out using Excel (Microsoft, Redmond, WA). MATLAB R2013 (The MathWorks, Natick, MA) was used to infer probability density functions from data distributions and to perform linear regressions and Wilcoxon tests.
RESULTS
Among the 515 patients included, about three quarters (391, 76%) received Dip and one quarter (124, 24%) Reg. Symptom prevalence, BMI, and number of CV risk factors were significantly higher in the Reg group. Table 2 summarizes the technical details of the acquisitions and the results of the expert qualitative assessment. Eight percent of the patients had a normal stress MPI and did not require rest imaging (9% in the Dip group, 6% in the Reg group, P = ns), while 355 patients from the Dip group and 117 from the Reg group underwent a stress-rest protocol. Due to higher mean BMI, mean injected activities were significantly higher in the Reg group with comparison to the Dip group (235 vs. 207 MBq at stress, and 634 vs. 561 MBq at rest). However, due to the precount acquisition stopping condition, total reconstructed counts in the left ventricle did not differ between the two groups. Scar from prior myocardial infarction was identified in about one-sixth of the patients (15% in the Dip group, 18% in the Reg group, P = ns). Regarding the characterization of the ischemic burden, there was no significant difference between the two groups in terms of proportion of patients without ischemia (31% in the Dip group vs. 24% in the Reg group, P = ns). In patients with a significant reversible perfusion defect, the mean number of ischemic segments was similar in the two groups (2.5 in the Dip group vs. 2.7 in the Reg group, P = ns). Multivariate analysis did not reveal any influence of the potential confounding factors [

Supplemental Table 1
Supplemental Table 1 P values of the linear regression models
- Ischemic burden as characterized by visual assessment in each group. Left: proportion of participants without myocardial ischemia. Right: number of ischemic segments in participants with myocardial ischemia.
Table 3 summarizes the results provided by the automated quantification of the reversible perfusion defect. No significant difference was found between the two groups regarding the number of connected components, defect extension, intensity, and severity. After multivariate analysis, none of these quantitative parameters was significantly influenced by any of the potential confounding factors (number of CV risk factors, obesity, and presence of symptoms) [


- Automated quantification of the reversible perfusion defect in terms of number of connected components (top left), defect extension (top right), intensity (bottom left), and severity (bottom right). Curves stand for probability density distributions and are normalized as such (area under the curve = 1).
Figure 3 details the localization of the reversible perfusion defect. The histograms of defect location in terms of affected myocardial segment and vascular territory are shown on the left panel. Histograms are normalized to the total number of affected segments and territories, respectively. No significant association was found between segmental or territorial involvement and the employed pharmaceutical agent. The polar plots of the relative spatial distribution of the reversible perfusion defect after Dip (top) and Reg stress (bottom) are displayed on the right panel. Each polar plot was built up by computing, for every pixel, the number of patients in which that pixel was involved in a reversible defect. Each polar plot appears normalized to its own maximum.

