Translate this page into:
Barium Defecating Proctography and Dynamic Magnetic Resonance Proctography: Their Role and Patient’s Perception

*Corresponding author: Anuradha Chandramohan, Department of Radiology, Christian Medical College, Vellore, Tamil Nadu, India. anuradha.chandramohan@cmcvellore.ac.in
-
Received: ,
Accepted: ,
How to cite this article: Korula DR, Chandramohan A, John R, Eapen A. Barium defecating proctography and dynamic magnetic resonance proctography: Their role and patient’s perception. J Clin Imaging Sci 2021;11:31.
Abstract
Objectives:
The objectives of the study were to compare the imaging findings and patient’s perception of barium defecating proctography and dynamic magnetic resonance (MR) proctography in patients with pelvic floor disorders.
Material and Methods:
This is a prospective study conducted on patients with pelvic floor disorders who consented to undergo both barium proctography and dynamic MR proctography. Imaging findings of both the procedures were compared. Inter-observer agreement (IOA) for key imaging features was assessed. Patient’s perception of these procedures was assessed using a short questionnaire and a visual analog scale.
Results:
Forty patients (M: F =19:21) with a mean age of 43.65 years and range of 21–75 years were included for final analysis. Mean patient experience score was significantly better for MR imaging (MRI) (p < 0.001). However, patients perceived significantly higher difficulty in rectal evacuation during MRI studies (p = 0.003). While significantly higher number of rectoceles (p = 0.014) were diagnosed on MRI, a greater number of pelvic floor descent (p = 0.02) and intra-rectal intussusception (p = 0.011) were diagnosed on barium proctography. The IOA for barium proctography was substantial for identifying rectoceles, rectal prolapse and for determining M line, p < 0.001. There was excellent IOA for MRI interpretation of cystoceles, peritoneoceles, and uterine prolapse and substantial to excellent IOA for determining anal canal length and anorectal angle, p < 0.001. The mean study time for the barium and MRI study was 12 minutes and 15 minutes, respectively.
Conclusion:
Barium proctography was more sensitive than MRI for detecting pelvic floor descent and intrarectal intussusception. Although patients perceived better rectal emptying with barium proctography, the overall patient experience was better for dynamic MRI proctography.
Keywords
Barium proctography
Magnetic resonance proctography
Pelvic floor
Imaging
Accuracy
Diagnosis
INTRODUCTION
Pelvic floor disorders are a common health problem, especially among women, affecting more than 15% of multiparous women with 10–20% of patients seeking medical care in gastrointestinal clinics for evacuation dysfunction.[1] Chronic constipation leads to approximately 2.5 million visits to physicians in the United States every year.[2] In India, approximately 10% of the population suffers from constipation.[3] The pelvic floor is divided into three compartments – the anterior compartment (bladder and urethra), middle compartment (vagina and uterus), and posterior (anorectal) compartment. Damage to structures in any of the compartments may lead to pelvic floor dysfunction. Common symptoms of these patients include constipation, straining, lower back pain, urinary urgency, frequency and hesitancy, pain during intercourse, and pelvic floor spasm. Obstructed defecation syndrome is a pathological condition in which there is impaired defecation upon the urge to defecate. There are many risk factors which have been described for developing pelvic floor disorders including gender, increasing age, parity, prior pelvic surgeries, and chronic raised intra-abdominal pressure, the greatest risk factor being the female sex.[3-5]
Although physical examination and barium proctography may be sufficient for the diagnosis of mild pelvic floor dysfunction, there is an underestimation of compartments involved leading to inaccurate diagnosis in patients with moderate and severe symptoms. Clinical examination either underestimates the pelvic compartments involved or leads to misdiagnosis of the site of prolapse in 45–90% of patients and it is said to be unreliable for assessing evacuation abnormalities.[6-7] The recurrence rate after surgery is ~10– 30% and this may be attributed to multi-compartmental involvement, which may have been missed at the time of diagnosis.[8] Thus, imaging is required for accurate diagnosis and for pre-operative planning. Dynamic magnetic resonance (MR) proctography has been said to change the surgical management in around 67% of cases compared to 40% with conventional fluoroscopic studies.[9] In this study, we aim to directly compare the imaging findings of barium proctography and dynamic MR proctography and the patient’s perception of the procedure in a cohort of 40 patients with clinically suspected pelvic floor disorders.
MATERIAL AND METHODS
This is an institutional review board approved prospective study (IRB Min no:9135) done in a 3000 bedded tertiary care teaching hospital between November 2014 and November 2016.
Patients
Informed consent was obtained from all the 40 patients. Consecutive patients above 18 years of age who were referred for conventional barium proctography for clinically suspected pelvic floor disorders were consented to undergo dynamic MR proctography. The mean age of the patients was 43.65 years and 21 were females and 19 were males with the predominant symptom being constipation. The patient’s mother tongue was used to obtain consent and for all procedure related instructions. All the patients who consented to participate in the study underwent barium proctography first and this was followed by dynamic MR proctography within 1 week. Patients who underwent both barium proctography and dynamic MR proctography were included for the final analysis. Patients who consented for the study but did not undergo both procedures were excluded. Those who had incomplete procedure due to claustrophobia in the MRI gantry and those who could not initiate defecation during the MR proctography study were excluded from the final analysis. Figure 1 shows the study population and participants included for final analysis.
