Translate this page into:
Caliber-Persistent Labial Artery: A Report of a Rarely Recognized Lip Swelling
Address for correspondence: Dr. Malarkodi Thanthoni, No. 20085, Tower 20B Floor 7, Prestige Bella Vista, Iyyapanthangal, Chennai - 600 056, Tamil Nadu, India. E-mail: tmalarkodi@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Calibre-persistent labial artery (CPLA) is a commonly underdiagnosed vascular lesion of the lip. CPLA is an arterial branch that penetrates the submucosal tissue without loss of calibre. Clinical diagnosis is significant as misdiagnosis can lead to profuse haemorrhage following an excisional biopsy or surgical excision. Colour Doppler ultrasonography is a safe and non-invasive diagnostic tool to confirm the diagnosis. Here, we report a case of a 24-year-old man who complained of an asymptomatic pulsating non-progressive nodule on the left side of upper lip initially diagnosed as peripheral angiomatous lesion. Diagnosis was confirmed by high-resolution Colour Doppler Ultrasonography. The purpose of this case report is to highlight the clinical importance and diagnosis of a rarely reported soft tissue swelling of the lip to the attention of clinicians.
Keywords
Caliber-persistent artery
caliber-persistent labial artery
lip swelling
vascular lesion

INTRODUCTION
Caliber-persistent labial artery (CPLA) is an arterial division that infiltrates the submucosal tissue of the lip without arborizing or loss of caliber.[1] Gallard,[2] in 1884, was the first to describe about abnormally large arteries within the gastric submucosa of three patients that died of gastric hemorrhage. Initially, these vascular anomalies occurring in the stomach and jejunum were misdiagnosed as arterial malformation, cirsoid aneurysm, and dieulafoy’s disease.[3] Later, in 1973, Howell and Freeman[4] first described about this type of vascular anomaly in the oral cavity, and it was termed as “prominent inferior labial artery.” The current terminology CPLA was given by Mikó et al., in 1980.[5]
The incidence of CPLA is approximately 3%[4] with lower lip being the most common site.[6] Few cases have also been reported on the upper lip, palate, and buccal vestibule.[17] Most of these patients were between 40 and 80 years of age.
CPLA can present as an ulcer, soft-tissue papule, or as a linear pulsating nodule with bluish or normal mucosal color. It is usually asymptomatic and diagnosed during the routine clinical examination. Occasionally, the patient can notice an increased pulse volume at the site of the lesion that could be visible or palpable. Patients with ulcers have reported with hemorrhagic episodes too.[78] We report a case of caliber-persistent artery (CPA) of the upper lip.
CASE REPORT
A 24-year-old male patient had been aware of a soft pulsating swelling on the left side of the upper lip for about 15 days. The nodule remained of the same size, and there was not any history of trauma to the lip, bleeding or interference in speech, and mastication. His medical history was unremarkable, and he does not smoke.
The clinical examination revealed a slightly raised nodule measuring 3 mm × 3 mm on the left side of the upper labial mucosa extending from the vermilion border. It was sessile, the surface and color appeared normal, and the pulsation was seen. The lesion was soft, nontender, and pulsatile on palpation. The remaining oral mucosa was normal. A provisional diagnosis of peripheral angiomatous lesion was given [Figure 1].

- A 24-year-old male with soft pulsating nodule on the left vermilion of the upper lip (arrow).
Color Doppler ultrasonographic examination was performed from the mucosal side of the oral cavity. The examination was carried out using a compact linear transducer with a frequency range of 7–15 MHz. An arterial vessel with a tortuous course was located on the left side of the upper labial mucosa [Figure 2]. The distance between the artery and the surface mucosa was 0.9mm. The diameter of the artery was 1mm near the periphery [Figure 3]. The peak systolic velocity was 58.06cm/s, and end-diastolic velocity was 11.87cm/s whereas the pulsatility and resistivity indices were 1.95 and 0.80, respectively. The spectral curve analysis showed moderate flow velocity, high resistance, and a dicrotic notch with forward flow in both systole and diastole [Figure 4]. There was no evidence of arteriovenous shunts or abnormal vascular communication or calcific deposits. The structures surrounding the vessel appeared normal.
