Translate this page into:
Cardiac Tamponade as Initial Presentation of Hodgkin Lymphoma
Address for correspondence: Dr. Adrija Hajra, 38/A/2, SB Ghosh Lane, Serampore, Hooghly - 712 202, West Bengal, India. E-mail: adrija847@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Cardiac involvement in malignant lymphoma is one of the least investigated subjects. Pericardial effusion is rarely symptomatic in patients of Hodgkin lymphoma (HL). Few case reports are available in the literature. There are case reports of diagnosed HL patients presenting with pericardial effusion. HL patients who present with recurrent episodes of pericardial effusion have also been reported. Pericardial effusion has also been reported in cases of non HL. However, pericardial effusion leading to cardiac tamponade as an initial presentation of HL is extremely rare. Very few such cases are there in the literature. Here, we present a case of a 26-year-old male patient who presented with cardiac tamponade and in due course was found to be a case of classical type of HL. This case is interesting because of its presentation.
Keywords
Cardiac tamponade
Hodgkin lymphoma
initial presentation
pericardial effusion

INTRODUCTION
Pericardial effusion is seen in approximately 5% of patients with Hodgkin lymphoma (HL).[1] It is usually asymptomatic. We have encountered patients with pleural effusion which is relatively common. There are case reports of previously diagnosed HL patients who later developed pericardial effusion.[1] We have also found case reports of non HL with cardiac tamponade as initial presentation.[2] However, cardiac tamponade as a presenting feature of HL has rarely been reported in the literature.[3] Here, we present a case of symptomatic pericardial effusion leading to cardiac tamponade as an initial presentation of HL.
CASE REPORT
A 26-year-old male patient presented to our outpatient department with a complaint of shortness of breath after doing normal daily activities that had persisted for 15 days. He also had fever for the past 7–8 days along with anorexia, night sweat, and weakness. He did not complain of weight loss during this period. There was no documentation of his weight for the last 1 year. He was examined thoroughly and significant findings were narrow pulse pressure of 14 mm of Hg (systolic blood pressure was 100 mm of Hg and diastolic blood pressure was 86 mm of Hg), elevated jugular venous pressure of 10 cm of H2O (≤8 cm of H2O), muffled heart sounds, and a single firm, round, mobile lymph node in the right anterior triangle of the neck. Available investigations showed hemoglobin was 11 g% (normal range: 13.3–16.2 g/dl), white blood cell (WBC) count 7800/cu mm (normal range: 3540–9060/cu mm) with 80% neutrophils and platelet count of 47,000/cu mm (normal range: 165,000-4.15/cu mm), and erythrocyte sedimentation rate (ESR) of 60 mm/h (normal range: 0–15mm/h). To evaluate the cause of diminished heart sound, echocardiography was performed immediately. It was revealed to be a case of cardiac tamponade, and immediate drainage of pericardial fluid was done. Approximately, 800 ml of fluid was drained at that setting. It was straw-colored opalescent fluid with thin coagulum. Routine and microscopic examination of pericardial fluid showed nucleated cells - 800/cu mm (mononuclear cells - 90% and neutrophils - 10%) and red blood cell were 700/cu mm. Gram-stain and acid fast bacilli stain showed no organism. Biochemical findings were pericardial glucose - 105 mg% (serum glucose was 103 mg% which was normal, pericardial level is roughly equal to this), protein - 5.4 g% (serum protein was 7 g% which was normal, pericardial level normally is 0.6 times of this.), albumin - 2.9 g%, adenosine deaminase - 5.8 U/L (normal range: 0–24 U/L), lactate dehydrogenase (LDH) – 231 U (serum LDH was 115 U which was normal; LDH level is normally 2.4 times of this value). In the meantime, chest X-ray of the patient revealed mediastinal widening [Figure 1]. Cervical lymph node excisional biopsy demonstrated histological finding of HL with lacunar cells (variant of Reed–Sternberg cells) which were positive for CD15 and CD30 [Figure 2]. This suggested the presence of a nodular sclerosing variant. Computed tomography (CT) scan chest showed anterior mediastinal mass suggestive of mediastinal lymphadenopathy and presence of pericardial effusion [Figures 3 and 4]. CT scan abdomen and pelvis was done for staging of disease though no lymph node was detected below the diaphragm. After initial evaluation and staging, it was revealed that patient had Stage IIB HL with an unfavorable prognosis. Combined chemotherapy and radiotherapy were planned for treatment. Chemotherapy with doxorubicin, vinblastine, bleomycin, and dacarbazine had been started and one cycle has been completed so far.