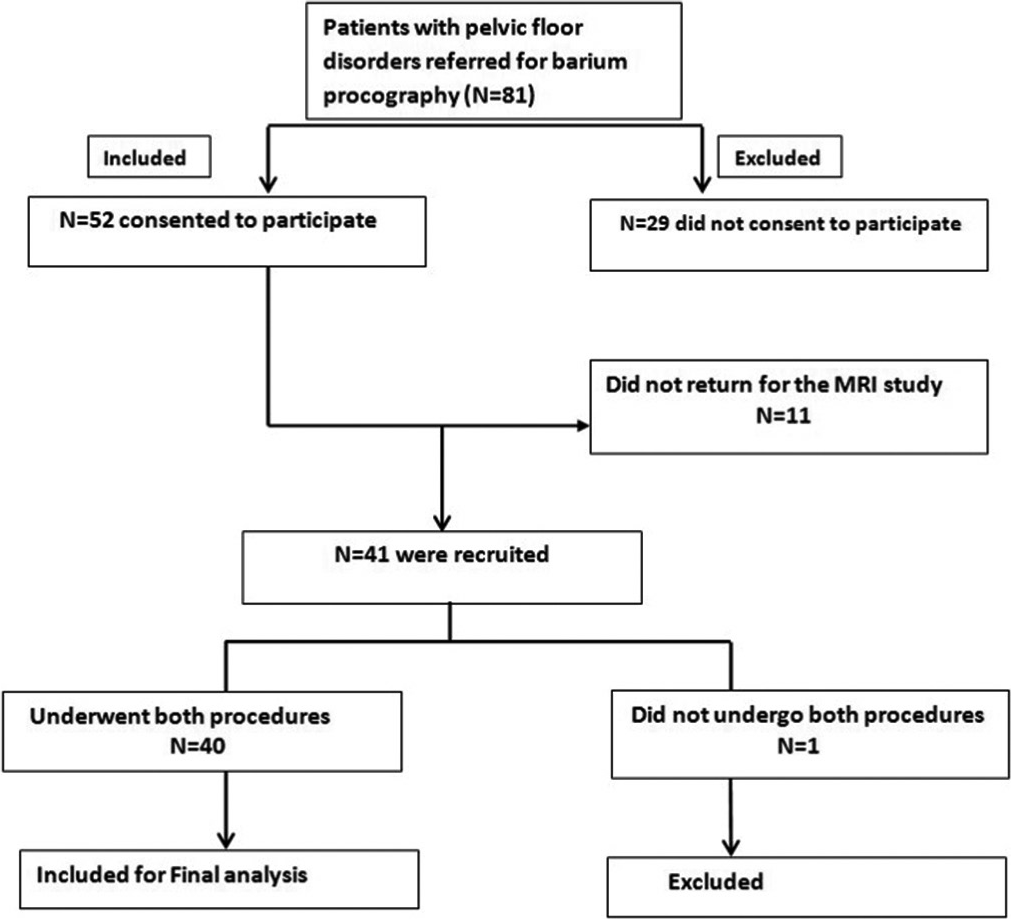
- Flow diagram of patients included in the study.
Barium defecography
All dynamic barium proctography studies were performed on the Luminos dRF Max, Siemens Healthineers. Patients were not given any dietary instructions. On the day of the procedure, patients were given instructions to perform the maneuvers just before the start of the procedure and once again following contrast instillation into the rectum.[10] Patients were placed in lateral decubitus position with the knees and hip joints flexed at 90°. Approximately 200–250 ml of thick barium paste was instilled into the rectum through a large bore soft rectal catheter until the patient developed rectal sensation. We did not opacify the vagina or the small bowel during the procedure. After ensuring adequate privacy with radiolucent curtains all around the commode, lateral spot images were obtained with the patient in sitting position on the commode at rest and during squeezing, straining and defecating phases. The last spot image was obtained after defecation to assess the degree of rectal emptying and barium trapping in a rectocele. Images were sent to picture archiving and communication system.
Technique of dynamic MR proctography
All dynamic MR proctography studies were carried out on a 1.5 T closed magnet MR imaging (MRI) scanner (Magnetom Avanto fit, Siemens Healthineers). No dietary instructions were given to the patients. Patients were instructed to empty the bladder 1 h before the MRI to ensure partial bladder distension during the procedure. Ultrasound gel was used as a rectal contrast. Patient was placed in a left lateral decubitus position and approximately 200–250 ml of ultrasound gel was instilled into the rectum through a wide bore soft rectal catheter until the patient developed rectal sensation. Patients were made to wear an incontinence pad and the MRI table was padded with liquid absorbing sheets. MRI was performed using body coil with the patient in supine position, legs slightly apart and a pillow under the knees. Patients were instructed to perform the squeeze, strain, and defecating maneuvers without moving.
MRI protocol included high resolution T2-weighted MRI in axial and coronal planes (repetition time/echo time [TR/ TE] =6110/81 m/s; field of view (FOV) of 25 cm; matrix of 250 × 384, section thickness of 4 mm and 3–4 min of imaging time) and dynamic mid sagittal steady-state sequence (TRUE FISP) obtained at rest, squeeze, strain, and defecation using the following parameters: TR/TE =47.1/1.33 msec; FOV =25 cm; matrix =216 × 240 matrix, slice thickness of 6 mm.
Image interpretation
Two experienced gastrointestinal radiologists with 15 years and 5 years of experience, blinded to each other’s findings interpreted both the barium proctography and dynamic MR proctography studies. To decrease the chance of bias during interpretation, radiologist 1 interpreted all the barium studies first and radiologists 2 interpreted all the MRI studies first and then vice versa. Definitions of terminologies used for image interpretation are given in Table 1[1,11,12] and Figure 2 shows the normal appearance. Imaging findings of barium proctography and dynamic MR proctography were compared and inter-observer agreement (IOA) was for certain key imaging features and was assessed within each modality separately.