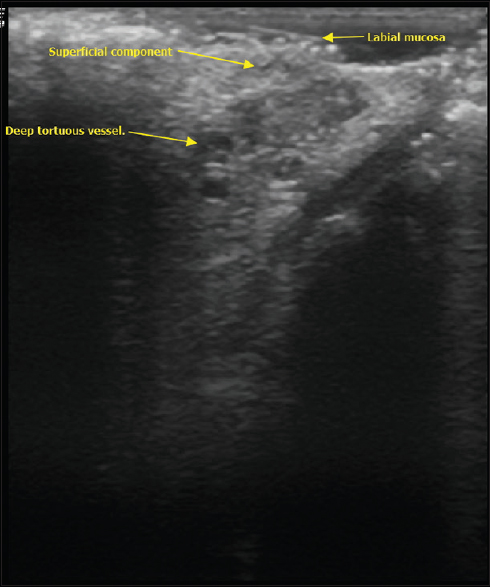
- Longitudinal view sonographic image shows tortuous course of superior-labial artery branch from deeper layers to superficial mucosal component.
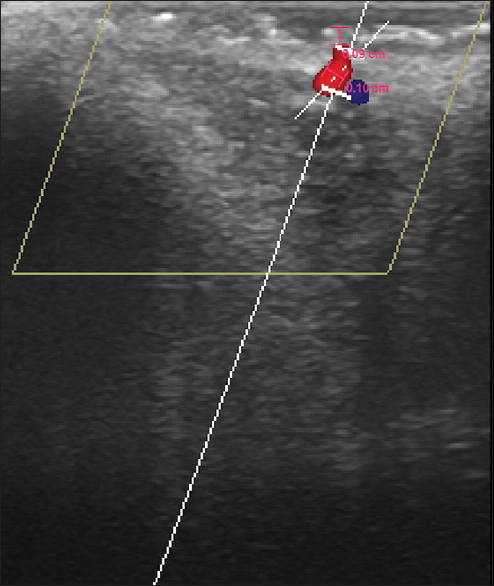
- Ultrasound image shows the arterial location at 0.9 mm below the mucosal surface with a diameter of 1 mm transversely.
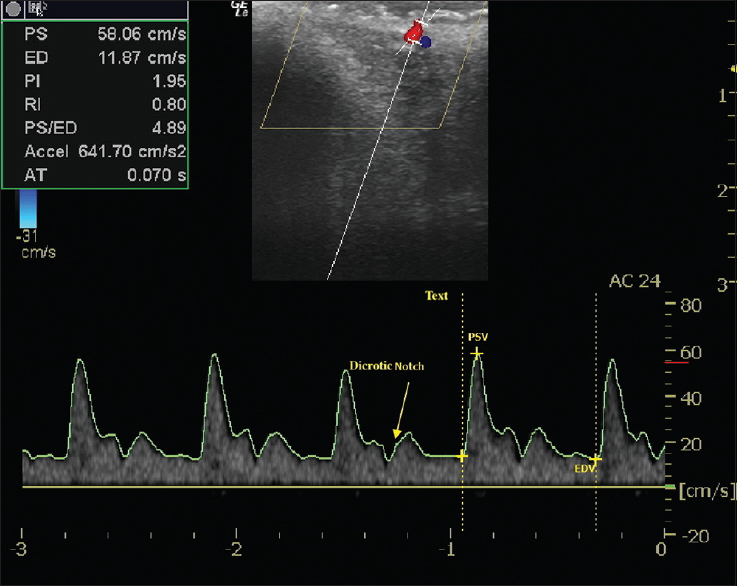
- Spectral measurements reveal high resistance and flow velocity with a dicrotic notch in the superior-labial artery branch, left side. PSV: Peak systolic velocity, EDV: End-diastolic velocity).
As the patient was asymptomatic with no clinical signs of ulceration or ischemic changes, the immediate surgical intervention was not recommended; however, the patient was well informed about the risk of bleeding even with minor trauma.
