Translate this page into:
Bronchial Artery Arising from the Left Vertebral Artery: Case Report and Review of the Literature
Address for correspondence: Dr. Timothy J. Amrhein, Department of Radiology, Duke University Medical Center, Box 3808 DUMC, Durham, NC 27710. E-mail: timothy.amrhein@duke.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Knowledge of bronchial artery anatomy, including the possible locations of anomalous origin, is essential for complete catheter directed embolization for massive hemoptysis. Undetected anomalous bronchial arteries can be a source of failed bronchial artery embolization. We report a case of a common trunk bronchial artery arising from the left vertebral artery and review standard and variant bronchial artery anatomy.
Keywords
Anomalous
aberrant
bronchial artery
CT angiography
embolization
INTRODUCTION

The bronchial arterial circulation is the source of bleeding in nearly 90% of cases of massive hemoptysis.[1] Bronchial artery embolization (BAE) has become an established procedure for the treatment of massive hemoptysis with proven efficacy and safety.[1] A thorough knowledge of bronchial artery anatomy, including the possible locations of anomalous origin, is an integral component of a successful procedure. The anatomy of the bronchial arteries has been previously reported in considerable detail, outlining variations in origin, course, and branching pattern.[2] We report a case of a common trunk bronchial artery arising from the left vertebral artery and review standard and variant bronchial artery anatomy relevant to complete evaluation of the bronchial arterial supply.
CASE REPORT
An 89-year-old female with a past medical history of hypertension and chronic obstructive pulmonary disease presented to the emergency department with new onset of dizziness and gait instability that had been progressive over the prior 7 months. She was admitted to the Neurology service, and during her evaluation for these complaints, she developed symptoms of shortness of breath, tachycardia, and chest fullness. Computed tomographic pulmonary angiography (CTA) was performed for evaluation of pulmonary embolism using a 16-detector scanner (Lightspeed 16, GE Medical Systems, Milwaukee, WI). Images through the thorax were acquired at 1.25 mm collimation (120 kVp, 441 mA, pitch 1.375:1, rotation time 0.8s) after bolus tracking at the main pulmonary artery during the administration of 100 mL of iopamidol nonionic contrast media (Isovue 370, Bracco Diagnostics Inc.) at 5 mL/s. While pulmonary embolism was not present, incidental finding was made of an anomalous bronchial artery arising from the proximal aspect of a left vertebral artery originating from the aortic arch between the left common carotid and left subclavian arteries [Figures 1a–c]. This single bronchial artery arose from the right posterior aspect of the left vertebral artery approximately 1.5 cm distal to the aortic arch. The bronchial artery coursed along the left aspect of the trachea prior to bifurcating into right and left bronchial arteries approximately 1 cm above the carina. Single bronchial arteries then coursed along the bilateral mainstem bronchi until subdividing into smaller tributary branches distally. No additional bronchial arteries were identified despite meticulous review of the source axial, reconstructed multiplanar, and 3D volume rendered images [Figure 2a–c].

- Contrast-enhanced axial CT images of the chest. (a) A common trunk anomalous bronchial artery arises from the left vertebral artery. (b) This bronchial artery courses inferiorly along the trachea. (c) Bifurcation of the bronchial artery into left and right branches, which supply the respective lungs.
![(a) Curved multiplanar reconstruction demonstrates the course of the bronchial artery within the mediastinum. (b) 3D volume rendered image demonstrates origin of the bronchial artery from the left vertebral artery (The right brachiocephalic artery has been excluded). (c) Note the close approximation of the bronchial artery with the adjacent tracheobronchial tree. [LSCA: Left subclavian artery; LCCA: Left common carotid artery; L Vertebral Art: left vertebral artery; RBCA: Right brachiocephalic artery].](/content/12/2011/1/1/img/JCIS-1-62-g003.png)
- (a) Curved multiplanar reconstruction demonstrates the course of the bronchial artery within the mediastinum. (b) 3D volume rendered image demonstrates origin of the bronchial artery from the left vertebral artery (The right brachiocephalic artery has been excluded). (c) Note the close approximation of the bronchial artery with the adjacent tracheobronchial tree. [LSCA: Left subclavian artery; LCCA: Left common carotid artery; L Vertebral Art: left vertebral artery; RBCA: Right brachiocephalic artery].