| Terminology | Definition |
|---|---|
| Pubococcygeal line (PCL) | Line between the inferior margin of the symphysis pubis and the tip of the coccyx |
| Anterior compartment | The posterior and most inferior part of the bladder base is the reference point |
| Middle compartment | The most anterior and inferior aspect of the cervix or posterosuperior vaginal apex in patients who have undergone hysterectomy is the reference point |
| Posterior compartment | The anterior aspect of the anorectal junction is the reference point |
| H-line | Distance between the inferior border of the pubic symphysis and the posterior wall of the rectum at the level of the anorectal junction |
| M-line | Vertical line drawn perpendicularly from the PCL to the posterior end of the H line |
| Cystocele* | Abnormal descent of urinary bladder at rest/straining using the PCL as the reference line |
| Urethral hypermobility | Urethra rotates >30° from rest from the vertical to horizontal axis |
| Prolapse* | Abnormal descent of the anteroinferior aspect of cervix/posterosuperior vaginal apex from the PCL |
| Peritoneocele* and enterocele | Inferior herniation of the peritoneal pouch along the anterior rectal wall with an increased distance between the vagina and rectum and wide rectovaginal fossa. Enterocele - Abnormal descent of small bowel loops below the PCL |
| Ano-rectal angle | Angle between the midline of the anal canal and a line tangent to the posterior rectal wall. At rest the normal angle measures ~ 70–134° |
| Rectocele | Abnormal bulge of the anterior rectal wall into the posterior vaginal wall |
| Rectal intussusception | Infolding of the full thickness of the rectal wall into the rectum (intrarectal) or into the anal canal (intra-anal) or beyond (complete rectal prolapse) |
| Pelvic floor descent* | Excessive descent of the pelvic floor at rest or during defecation |
| Anismus | Lack of pelvic floor descent/ prominent puborectalis impression/ failure of opening of the anorectal angle |
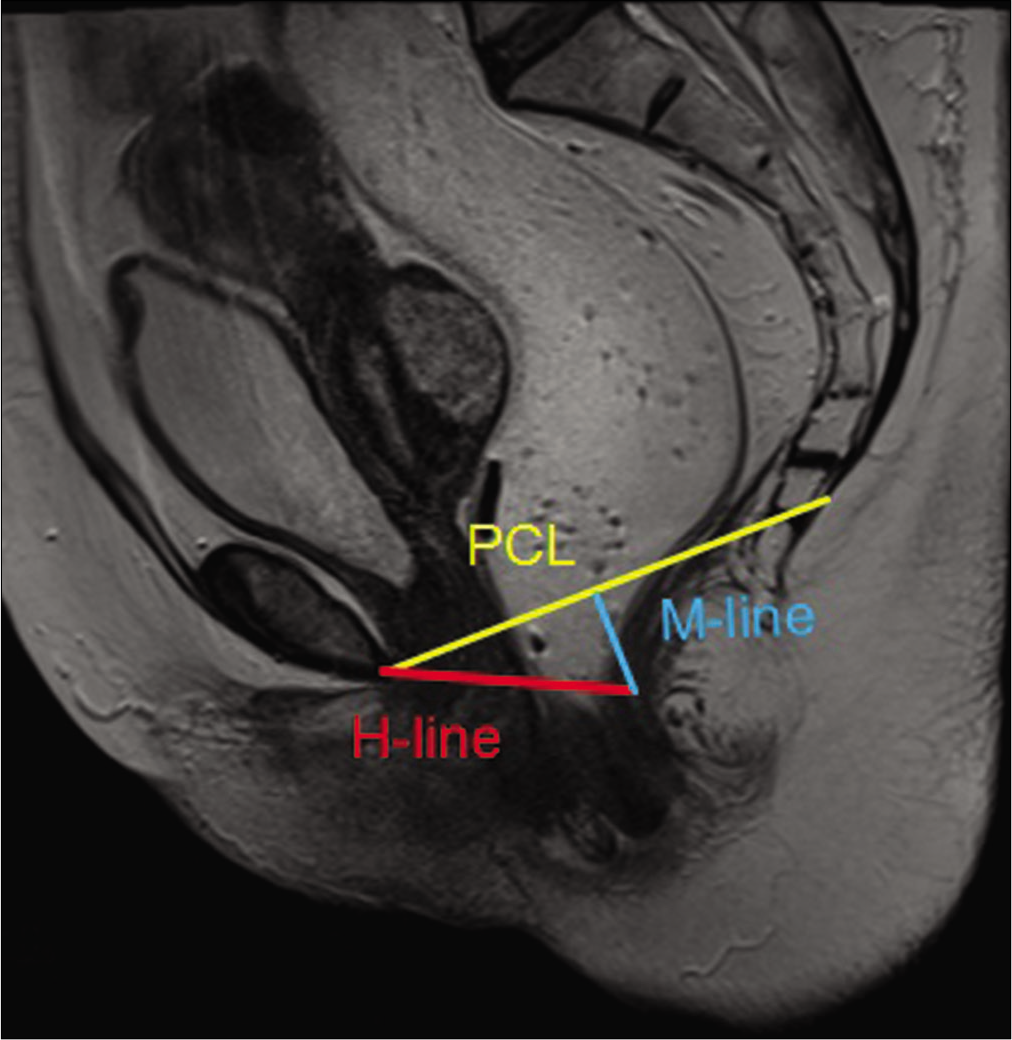
- T2W sagittal section of the pelvic magnetic resonance imaging depicting the normal pubococcygeal line (PCL) (yellow), H line (red) and the M line (blue). PCL is between the inferior margin of symphysis pubis and the tip of the coccyx. H-line is the distance between the inferior border of the pubic symphysis and the posterior wall of the rectum at the level of the anorectal junction and indicates the width of the levator hiatus. M-line is the vertical line drawn perpendicularly from the PCL to the posterior end of the H line. Mline indicates the degree of decent of the levator hiatus or the degree of pelvic floor laxity.
Patient’s perception
Immediately after the procedure, the study participants were given a short questionnaire to assess their perception of the procedure and the patient experience. There were questions to determine what the study participants perceived with regards to instructions, steps of the procedure, and how they felt during the procedure.