DISCUSSION
CPLA is a vascular lesion in which the primary arterial division will neither lose its caliber nor arborize after penetrating the submucosal tissue.[1]
In 1980, following a series of three cases, Mikó et al. reported about the extra gastrointestinal presentation of this lesion in the lower lip and introduced the current terminology “CPA of the lower lip.” All three cases which presented as chronic ulceration involving the lower lip were clinically misdiagnosed with malignant ulcers and were treated with wedge resection. However, microscopic examination showed ulceration without any dysplastic features. It also showed an artery with a large diameter, penetrating the orbicularis oris muscle without subdivision, or decrease in diameter representing a branch of inferior-labial artery.[5]
Marshall and Leppard,[9] in 1985, reported a case of CPA in a 72-year-old male patient who presented with a long-standing ulceration of the lower lip. A wedge lip excision was done as it mimicked squamous cell carcinoma.
Mikó et al.,[5] and Marshall and Leppard[9] emphasized that CPLA should be considered when chronic inflammation and ulceration are evaluated. Jaspers, in 1992,[1] reported two cases of CPA with different presentations. The first case reported with chronic ulceration of the hard palate with hemorrhagic episode. Following surgical removal of the ulcer, the patient has experienced profuse hemorrhage from the surgical site. The second case was an asymptomatic whitish – tan, nodular lesion involving the lower lip that was clinically misdiagnosed with mucocele. There was “vigorous arterial hemorrhage” during the surgical excision. Histopathological findings of both the lesions were consistent with CPLA. Hence, Jaspers suggested that CPLA can be included in the differential diagnosis of the soft-tissue nodule as it can also present without ulceration or inflammation.[1]
The etiology of CPLA remains unclear. Different theories have been hypothesized to explain the etiology of this lesion. First, Mikó et al.,[5] suggested that senile atrophy of the soft tissues caused senile ectasias of the blood vessels. Factors, such as trauma, pressure from pipe stem, sun exposure, and continuous pressure exerted by the pulsating artery over the epithelium, were linked as probable reasons for chronic ulcers associated with CPLA. Although the theory of aging was supported by Mikó et al.,[5] based on his case reports in elderly patients, it is unlikely that this is the reason for the occurrence, as CPLAs were reported in young adults too.[810] Our case was also diagnosed at the age of 24 years.
Kocyigit et al.[8] believed that CPLA'S are congenital malformation of the blood vessels that are left unrecognized for a long time until it becomes prominent. The theory of the sun exposure as a reason for mucosal erosion or degeneration ratifies for lesions occurring on the lip. However, the same could not be validated for lesions that occurred in buccal vestibule and palate.[17]
Clinically, CPLA can appear either as a soft elevated nonulcerated pulsatile solitary lesion which could be linear or papular, located close to the mucosa having a unilateral presentation or as chronic ulcers.[14568] Although pulsation serves as a key feature in the clinical diagnosis of CPLA, noninvasive test, such as color Doppler ultrasonography, can be used to confirm the diagnosis.[89]
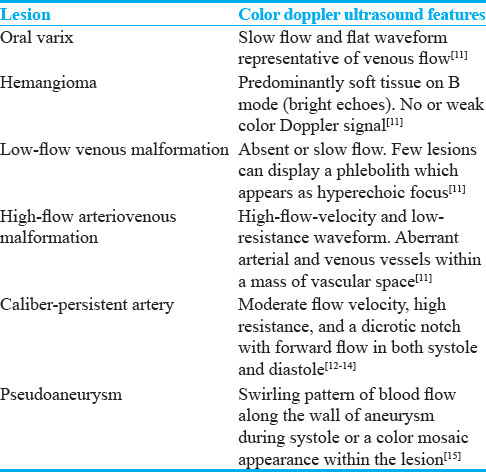
Vascular lesions such as varicose veins, hemangioma, pseudoaneurysm, and vascular malformation[11] [Table 1] along with nonvascular lesions, such as mucocele, irritational fibroma, and sclerosing sialadenitis, can be considered in the differential diagnosis of CPLA.[18]
Misdiagnosis can lead to vigorous arterial hemorrhage when attempted with an excisional biopsy.[14569] The location of these lesion makes it susceptible to trauma, and the ensuing hemorrhage will require a surgical procedure to achieve hemostasis.[1]
High-resolution B-mode/Grayscale imaging with a linear high-frequency transducer shows a good near-field resolution to differentiate fine anatomic details in superficial structures. Color Doppler adds an extra layer of information over the B-mode, i.e., directional information about moving/flowing content. Spectral Doppler adds yet another layer of added information pertaining to the velocity of the moving content.