Secondary to this finding the possibility of steal phenomena was explored via transcranial Doppler evaluation, which was negative. An etiology for the patient's neurological symptoms was not identified and the patient was discharged and advised outpatient physical and occupational therapy.
DISCUSSION
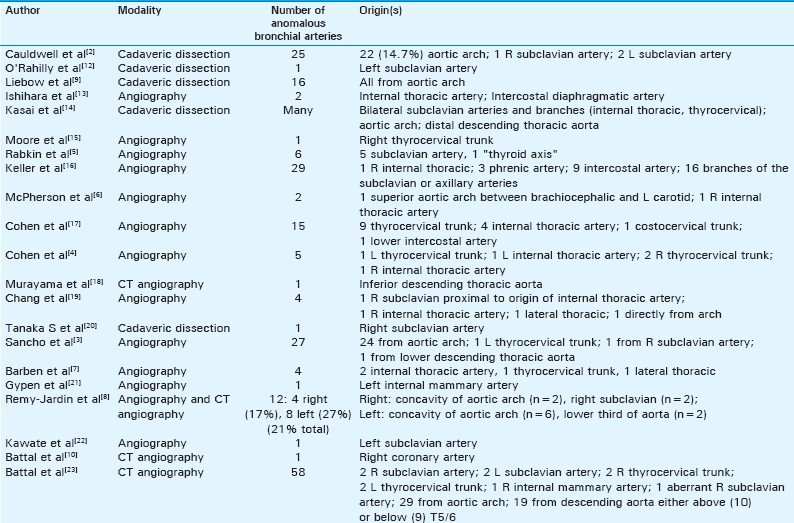
Numerous earlier investigations have evaluated the anatomy of the bronchial arteries describing variation in their origin, branching patterns and course. The bronchial arteries most commonly arise from the descending thoracic aorta between the lower margin of the T4 vertebral body and the upper margin of the T6 vertebral body (70 – 83.3%).[3] Bronchial arteries with an origin outside of this region are considered anomalous. The reported incidence of anomalous bronchial arteries varies widely, ranging from 8.3 to 35%.[1] In 1948, Caudwell et al reported their anatomical findings after dissection of 150 human cadavers.[2] This landmark study revealed 25 anomalous bronchial arteries (16.7%), 22 arising directly from the aortic arch (14.7%), 1 from the right subclavian artery, and 2 from the left subclavian artery. A review of the literature demonstrates general agreement with these initial findings, with an anomalous origin from the aortic arch being most common and an origin from the subclavian arteries second most common. Since Caudwell et al's initial extensive study, anomalous bronchial arteries have also been reported to arise from the thyrocervical trunk, internal mammary artery, costocervical trunk, lateral thoracic artery, and the inferior aspect of the descending thoracic aorta.[3–9] Additionally, Battal et al recently described the origin of an anomalous bronchial artery from the right coronary artery via multidetector computed tomography (MDCT) [Table 1].[10]
MDCT angiography is a proven method for the evaluation of the bronchial arteries. In their retrospective study comparing conventional angiography with thin-section MDCT angiography, Remy-Jardin et al found concordant identification of the number and origin of bronchial arteries in 86% of cases.[8] Use of MDCT angiography prior to attempted BAE may provide assistance in directing selective catheterization, particularly in the setting of an anomalous origin of the bronchial arteries, possibly reducing procedure time. Further, MDCT has the added benefit of providing an opportunity to identify non-bronchial artery bleeding sources such as non-bronchial systemic arteries, bronchiectasis, bronchogenic carcinomas, and aspergillomas.[1] The normal adult bronchial arteries measure less than 1.5 mm in diameter at their origin and 0.5 mm at their point of entry into a bronchopulmonary segment.[11] Abnormal or hypertrophic bronchial arteries measure greater than 2 mm in diameter on MDCT.
We believe that this case represented a true bronchial artery, rather than a non-bronchial systemic collateral artery for several reasons. First, the 1-mm vessel diameter is well within the normal range for a native bronchial artery. Second, there was no evidence of pleural thickening, significant pulmonary disease, or associated systemic collateralization to suggest that this vessel had arisen secondary to an underlying pathologic process. Third, the patient had no prior history of bronchial artery embolization that would have lead to the recruitment of abnormal collateral vessels. Fourth, no additional candidate bronchial arteries were identified. Finally, and most importantly, this vessel coursed along the tracheobronchial tree, which is the main distinguishing characteristic of a bronchial artery [Figure 2c].