Statistical analysis
Statistical package (SAS Institute, Inc. (Cary, North Carolina) was used to perform the analyses. All continuous variables were expressed as the mean ± standard deviation (SD). Posterior compartment imaging findings identified on barium and MR proctography were compared. Student’s t-test was used to compare the difference between the continuous variables. Chi-square test was used to compare categorical values. Additional findings seen on MR proctography were assessed as number (N) and percentage (%). IOA was assessed using weighted Kappa. P <0.05 was considered statistically significant.
RESULTS
A total of 40 patients (21 females and 19 males) were included for final analysis. The mean age of the patients included in the study was 43.65 ± 14.2 years with a range of 21–75 years. The most common presenting symptom was constipation (n = 37, 92.5%). Other symptoms included dyspepsia, lower back pain, anal region pain, micturating difficulty, urge incontinence, and mass descending per rectum or vagina. The average time taken for the barium proctography study was ~12 min while the MRI proctography took ~15 min.
Table 2 and Figure 3 shows the patient’s perception of these procedures. While the mean patient experience score was significantly better for MRI study (p < 0.001), they perceived significantly higher difficulty in rectal evacuation compared to barium proctography (p = 0.003).
| Questions | Barium (%) | MRI (%) | Chi-square value, P-value |
|---|---|---|---|
| Contrast instillation | |||
| Comfortable | 28 (70) | 31 (77.5) | 0.581, 0.446 |
| Uncomfortable | 12 (30) | 9 (22.5) | |
| Holding rectal contrast | |||
| Easy | 32 (80) | 39 (97.5) | 6.135, 0.013 |
| Difficult | 8 (20) | 1 (2.5) | |
| Rectal evacuation | |||
| Easy | 37 (92.5) | 26 (65) | 9.038, 0.003 |
| Difficult | 3 (7.5) | 14 (35) | |
| Following instructions | |||
| Able to follow | 40 (100) | 38 (95) | 2.051, 0.152 |
| Unable to follow | 0 | 2 (5) | |
| Overall patient experience | |||
| VAS (0 to 10) | 3.43±8.5 | 8±0.1 | P<0.001 |
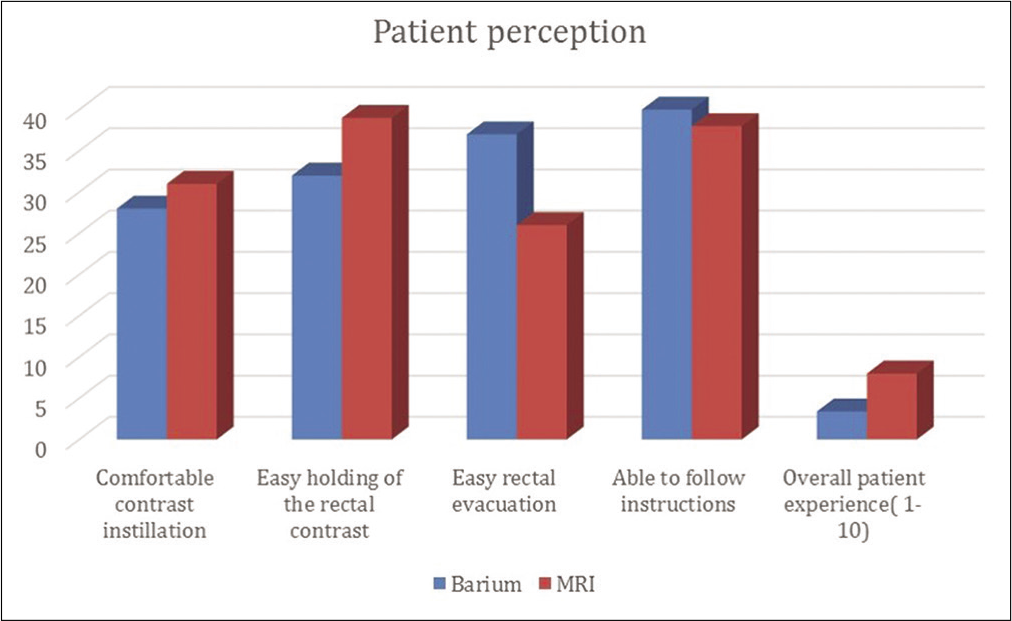
- Comparison of patient’s perception of barium and magnetic resonance imaging proctography.
Table 3 compares the barium and MRI imaging findings of the patients included in the final analysis. Significantly higher number of rectoceles (p = 0.014) was detected on MR proctography. On the other hand, a greater number of pelvic floor descent (p = 0.02) and intra-rectal intussusception (p = 0.011) were seen on barium proctography as also demonstrated in Figures 4-6. Table 4 shows the additional findings detected on MRI proctography. MRI proctography was useful in detecting the following additional findings in the anterior and middle compartment: 13 (32.5%) patients had small cystoceles; 12 (30%) patients had urethral descent; 12 (30%) patients had urethral rotation/funneling; 25 (62.5%) patients had uterine prolapse; and three (7.5%) patients had abnormalities of puborectalis such as muscle defects or thickening from scarring; one (2.5%) patient had a peritoneocele. Figures 7, 8 and multimedia 1 and 2 show these findings.