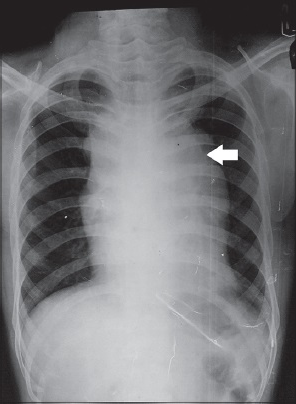
- 26-year-old male patient presented with fever, night sweat and shortness of breath, subsequently diagnosed to have pericardial effusion leading to cardiac tamponade. Further studies led to the diagnosis of Hodgkin lymphoma. Chest X-ray posteroanterior view shows mediastinal widening (arrow) suggestive of mediastinal lymphadenopathy.
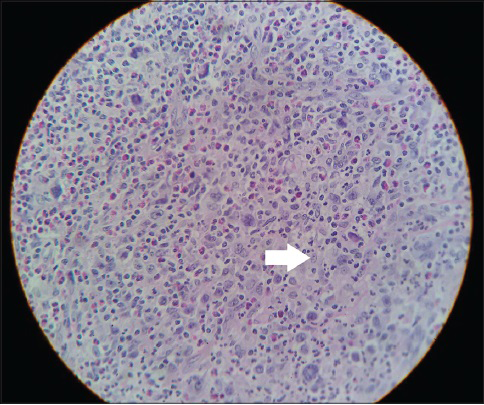
- 26-six-year-old male patient presented with fever, night sweat and shortness of breath, subsequently diagnosed to have pericardial effusion leading to cardiac tamponade. Further studies led to the diagnosis of Hodgkin lymphoma. Cervical lymph node biopsy stained with hematoxylin and eosin magnification ×10 shows lacunar variety of Reed Sternberg cell (arrow) suggestive of nodular sclerosing Hodgkin lymphoma.
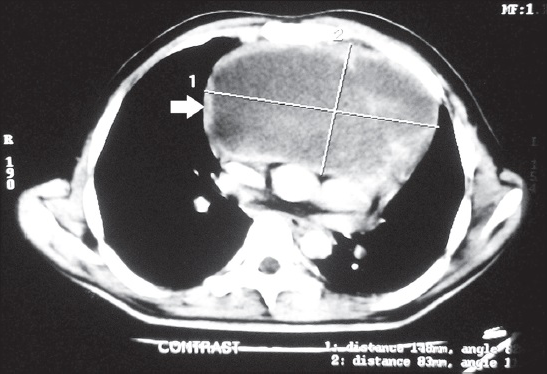
- 26-six-year-old male patient presented with fever, night sweat and shortness of breath, subsequently diagnosed to have pericardial effusion leading to cardiac tamponade. Further studies led to the diagnosis of Hodgkin lymphoma. Computed tomography scan thorax of the same patient shows anterior mediastinal lymphadenopathy (arrow) greatest dimension of the mass is 14.8 cm.
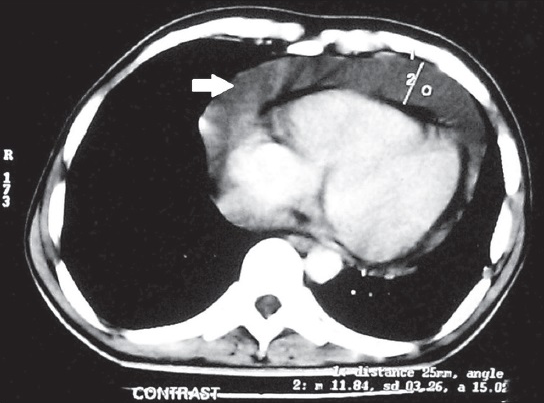
- 26-year-old male patient presented with fever, night sweat and shortness of breath, subsequently diagnosed to have pericardial effusion leading to cardiac tamponade. Further studies led to the diagnosis of Hodgkin lymphoma. Computed tomography scan thorax shows pericardial effusion (arrow).
