Translate this page into:
Bilateral Renal Lymphangiectasia: Radiological Findings by Ultrasound, Computed Tomography, and Magnetic Resonance Imaging
Address for correspondence: Dr. Khaled Youssef Elbanna, Department of Medical Imaging, King Abdul-Aziz Medical City (KAMC), National Guard Hospital, Riyadh - 11426, Saudi Arabia. E-mail: khaledbanna77@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Renal lymphangiectasia is a rare benign condition of the kidney without specific clinical presentations. Classic imaging findings are described in literature. Here, we present a case of renal lymphangiectasia with history of bilateral flank pain and abnormal renal function tests. The radiological appearance on ultrasound (US) and computed tomography (CT) showed features of bilateral renal lymphangiectasia but the patient refused invasive procedure for aspiration of the cysts. So, follow-up of the patient was done by magnetic resonance imaging (MRI). Imaging findings of our case on US, CT, and MRI are discussed along with details of the additional finding of dilated retroperitoneal lymphatic channels, cisterna chyli, as well as the thoracic duct.
Keywords
Cisterna chyli
MRI
renal lymphangiectasia
thoracic duct
INTRODUCTION

Retroperitoneal lymphangiectasia is a rare condition accounting for ~1% of all lymphangiectasias.[1] Lymphangiectasia is a developmental disorder with failure of development of normal communication between the lymphatic tissue and the rest of the lymphatic system leading to lack of normal drainage of lymphatic fluid with subsequent cystic dilatation of the lymphatic channels.[2]
CASE REPORT
38-year-old male presented to the emergency department with bilateral flank pain. Physical examination was normal and vital signs were within normal limits. Urine analysis was nonspecific. Blood tests revealed high creatinine level reaching 155 μmol/l (normal: 50–110 μmol/l), blood urea nitrogen (BUN) was 9.7 mmol/l (normal: 8.0–16.4 mmol/l), and estimated glomerular filtration rate (eGFR) was 68 ml/min (normal: above 60 ml/min).
Non-contrast computed tomography (CT) of the abdomen was done to rule out obstructive ureteric stones. CT scan showed perirenal and peripelvic encysted fluid densities without hydronephrosis, nephrolithiasis, or urolithiasis [Figure 1a and b].
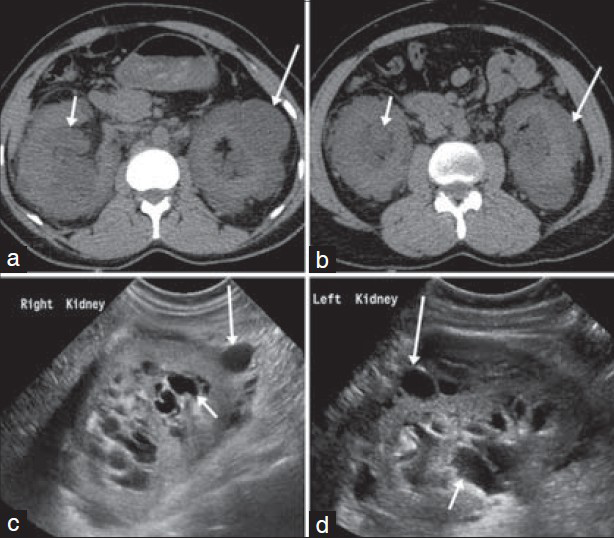
- 38-year-old male presented with bilateral flank pain and was later diagnosed with bilateral renal lymphangiectasia. (a and b) Axial non-contrast CT images at the level of the kidneys show perirenal (long arrows) and peripelvic (short arrows) cysts with fluid density. (c and d) Sonography of the kidneys along the longitudinal plane show perirenal (long arrows) and peripelvic (short arrows) cysts with septations and clear fluid contents together with increased parenchymal echogenicity.
Ultrasonography (US) was done to confirm the findings. US revealed bilateral septated cysts surrounding the kidneys and also cysts inside the renal sinuses. The contents of the cysts were anechoic indicating clear fluid content. Hyperechoic renal parenchyma was noted bilaterally [Figure 1c and d].
The combination of imaging findings was convincing enough to make the diagnosis of bilateral renal lymphangiectasia.
The patient received conservative treatment including analgesia, and was discharged from the emergency department and referred for urology consultation. Patient refused to get aspiration of cysts done to confirm the radiological diagnosis. The patient developed hypertension with persistently slightly high serum creatinine level.
Radiological follow-up was done by magnetic resonance imaging (MRI) 1 year after the initial CT. Contrast-enhanced MRI was done and confirmed the distribution of the cysts that showed septations with low signal in T1-weighted images (T1WI) and high signal in T2-weighted images (T2WI) without contrast pooling in the delayed post-contrast images, indicating absence of communication with the renal collecting system. The renal cortex showed high T2 signal [Figure 2a and b].