| Findings | Barium (%) | MRI (%) | P-value |
|---|---|---|---|
| Rectocele | 8 (20) Small: 7 (87.5) Medium: 1 (12.5) |
15 (37.5) Small: 14 (93.3) Medium: 1 (6.6) |
0.014 |
| Pelvic cavity widening | 23 (57.5) | 6 (15) | 0.165 |
| Pelvic floor descent | 37 (92.5) Mild–14 (38) Moderate–16 (43) Severe–7 (19) |
29 (72.5) Mild–10 (34.5) Moderate–12 (41.5) Severe–7 (24) |
0.02 |
| M line - >2 cm | 7 (17.5%) All were 2–4 cm |
13 (32.5) 2–4 cm-11 (85) 4–6 cm-2 (15) |
0.125 |
| Anorectal angle | Mean+2SD Barium | Mean+2SD MRI | |
| Rest | 111.45±14.8 | 100.87±13.1 | 0.002 |
| Squeeze | 110.75±15.1 | 91.4±14.7 | <0.001 |
| Defecation | 125.9±14.3 | 111.1±16.6 | <0.001 |
| Intra-rectal intussusception | 19 (47.5) | 15 (37.5) | 0.011 |
| Rectal prolapse | 2 (5) | 0 | 1.0 |
| Intra-anal intussusception | 3 (7.5) | 0 | 1.0 |
| Complete rectal voiding | 40 (100) | 40 (100) | – |
| Contrast trapping | 1 (2.5) | 0 | – |
| Animus | 1 (2.5) | 0 | – |
MR: Magnetic resonance, MRI: Magnetic resonance imaging
| Finding*** | MRI (%) |
|---|---|
| Increased puborectalis thickness | 1(2.5) |
| Defect in puborectalis | 2 (50) |
| Urethral descent | 12 (30) |
| Cystocele | 13 (32.5) Small–13 (100) Moderate–nil Large–nil |
| Urethral rotation/funneling | 12 (30) |