DISCUSSION
HL is a relatively common disease with an incidence of 3 cases in 100,000 in the Western world.[1] Cardiac metastasis is found in 20–25% of lymphoma patients.[4] Studies by Roberts et al., and Cairns et al., report that 9% of all cardiac tumors are related to lymphoma.[4] However, the clinical course and outcome of pericardial involvement in HL are not very well known. Pericardium may get involved due to pericardial seeding from metastatic disease, invasion from primary cardiac tumors, benign idiopathic causes, infection, or drug/radiation-induced pericarditis.[1] In addition, patients who are immunocompromised due to treatment of an underlying malignancy can develop autoimmune pericardial effusion. There are some explanations regarding pericardial effusion in lymphoma. It may be due to lymphatic and hematogenous spread. Effusion may be caused by blockage of lymphatic and venous drainage of pericardial fluid. Effusion may also be caused without involvement of the pericardium. The lymphatic channels from visceral pericardium have ultimate drainage at the aortic root. This drainage site can be blocked either by malignant deposits or via compression due to enlarged lymph nodes.[1] In most of the cases, patients with cardiac involvements are clinically silent. In a retrospective study consisting of 273 patients, Bashir et al., recorded only two patients with symptoms of pericardial effusion.[5] Malignant lymphoma can originate in or spread to the mediastinum. Mediastinal lymphadenopathy due to lymphoma may present early due to rapid growth of the tumor and compression caused by it. The clinical manifestations may be cough, dysphagia, and hoarseness of voice.[6] However, pericardial effusion as an initial presentation is very rare. This patient had a feature of early tamponade though his presentation was not drastic but rather subtle. The rate of fluid accumulation within pericardial cavity determines the intra pericardial pressure and pattern of presentation.[2] In our patient, pericardial fluid was drained immediately to prevent future complication and sent for investigation. Tissue diagnosis helped us diagnose the case. This case is unique due to its presentation. The patient was admitted for evaluation of shortness of breath, but he was detected to have HL. Our patient was diagnosed to have Stage IIB disease with some unfavorable prognostic factors (large mediastinal adenopathy; ESR ≥ 30 mm/h with B symptoms). Regarding staging, our pateint had a positive cervical lymph node and mediastinal lymphadenopathy. CT scan thorax was done after excisional biopsy of cervical node and it revealed mediastinal lymphadenopathy. CT scan abdomen showed there was no lymph node below the diaphragm. He had fever and night sweat indicative of B symptoms. Hence, he was diagnosed with Stage IIB disease. He also had extranodal involvement in terms of pericardial effusion. International prognostic score (IPS) is a predictor of treatment outcome for HL patients. There are seven prognostic points: Serum albumin level <4 g/L, hemoglobin <10.5 g/dl, male gender, age more than 45 years, Stage IV disease, WBC count ≥15,000/μL, absolute lymphocyte count <600/μL, and/or <8% of the total WBC count. Our patient being a male had one prognostic factor. In a study with 5141 patients with HL treated with combination chemotherapy with or without radiotherapy, event free survival rates at 5 years was found to be 77% with one factor mentioned in IPS. According to European Organization for the Research and Treatment of Cancer (EORTC) trials and German Hodgkin's Study Group, trials have grouped the variants as having favorable or unfavorable prognosis. Our patient fulfilled the criteria (current Lugano classification) of having single nodal mass of more than 10 cm [14.8 cm as depicted in Figure 3], B symptoms and raised ESR.[7] Studies have shown different chemotherapeutic regimens in unfavorable prognosis Stage I-II disease generally have no important differences in overall survival. Doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) is usually considered the treatment of choice. It is given every 14 days in 28 days cycles; two administrations are considered one cycle. Patient is given radiotherapy between fourth and sixth cycles of ABVD depending upon response. The randomized EORTC H8U trial using four cycles of chemotherapy provides the most complete evidence to date that four cycles of chemotherapy is sufficient when combined with radiotherapy. According to the International Lymphoma Radiation Oncology Group, involved site radiation therapy is preferred over larger radiation fields. In general, four cycles of ABVD should be followed by 30 Gy involved site radiation in patients with unfavorable prognosis nonbulky early-stage HL. Bulky disease is treated with 30–36 Gy radiation dose.[8] Our patient has received one cycle of chemotherapy and is under monitoring to detect response and adverse effects. Our patient had nodular sclerosing type HL. Most common types of lymphoma presenting with mediastinal mass are nodular sclerosing type.[9] In a study conducted by Bashir et al., it was seen that all patients with pericardial involvement have nodular sclerosing type of disease.[5] In other case reports also, we have found that patients had nodular sclerosing variety of HL.[3410] Whether nodular sclerosing type of histology has a relationship with development of pericardial effusion needs more evaluation.