- Automated localization of the reversible perfusion defect. Left: distribution according to the 17-segment division of the left ventricle (top) and to vascular territory (bottom). Histograms are normalized to the total number of affected segments and territories, respectively. Right: polar plots of the relative spatial distribution of the reversible defect after dipyridamole (top) and regadenoson (bottom). The gray level of a pixel reflects the proportion of patients in which the pixel was involved in a defect. Each polar plot is normalized to its own maximum.
DISCUSSION AND CONCLUSIONS
We systematically assessed the results of pharmacologic stress MPI based on both expert visual analysis and automated quantitative characterization, to evaluate the relative performances of Dip and Reg in a cohort of 515 consecutive outpatients referred for CAD diagnosis or follow-up. Owing to its safety of use in patients with chronic respiratory disease and to its administration at a fixed dose without adjustment to patient's weight, Reg was employed in our institution in almost one-fourth of the patients. In the present study, the two groups were homogeneous in terms of patient age, sex, and clinical history of CAD. Due to its administration to morbidly obese patients, BMI was higher in the Reg group, which likely explains the higher prevalence of diabetes and high blood pressure in that group. Smoking and prevalence of dyspnea were also naturally higher in the Reg group.
Our study has inherent limitations due to its retrospective design yielding two populations with unbalanced comorbidities and CV risk factors. A thorough evaluation of the relative performances of Dip and Reg should rely on the prospective assessment of stress MPI using both stress agents in each participant, which is hardly achievable in clinical routine due to practical and ethical considerations.
The ischemic burden as assessed qualitatively by expert visual interpretation, although slightly higher in the Reg group both in terms of percentage of patients with an ischemic area and in terms of number of ischemic segments, did not significantly differ between the two groups from a statistical point of view. Besides, the proportion of patients with an ischemic area involving more than two myocardial segments, which is a recognized cut-off value to guide revascularization,[22] was comparable using the two stress agents.
The relatively low proportion of normal scans (31% in the Dip group and 24% in the Reg group) may be attributed to the fact that patients referred for pharmacologic stress belong to a clinically higher risk population.[23] In a large meta-analysis of MPI studies dating from 1990 to 2001, Navare et al. highlighted a normalcy rate of 40% in the pharmacologic stress group.[24] The slightly lower rates reported in our cohort are likely related to the higher sensitivity of new dedicated CZT cameras compared to old generation cameras.
The automated postprocessing step was performed to cancel intraoperator and interoperator variability and to provide continuously distributed indices of perfusion reversibility independent of myocardial segmentation. Its result was highly coherent with those of the visual analysis in term of reversible defect extension since, based on a 17-segment partition of the myocardial wall, the mean extension corresponded to 2.3 ± 1.5 segments (vs. 2.5 ± 1.6 for visual assessment) using Dip and 2.6 ± 1.8 segments (vs. 2.7 ± 1.6) using Reg. Here again, the ischemic burden was minimally higher in the Reg group compared to the Dip group, both in terms of defect extension and severity but without statistical significance. As regards defect location, spatial distribution was similar in the two groups both at the myocardial segment and vascular territory scales, with a preferential localization in the inferior and inferolateral walls across the RCA and LCX territories.
The small differences observed between the two groups were likely related to a higher a priori probability of CAD in the Reg group that the regression model employed for multivariate analysis failed to highlight statistically due to the intrinsically multifactorial, tenuous, and nonlinear nature of the association. Yet, our results were concordant with those of previous studies comparing Dip and Reg using perfusion PET, showing slightly higher segmental defect scores[12] and stress flow and flow reserve in healthy[13] and pathologic participants[14] using Reg, without statistical significance. Larger studies based on multicentric cohorts using thorough patient stratification would allow to better determine the statistical significance of these differences and their association with the type of pharmacologic stress agent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/51/245533
REFERENCES
- Noninvasive assessment of myocardial perfusion. Circ Cardiovasc Imaging. 2009;2:412-24.
- [Google Scholar]
- EANM procedural guidelines for radionuclide myocardial perfusion imaging with SPECT and SPECT/CT: 2015 revision. Eur J Nucl Med Mol Imaging. 2015;42:1929-40.
- [Google Scholar]
- Pharmacology of coronary vasodilation: A brief review. J Nucl Cardiol. 1996;3:S27-30.
- [Google Scholar]
- Safety of dipyridamole testing in 73,806 patients: The multicenter dipyridamole safety study. J Nucl Cardiol. 1995;2:3-17.
- [Google Scholar]
- Regadenoson, a selective A2A adenosine receptor agonist, causes dose-dependent increases in coronary blood flow velocity in humans. J Nucl Cardiol. 2007;14:514-20.
- [Google Scholar]
- Selective adenosine agonists and myocardial perfusion imaging. J Nucl Cardiol. 2012;19:126-41.
- [Google Scholar]
- Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: Results of the ADVANCE phase 3 multicenter international trial. J Nucl Cardiol. 2007;14:645-58.
- [Google Scholar]
- Effects of age, gender, obesity, and diabetes on the efficacy and safety of the selective A2A agonist regadenoson versus adenosine in myocardial perfusion imaging integrated ADVANCE-MPI trial results. JACC Cardiovasc Imaging. 2008;1:307-16.
- [Google Scholar]
- Myocardial perfusion imaging laboratory efficiency with the use of regadenoson compared to adenosine and dipyridamole. J Med Econ. 2013;16:449-60.
- [Google Scholar]
- Patient- and clinician-reported satisfaction with pharmacological stress agents for single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) J Med Econ. 2013;16:828-34.
- [Google Scholar]
- Regadenoson pharmacologic rubidium-82 PET: A comparison of quantitative perfusion and function to dipyridamole. J Nucl Cardiol. 2013;20:76-83.
- [Google Scholar]
- Comparison of the myocardial blood flow response to regadenoson and dipyridamole: A quantitative analysis in patients referred for clinical 82Rb myocardial perfusion PET. Eur J Nucl Med Mol Imaging. 2011;38:1908-16.
- [Google Scholar]
- Comparison and effectiveness of regadenoson versus dipyridamole on stress electrocardiographic changes during positron emission tomography evaluation of patients with hypertrophic cardiomyopathy. Am J Cardiol. 2012;110:1033-9.
- [Google Scholar]
- Regadenoson versus dipyridamole hyperemia for cardiac PET imaging. JACC Cardiovasc Imaging. 2015;8:438-47.
- [Google Scholar]
- Regadenoson and adenosine are equivalent vasodilators and are superior than dipyridamole- a study of first pass quantitative perfusion cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2013;15:85.
- [Google Scholar]
- Initial clinical experience with regadenoson, a novel selective A2A agonist for pharmacologic stress single-photon emission computed tomography myocardial perfusion imaging. J Am Coll Cardiol. 2005;46:2069-75.
- [Google Scholar]
- Performance of cardiac cadmium-zinc-telluride gamma camera imaging in coronary artery disease: A review from the cardiovascular committee of the European Association of Nuclear Medicine (EANM) Eur J Nucl Med Mol Imaging. 2016;43:2423-32.
- [Google Scholar]
- An automatic approach to the analysis, quantitation and review of perfusion and function from myocardial perfusion SPECT images. Int J Card Imaging. 1997;13:337-46.
- [Google Scholar]
- Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the cardiac imaging committee of the council on clinical cardiology of the American Heart Association. Circulation. 2002;105:539-42.
- [Google Scholar]
- Myocardial perfusion and function: Single photon emission computed tomography. J Nucl Cardiol. 2007;14:e39-60.
- [Google Scholar]
- Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: Results from the clinical outcomes utilizing revascularization and aggressive drug evaluation (COURAGE) trial nuclear substudy. Circulation. 2008;117:1283-91.
- [Google Scholar]
- Stress myocardial perfusion imaging for assessing prognosis: An update. JACC Cardiovasc Imaging. 2011;4:1305-19.
- [Google Scholar]
- Comparison of risk stratification with pharmacologic and exercise stress myocardial perfusion imaging: A meta-analysis. J Nucl Cardiol. 2004;11:551-61.
- [Google Scholar]