| Uterine prolapse | 25 (62.5) Mild–5 (20) Moderate–20 (80) Severe–nil |
| Peritoneocele | (2.5) |
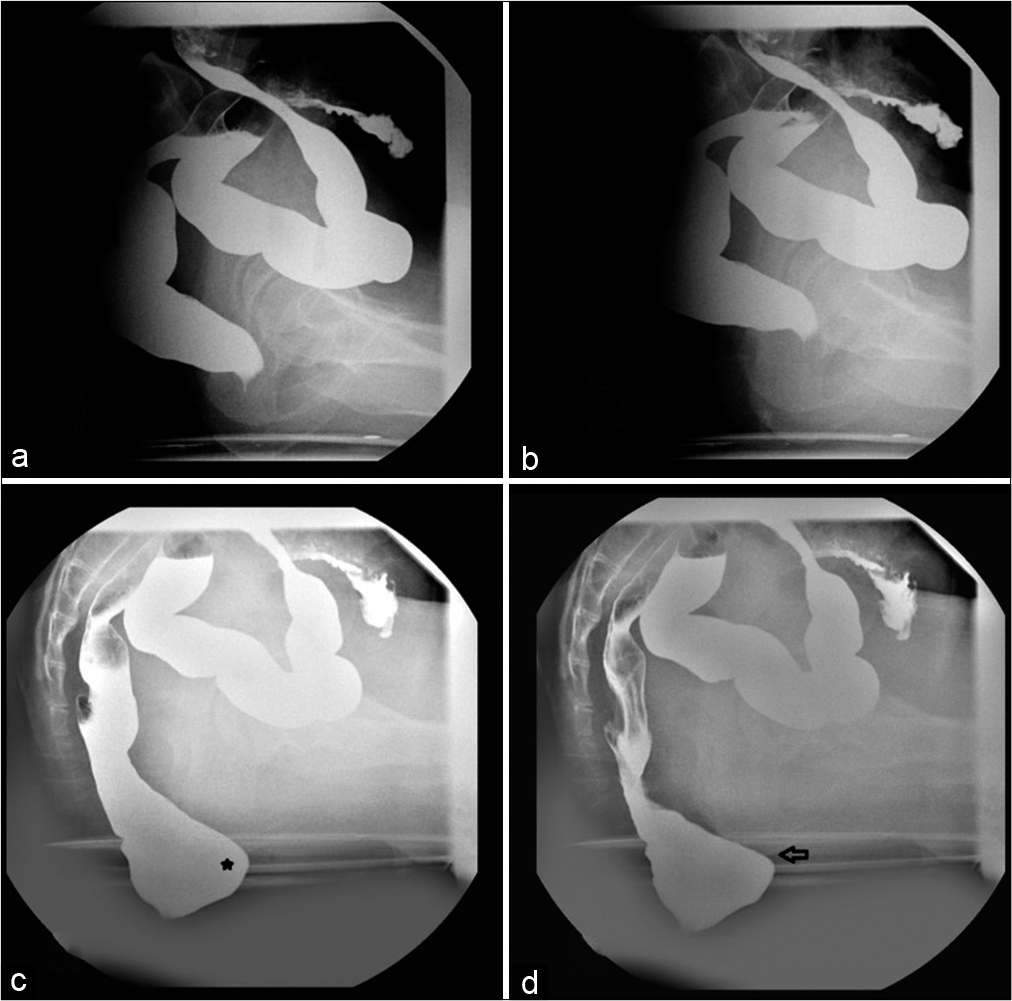
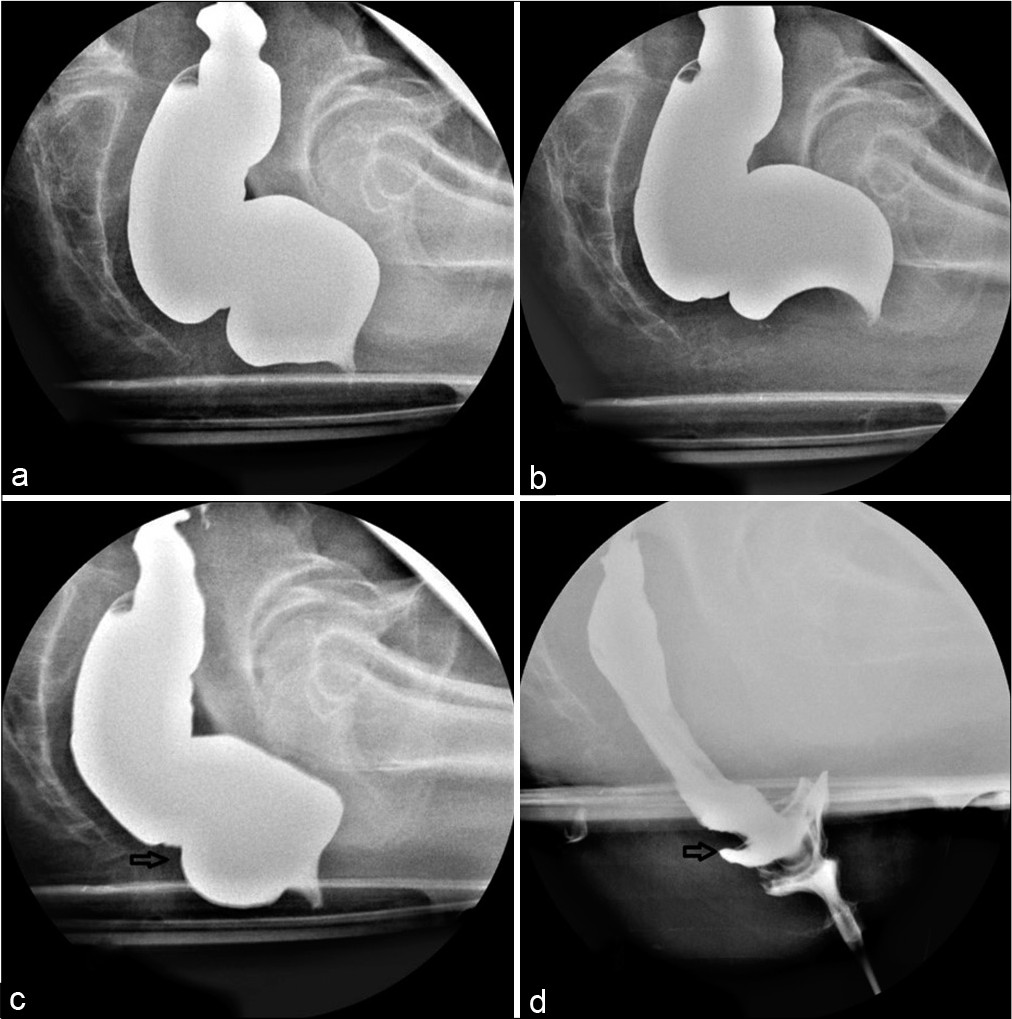
- Spot radiographs of Barium proctography study of a 36-year-old lady with constipation at rest (a), pelvic lift (b), straining (c) and defecating (d). There is a small anterior rectocele (asterisk) and moderate pelvic floor descent depicted by descent of the anorectal junction below the ischial tuberosity during strain and defecation (black arrow). Magnetic resonance imaging proctography did not demonstrate these findings.
- Spot radiographs of the Barium proctography study at (a) rest (b) pelvic lift (c) straining and (d) defecation of a 48-year-old lady with difficulty in defecation and micturition showed infolding of the rectal wall with a filling defect suggestive of rectorectal intussusception (arrows) and pelvic floor descent.
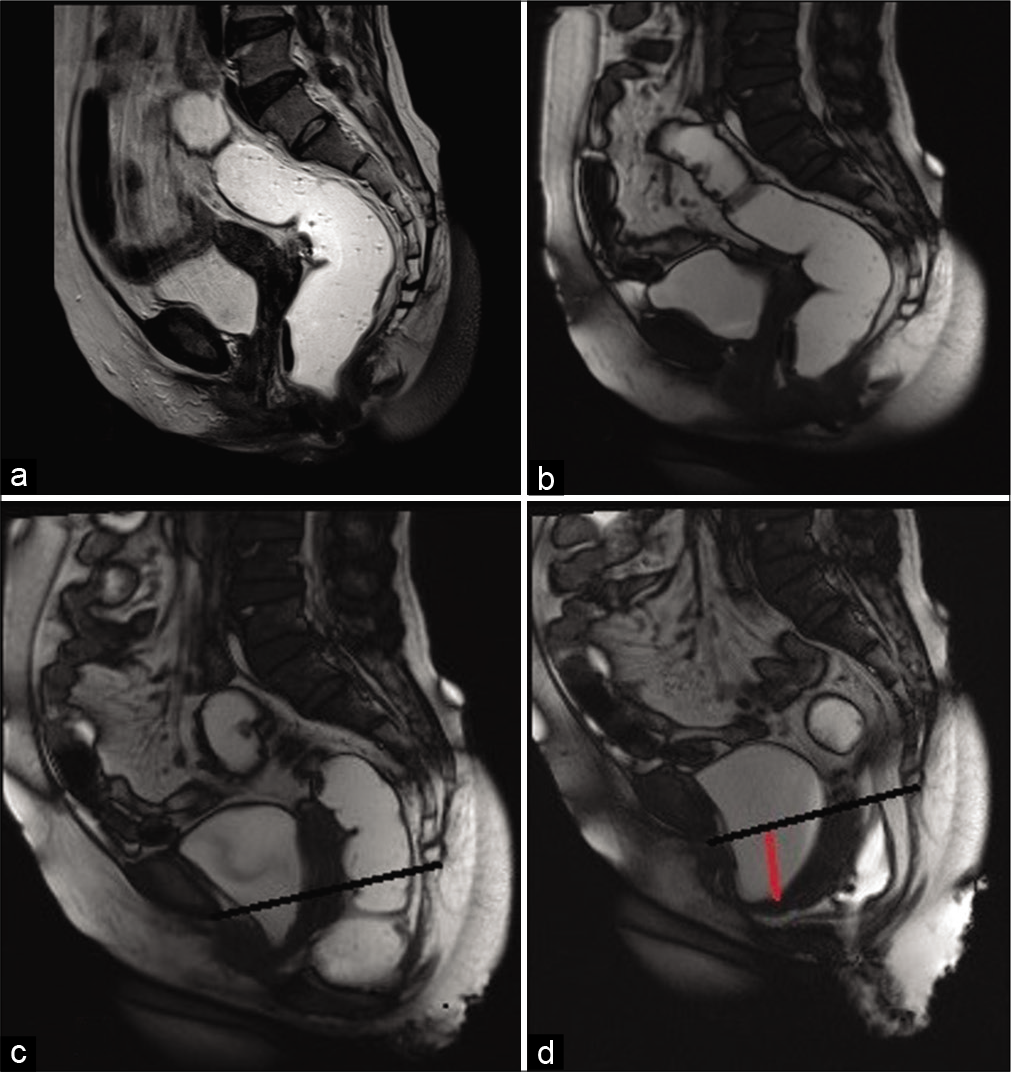
- Magnetic resonance imaging proctography of the same patient as in Figure 5 showed significant pelvic floor descent with additional findings of grade 2 cystocele (red line) however could not demonstrate the intussusception. The black line depicts the pubococcygeal line.