CPLA can be diagnosed using reliable, real-time imaging method such as color Doppler ultrasonography that has high resolution, frequency, and provides both morphological and vascular information. This noninvasive diagnostic method has several benefits over angiography as it permits to assess the location and distance of the vessel from the mucosal surface, its diameter and the direction of blood flow through direct visualization. In addition, color Doppler spectral curve analysis determines the blood-flow velocity (cm/s) and the arterial or the venous nature, thereby reducing the risk of complications that might occur following a surgical procedure. Compact linear transducers have the shape of a hockey stick and enable better examination and access of intraoral structures. This small-sized probe permits the visualization of the course and anatomy of the blood vessel both from extraoral and intraoral mucosal surface, thereby allowing a complete three-dimensional evaluation.[11121314] In our case, B-mode imaging shows a prominent well-defined single luminal structure seen extending from the deep plane to the cutaneous plane. The intimal and medial layers were well differentiated with the muscular layer being well demonstrable in arteries as compared to veins. By this deduction, we can see that the visualized vessel in our case appears to be a CPA in the submucosal region. Sonographic findings of the present case were similar to that of the previously reported CPLA’s.
Commonality of CPA occurring in the stomach and lip ends with profuse hemorrhage. Death following profuse hemorrhage has been reported in CPA’s occurring in the gastrointestinal tract,[23] however, no reported fatality following lip hemorrhage from CPLA.
Patients young age, no history of trauma, or use of tobacco could be included as a plausible cause for lack of ulceration or bleeding[8] in the present case. The treatment of choice varies with the clinical presentation of the lesion. Conservative management and reassurance can be considered for cases which are asymptomatic and surgical management for lesions that are symptomatic and/or located at susceptible sites to trauma and/or unesthetic on patients’ demand. Doppler ultrasonography should be used to confirm the diagnosis to avoid the brisk arterial hemorrhage associated with excisional biopsy or surgery and as a follow-up noninvasive tool.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/41/241712
REFERENCES
- Oral caliber-persistent artery.Unusual presentations of unusual lesions. Oral Surg Oral Med Oral Pathol. 1992;74:631-3.
- [Google Scholar]
- Miliary aneurysm of the stomach giving cause to fatal hematemesis. Bull Mem Soc Med hop Paris. 1884;1:84-91.
- [Google Scholar]
- A 74-year-old man with fatal gastrointestinal bleeding.Ruptured dieulafoy lesion or caliber-persistent artery. Arch Pathol Lab Med. 2006;130:223-4.
- [Google Scholar]
- Simulated cancer of the lower lip attributed to a “caliber persistent” artery. J Oral Pathol. 1980;9:137-44.
- [Google Scholar]
- Caliber-persistent labial artery. A common vascular anomaly. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:308-12.
- [Google Scholar]
- Calibre persistent labial artery: Clinical features and noninvasive radiological diagnosis. Clin Exp Dermatol. 2006;31:528-30.
- [Google Scholar]
- Ulceration of the lip associated with a ‘calibre-persistent artery’. Br J Dermatol. 1985;113:757-60.
- [Google Scholar]
- Clinical diagnosis of caliber-persistent labial artery of the lower lip. Oral Surg Oral Med Oral Pathol. 1993;76:480-3.
- [Google Scholar]
- Color-Doppler ultrasound in the diagnosis of oral vascular anomalies. N Am J Med Sci. 2014;6:1-5.
- [Google Scholar]
- Ultrasonography: A noninvasive tool to diagnose a caliber-persistent labial artery, an enlarged artery of the lip. J Ultrasound Med. 2005;24:1295-301.
- [Google Scholar]
- High-resolution color Doppler ultrasound of a caliber-persistent artery of the lip, a simulator variant of dermatologic disease: Case report and sonographic findings. Int J Dermatol. 2009;48:830-3.
- [Google Scholar]
- Early diagnosis of a calibre persistent labial artery in a child: Usefulness of ultrasonography. Australas J Dermatol. 2012;53:e18-9.
- [Google Scholar]
- “To-and-fro” waveform in the diagnosis of arterial pseudoaneurysms. World J Radiol. 2015;7:89-99.
- [Google Scholar]