CONCLUSION
HL is one of the curable malignancies. It can present in a variety of ways with nonspecific symptoms of fever, weight loss or night sweat, asymptomatic lymphadenopathy, mediastinal mass producing local symptoms, or systemic symptoms. As in our case, they may also present with symptomatic pericardial effusion in rare occasions. Early intervention not only helped our patient symptomatically, but it also allowed us to do further investigations. Commonly, in India, infectious diseases such as tuberculosis are sought in such backgrounds, but biopsy proved our case to be HL. As patients of HL have a good post therapy survival, it is important to detect treatable manifestations early. Large mediastinal mass as present in our patient; though rare, can present with superior vena caval obstruction syndrome and require emergency attention. Apart from these, a patient of HL treated with chemotherapy has increased chance of infections. Proper monitoring and, if needed, prophylactic antibiotic therapy may be given. Development of second malignancies (lung cancer, acute leukemia, non HL) and cardiovascular complications other than pericardial involvement may occur in these patients. Symptomatic pericardial effusion as first presentation of HL makes this case interesting. These patients can develop pericardial effusion in later course due to the disease itself or as a complication of therapy particularly radiation therapy. As the rate of fluid accumulation within pericardial cavity determines the acuteness of presentation of cardiac tamponade, it may be possible that future presentation of pericardial effusion leading to tamponade will be more aggressive. Early detection and timely intervention is necessary to combat such situations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2015/5/1/67/172971
REFERENCES
- Symptomatic pericardial effusion in Hodgkin's lymphoma: A rare occurrence. Case report and review of the literature. Tumori. 2012;98:50e-2e.
- [Google Scholar]
- Non-Hodgkin's lymphoma presenting as malignant pericardial effusion and cardiac tamponade. Hum Pathol. 1985;16:315-7.
- [Google Scholar]
- A case of Hodgkin's lymphoma which caused pericardial tamponade in a young female patient. Thorac Cardiovas Surg Derg. 2012;20:659-61.
- [Google Scholar]
- Hodgkin's lymphoma presenting with heart failure: A case report. J Med Case Rep. 2010;4:14.
- [Google Scholar]
- Pericardial involvement at diagnosis in pediatric Hodgkin lymphoma patients. Pediatr Blood Cancer. 2007;49:666-71.
- [Google Scholar]
- Cardiac tamponade; a rare presentation of mediastinal lymphoma. J Case Rep Pract. 2014;2:113-5.
- [Google Scholar]
- Staging and prognosis of Hodgkin lymphoma. 2015. UpToDate. Available from: http://www.uptodate.com/contents/staging-and-prognosis-of-hodgkin-lymphoma
- [Google Scholar]
- Treatment of unfavorable prognosis early (stage I- II) classical Hodgkin lymphoma. 2015. UpToDate. Available from: http://www.uptodate.com/contents/treatment-of-unfavorable-prognosis-early- stage-I-II-classical- hodgkin-lymphoma
- [Google Scholar]
- Evaluation of mediastinal masses. 2015. UpToDate. Available from: http://www.uptodate.com/contents/evaluation-of-mediastinal-masses
- [Google Scholar]