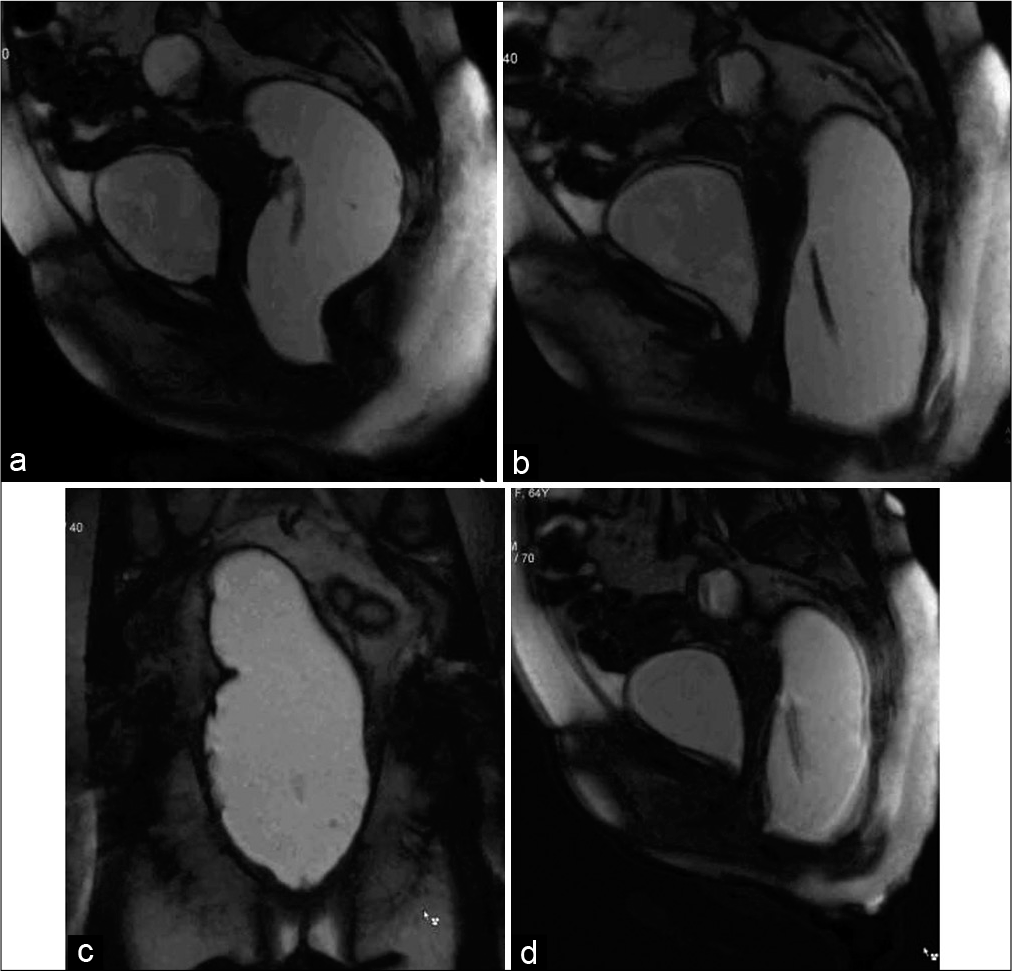
- Spot radiographs of the Barium proctography study at (a) rest (b) pelvic lift (c) straining and (d) defecation of a 40 year old female with suspected obstructed defecation syndrome and history of digital evacuation of faeces shows recto-anal intussusception (arrow in d), small anterior rectocele with barium trapping during defecation (asterisk) and moderate pelvic floor descent.

- Magnetic resonance imaging proctography of the same patient as in Figure 7 showed an anterior rectocele (asterisk), moderate pelvic floor descent and additionally depicted a grade 2 cystocele (red line). The black line depicts the pubococcygeal line.