A complete knowledge of bronchial artery anatomy, including the locations of their common aberrant origin, is a prerequisite for successful complete angiographic assessment of the bronchial artery distribution as well as for successful embolization procedures. Failure to identify a causative bronchial artery arising from the descending aorta should prompt a search for an aberrant origin, including an evaluation of the aortic arch and of the bilateral subclavian arteries and their branch vessels. In light of the case presented here, consideration of an origin from the vertebral artery should be entertained in cases of persistent failed identification.[23]
ACKNOWLEDGMENTS
The authors would like to thank Laura Pierce, RT for her gracious help in generating the images for this report.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/62/91135
REFERENCES
- Bronchial and nonbronchial systemic artery embolization for life-threatening hemoptysis: A comprehensive review. Radiographics. 2002;22:1395-409.
- [Google Scholar]
- The bronchial arteries; an anatomic study of 150 human cadavers. Surg Gynecol Obstet. 1948;86:395-412.
- [Google Scholar]
- Embolization of bronchial arteries of anomalous origin. Cardiovasc Intervent Radiol. 1998;21:300-4.
- [Google Scholar]
- Left thyrocervical trunk bronchial artery supplying right lung: Source of recurrent hemoptysis in cystic fibrosis. AJR Am J Roentgenol. 1992;158:1131-3.
- [Google Scholar]
- Transcatheter embolization in the management of pulmonary hemorrhage. Radiology. 1987;163:361-5.
- [Google Scholar]
- Anomalous origin of bronchial arteries: Potential pitfall of embolotherapy for hemoptysis. J Vasc Intervent Radiol. 1990;1:86-8.
- [Google Scholar]
- Bronchial artery embolization for hemoptysis in young patients with cystic fibrosis. Radiology. 2002;224:124-30.
- [Google Scholar]
- Bronchial and nonbronchial systemic arteries at multi-detector row CT angiography: Comparison with conventional angiography. Radiology. 2004;233:741-9.
- [Google Scholar]
- Patterns of origin and distribution of the major bronchial arteries in man. Am J Anat. 1965;117:19-32.
- [Google Scholar]
- Aberrant right bronchial artery originating from right coronary artery - MDCT angiography findings. Br J Radiol. 2010;83:e101-4.
- [Google Scholar]
- The bronchial circulation.Small, but a vital attribute of the lung. Am Rev Respir Dis. 1987;135:463-81.
- [Google Scholar]
- Selective bronchial arteriography and hemoptysis in nonmalignant lung disease. Chest. 1974;66:633-8.
- [Google Scholar]
- Macroscopic anatomy of the bronchial arteries. Anatomischer Anzeiger. 1979;145:166-81.
- [Google Scholar]
- Massive hemoptysis: Control by embolization of the thyrocervical trunk. Radiology. 1986;161:173-4.
- [Google Scholar]
- Nonbronchial systemic collateral arteries: Significance in percutaneous embolotherapy for hemoptysis. Radiology. 1987;164:687-92.
- [Google Scholar]
- Bronchial artery embolization to control hemoptysis in cystic fibrosis. Radiology. 1990;175:401-5.
- [Google Scholar]
- Helical CT imaging of bronchial arteries with curved reformation technique in comparison with selective bronchial arteriography: Preliminary report. J Comput Assist Tomogr. 1996;20:749-55.
- [Google Scholar]
- Major hemoptysis in a child with cystic fibrosis from multiple aberrant bronchial arteries treated with tranexamic acid. Pediatr Pulmonol. 1996;22:416-20.
- [Google Scholar]
- Right superior bronchial artery arising from the right subclavian artery and accompanying nerve branches: An autopsy case. Kaibogaku zasshi J Anat. 1997;72:455-60.
- [Google Scholar]
- Severe hemoptysis 6 years after coronary artery bypass grafting. Ann Thorac Surg. 2003;75:999-1001.
- [Google Scholar]
- Rare multiple combined anomaly of the vertebral vessels and bronchial artery. Anat Sci Int. 2008;83:267-72.
- [Google Scholar]
- Normal anatomical features and variations of bronchial arteries: An analysis with 64-detector-row computed tomographic angiography. J Comput Assist Tomogr. 2011;35:253-9.
- [Google Scholar]