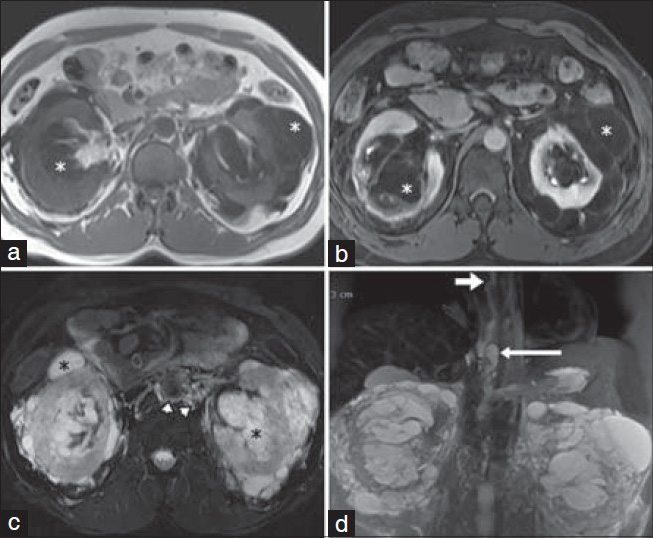
- 38-year-old male presented with bilateral flank pain and was later diagnosed with bilateral renal lymphangiectasia. (a) MRI axial T1-weighted image of the kidneys and (b) Axial post-contrast T1-weighted delayed phase image show the cysts have dark T1 signal (white asterisks) with lack of contrast pooling inside the cysts in the delayed phase, confirming absence of communication with the renal collecting system. (c) Axial T2 fat-suppressed weighted image and (d) coronal reformatted maximum intensity projection T2 fat-suppressed image demonstrate cysts with fluid signal intensity (black asterisks) and dilated retroperitoneal lymphatic channels (arrowheads), together with dilatation and tortuosity of the cisterna chyli (long arrow) and thoracic duct (short arrow).
Also, dilated retroperitoneal lymphatic channels, cisterna chyli, and thoracic duct were noted and best appreciated in axial T2 fat-suppressed images and maximum intensity projection (MIP) reformatted coronal images [Figure 2c and d].
DISCUSSION
Only 22 cases of renal lymphangiectasia have been described during the past 23 years in the literature. It has an equal incidence in males and females and can present in the age group from 8 to 74 years. Lymphatic dilatations are seen in perirenal, peripelvic, and intrarenal locations. That is why, the new term “renal lymphangiectasia” is more descriptive of the nature of the disease. So, it has replaced older terms of the disease, e.g. renal lymphangiomatosis, renal lymphangioma.[3]
It is almost always bilateral and the common presentations include flank pain, abdominal distension, hematuria, and proteinuria. Initially, the blood pressure is normal. Renal function is usually abnormal. Renal lymphangiectasia can be exacerbated by pregnancy.[4]
Clinical manifestations and typical imaging criteria are helpful to differentiate renal lymphangiectasia from similar conditions. For example, variable-sized scattered parenchymal cysts are seen in adult polycystic kidney disease with or without hepatic and pancreatic cysts. Focal masses with soft tissue attenuation are seen in lymphoma, while cysts with fluid attenuation are found in renal lymphangiectasia. Nephroblastomatosis is another differential diagnosis that presents in children with renomegaly and soft-tissue masses.[5]
Complications include hemorrhage, rupture, ascites, and hypertension secondary to perirenal fluid collection. Less commonly reported complication is venous thrombosis.[6]
Sonography frequently demonstrates anechoic lesions with increased through transmission and sharply defined thin wall. Fine echoes in the cysts are seen in cases with debris or hemorrhage. These cystic spaces extend along and into the peripelvic region as the larger lymphatic channels drain through the renal pedicle.[3]
CT examination reveals peripelvic/perirenal multiloculated cystic lesions with fluid attenuation ranging from 0 to 10 Hounsfield units while higher attenuations are secondary to intracystic hemorrhage. The walls and septations are usually thin and regular, but may also be thick and irregular. Rarely, retroperitoneal fluid collections may be present. Free intraperitoneal fluid may be seen in severe cases.[7]
The typical appearance on MRI of lymphangiectasia consists of cystic lesions that are hypointense on T1WI and hyperintense on T2WI. Also, the involved kidney may be enlarged with increased cortical intensity and decreased medullary intensity in T2WI.[5] This could be explained by obstructed intrarenal lymphatics and subsequent edema. Rarely, retroperitoneal perivascular tubular lesions may be present, in keeping with enlarged lymphatic vasculature.[8] Associated retroperitoneal perivascular thin lymphatic channels seen in MRI have been described by Kocaoglu et al.[5] Also, as in our case, MRI may detect the tortuous dilatation of cisterna chyli and thoracic duct.
Lymphatic vascular anomaly is one of the causes of dilatation of retroperitoneal lymphatic ducts. The dilated lymphatic ducts can decompress by rupturing into the urinary tract, resulting in a lymphatico-forniceal fistula and manifesting as chyluria.[9]
More recently, lymphoscintigraphy has been used to detect abnormal lymphatic flows associated with lymphangiectasia.[10]
Percutaneous drainage can be useful in the conservative management of symptomatic patients; however, surgery (cyst marsupialization) is considered as the last therapeutic measure and it may result in nephrectomy because these lesions tend to bleed easily during operation.[3]
CONCLUSION
Confident diagnosis of the rare disease of renal lymphangiectasia can be established by the radiological findings and radiologists should be aware of its imaging criteria to avoid misdiagnosis and help in early detection of the condition. MRI may have a special role among the different imaging modalities, as it can clearly assess the contents of the cysts as well as the extension of the disease and associated involvement of the retroperitoneal lymphatics and thoracic duct. Also, gadolinium can be given to patients with high creatinine levels, and gives an idea about renal parenchymal enhancement and, in turn, the renal function.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2015/5/1/6/150449
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Computed tomography findings in bilateral perinephric lymphangiomatosis. Urol Ann. 2010;2:26-8.
- [Google Scholar]
- Bilateral renal lymphangiomatosis: Imaging and histopathologic findings. Abdom Imaging. 2013;38:858-62.
- [Google Scholar]
- Exacerbation of familial renal lymphangiomatosis during pregnancy. AJR Am J Roentgenol. 1988;151:965-6.
- [Google Scholar]
- Retroperitoneal lymphangiectasia associated with bilateral renal vein thrombosis. Nephrol Dial Transplant. 1997;12:1701-3.
- [Google Scholar]
- Lymphoscintigraphy in the diagnosis of lymphangiomatosis. Clin Nucl Med. 2010;35:579-82.
- [Google Scholar]






