Translate this page into:
F-18 Fluorodeoxy Glucose Positron Emission Tomography/Computed Tomography Findings in a Rare Case of Penile Leiomyosarcoma
Address for correspondence: Dr. Bhagwant Rai Mittal, Department of Nuclear Medicine and PET, PGIMER, Chandigarh-160 012, India. E-mail: brmittal@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Penile cancer is a rare entity accounting for only 0.4% all male malignancies. Penile leiomyosarcomas are even rarer with only around 35 cases reported in literature. We report a rare case of penile leiomyosarcoma illustrating F-18 Fluorodeoxy glucose (FDG) positron emission tomography/computed tomography (PET/CT) features and histopathology correlation.
Keywords
F-18 FDG
leiomyosarcoma
penile cancer
PET/CT
INTRODUCTION

Penile cancer is a relatively rare neoplasm of the urogenital tract. Penile leiomyosarcoma is still rarer with only about 35 cases reported in literature. Imaging findings, even with computed tomography (CT), of such tumors are rarely described in literature. F-18 fluorodeoxy glucose positron emission tomography/computed tomography (F-18 FDG PET/CT) is emerging as a useful modality in assessment of genito-urinary malignancies. F-18 FDG PET/CT findings in penile leimyosarcoma have not been reported in literature. We present here a case of penile leiomyosarcoma with emphasis on findings on F-18 FDG PET/CT with histopathology correlation.
CASE REPORT
A 47-year-old male presented with a palpable penile mass, with rapid growth over a period of 1 month. He was examined at an outside center and an incision biopsy of the tumor was done that revealed penile leiomyosarcoma. He was later referred to our institute, a tertiary care center, for further management. On examination of the patient at our institute, the patient was found to have 2 × 2 cm a typical nodular lesion in the proximal penile shaft. There was no gross lymphadenopathy in bilateral inguinal regions. Review of the histopathology examination after biopsy revealed tumor composed of spindle cells with hyperchromatic nuclei, inconspicuous nucleoli, and frequent mitoses. Tumor cells also stained positive for smooth muscle antigen (SMA) consistent with diagnosis of leiomyosarcoma of penis [Figures 1c and 1d]. As a part of staging, the patient was subjected to F-18 FDG PET/CT examination 2 months after the biopsy (this delay was due to late reporting of the patient to our institute from the peripheral center). The CT scan revealed moderate FDG uptake in the periphery of an ill-defined heterogeneously enhancing soft tissue lesion 2.9 × 2.2 cm in size involving corpora cavernosa on the left side of the distal penile shaft. This mass showed slightly thick, peripheral rim enhancement on the contrast-enhanced CT images corresponding to an area of increased F-18 FDG uptake, with an internal homogeneous region of low density, compared to the adjacent normal shaft of the penis, representing residual disease [Figures 1a and 1b]. No significant F-18 FDG uptake was noted in bilateral inguinal or iliac lymph nodes. Taking into consideration possible microscopic lymph node metastases total penectomy and bilateral inguinal lymphadenectomy was planned and the patient was counseled. However, the patient refused to undergo lymphadenectomy and only total penectomy was done. On follow-up after 8 months, the patient was found to be disease free.
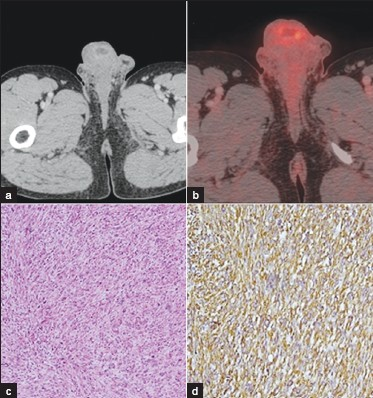
- (a) Contrast-enhanced axial CT through the penis demonstrates a low attenuating lesion in the corpora of the penis with peripheral enhancement. No inguinal lymphadenopathy present. (b) F18-FDG PET image fused with corresponding CT demonstrates increased FDG uptake in the periphery of an ill-defined lesion within the corpora of the penis. (c) Histopathological examination shows tumor composed of spindle cells with hyperchromatic nuclei, inconspicuous nucleoli with frequent mitoses (d) Histopathological examination shows positivity for smooth muscle antigen
DISCUSSION
Penile cancer is a rare neoplasm and accounts for approximately 0.4% of all male malignancies.[12] The most common primary malignant neoplasm of the penis is squamous cell carcinoma, constituting more than 95% of cases, followed by metastatic neoplasms of the prostate, bladder, rectum, kidney, and testis, as well as those spreading by direct extension from the adjacent structures.[3] It accounts for 10–20 % of all malignancies in males in Asia, Africa, South America, and it has a prevalence of only 1% in Western countries.[2] Predisposing factors are phimosis, cigarette smoking, and human papilloma virus (HPV) infection. Other tumors of the genitourinary tract include sarcoma, melanoma, basal cell carcinoma, and lymphoma.[4] Sarcomas are uncommon penile neoplasms, which include epithelioid sarcoma, Kaposi sarcoma, leiomyosarcoma, and rhabdomyosarcoma.[5] In general, very little literature exists that discusses the management of penile leimyosarcoma, due to the rarity of disease. Penectomy is the usual surgical option. Role of routine lymphadenectomy is controversial as few authors have suggested that regional lymph node dissection is usually not indicated, since nodal metastases are uncommon.[6] In our case lymphadenectomy was planned; however, patient refused to undergo lymphadenectomy and was managed only with total penectomy. The CT findings of penile leiomyosarcoma are also rarely reported in literature in which the tumor may appear as a mass showing a relatively thick peripheral rim enhancement with internal regions of homogeneous low density, compared to the adjacent normal shaft of the penis, (similar to findings in our case) or as a soft tissue mass.[35] FDG uptake has been described in penile squamous cell carcinomas and F-18 FDG PET/CT has been shown to be useful in detection of lymph nodal and distant metastases in penile carcinoma.[78] F-18 FDG uptake has also been described in leiomyosarcomas and tumoral F-18 FDG uptake correlates well with the grade of the tumor in case of leiomyosarcomas.[9] F-18 FDG PET/CT plays an important role in diagnosis, staging, treatment response monitoring, and follow-up in patients with sarcomas. PET/CT is better in detecting recurrence than the conventional imaging.[10] This is the first case demonstrating F-18 FDG PET/CT findings in a case of penile leimyosarcoma.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/57/90955
REFERENCES
- Histopathology of malignant lesions of the penis. Urol Clin North Am. 1992;19:227-46.
- [Google Scholar]
- Imaging Findings of Sonography and Computed Tomography for a Penile Leiomyosarcoma. J Korean Soc Radiol. 2009;61:405-8.
- [Google Scholar]
- Scanning with 18F-FDG-PET/CT for detection of pelvic nodal involvement in inguinal node-positive penile carcinoma. Eur Urol. 2009;56:339-4.
- [Google Scholar]
- Fluorodeoxyglucose positron emission tomography in leiomyosarcoma: Imaging characteristics. Nucl Med Commun. 2009;30:546-9.
- [Google Scholar]
- Clinical applications of positron emission tomography in sarcoma management. Expert Rev Anticancer Ther. 2011;11:195-204.
- [Google Scholar]