Table 5 shows the IOA for imaging findings seen on barium and MR proctography. In interpreting barium proctography, the IOA was substantial for identifying rectoceles (k = 0.729, p < 0.001), rectal prolapse (k = 0.655, p < 0.001), and determining the M line (k = 0.610, p < 0.001) and was moderate for determining the anorectal angle (k = 0.570) and pelvic floor descent (k = 0.460, p < 0.001).
| Finding | Barium proctography | MRI proctography |
||
|---|---|---|---|---|
| Weighted Kappa | P-value | Weighted Kappa | P-value | |
| Rectocele | 0.729 | <0.001 | 0.386 | 0.004 |
| Pelvic cavity widening | 0.38 | 0.16 | 0.48 | 0.16 |
| Pelvic floor descent | 0.46 | <0.001 | 0.44 | <0.001 |
| M line - >2 cm | 0.61 | <0.001 | 0.61 | 0.125 |
| Anorectal angle | 0.446–0.575 | <0.001 | 0.652–0.84 | 0.02 |
| Anal canal length | - | 0.608–0.838 | <0.001 | |
| Intra-rectal intussusceptions | 0.119 | 0.308 | 0.028 | 0.766 |
| Rectal prolapse | 0.655 | <0.001 | - | |
| Puborectalis thickness | - | 0.65 | <0.001 | |
| Defect in puborectalis | - | 0.0 | 1.0 | |
| Cystocele | - | 0.83 | <0.001 | |
| Urethral descent | - | 0.64 | <0.001 | |
| Urethral funneling | - | 0.048 | 0.507 | |
| Peritoneocele | - | 1.0 | <0.001 | |
| Uterine prolapse | - | 0.85 | <0.001 | |
IOA: Inter-observer agreement, MR: Magnetic resonance, MRI: Magnetic resonance imaging
In interpreting MRI proctography, there was excellent IOA in interpreting cystoceles (k = 0.83, p < 0.001); peritoneoceles (k = 1, p < 0.001); uterine prolapse (k = 0.85, p < 0.001); and anal canal length (k = 0.83, p < 0.001). There was substantial agreement between the observers for determining the anorectal angle (k = 0.65, p < 0.001) using MRI. There was, however, only a fair agreement between both the observers in determining rectoceles (k = 0.38, p = 0.004).
Out of the 40 patients, 39 were managed conservatively and only patient had surgical pelvic floor repair in our institute.
In this patient, the MRI proctography could demonstrate the Grade 2 cystocele and uterine prolapse in addition to pelvic floor descent seen on the barium proctography and this was helpful in management.
DISCUSSION
Pelvic floor disorders are a commonly occurring health problem especially among women. When the patient’s symptoms are mild, physical examination may be sufficient for the diagnosis. However, when the patient’s symptoms are moderate or severe, routine examination may underestimate the compartments involved and lead to inaccurate diagnosis. Assessment of all three-compartment using conventional barium proctography involves opacification of small bowel and distension of bladder and rectum with contrast.[13] On the other hand, pelvic floor imaging using MRI is less invasive and has far superior soft-tissue resolution to depict abnormalities of all compartments. The concordance between clinical assessment and findings at dynamic MRI for disease staging has been found to be good with a slightly weaker correlation for findings in the posterior compartment.[6,14] MR proctography has been found to show more extensive abnormalities than physical examination alone.[15,16] Dynamic MR proctography has been said to change that the surgical management is around 67% of patients compared to 40% with conventional fluoroscopic studies.[9,17] For example, the treatment for an uncomplicated cystocele is retropubic colposuspension, however when the paravaginal fascia is detached, fascial repair is required. Anterior rectocele repair by surgery may be performed either by trans anal or transvaginal approach. If there is a rectal intussusception, posterior fixation of the rectum may be included as well. MRI study may also help in identifying other incidental pathologies which may additionally impact patient’s management. Compared to MRI, which is free of radiation, barium proctography confers a typical radiation dose of ~2–3 mSv. Thus, in our study, we aimed to compare barium and MRI proctography with a view to assess the strengths and weaknesses of these procedures in terms of imaging findings and patient’s perception.
We found significant difference in the number of rectoceles diagnosed on barium and MR proctography, with more numbers detected with MR studies, p = 0.014. Our results were similar to one previous study, which found that the sensitivity and specificity of detecting rectoceles on MR colplocystorectography (69% and 96%, respectively) were slightly higher than barium proctography (50% and 93%, respectively).[18] These results could be attributed to superior spatial resolution of MRI. However, the additional rectoceles detected on MRI were only small in size and the clinical significance of this finding is questionable. In our study, the IOA for detection of rectocele was substantial for barium studies (k = 0.729) compared to moderate for MR studies (k = 0.386). This is in contrast to the previous studies, which reported a substantial to good agreement between both the procedures in detecting rectoceles with a kappa of 0.690. However, these studies reported a significant difference in the size of the rectoceles detected.[16-18]
Significantly higher number of pelvic floor descent and intrarectal intussusception was detected on barium proctography, which may be due to barium proctography studies being conducted in a physiological position compared to supine position of MRI studies in a closed magnet. This may also be the reason for significant differences seen in the anorectal angle measured in barium and MR proctography studies in all three phases – rest (p = 0.002), squeeze (p < 0.001) and defecation (p < 0.001). Our findings are in line with a previous study, which showed ~31% higher detection of intra-rectal intussusception on barium proctography with only low IOA (k = 0.209) for this finding.[17] Another study has also shown a significant difference in the detection of rectal prolapse between conventional barium and MR proctography.[19] These differences have been attributed to failure of complete rectal evacuation on the MR studies by previous workers. Our study confirms this theory by demonstrating a significant difference in patient’s perception of rectal evacuation between the two procedures with more patients perceiving incomplete evacuation after MR proctography.
MRI proctography was useful in detecting additional anterior and middle compartment findings, which would not be identified on the barium proctography. These included cystocele (32.5%); urethral descent and urethral hypermobility (30%); uterine prolapse (62.5%); puborectalis muscle abnormalities (7.5%); and peritoneocele (2.5%). Furthermore, we found that the overall patient experience score was superior for MR proctography compared to barium studies (P < 0.001). Similar findings have been reported by other workers.[14]
Our study is not without limitations. The index studies being compared in this study were performed in different positions. Thus, the differences in the imaging findings of these two modalities may have been due to differences in the position, rather than superiority of a modality. Second, the more symptomatic patients may not have consented, and this may have introduced bias. Third, we do not have a dedicated pelvic floor clinic in our setting. Majority of our patients were being referred by colorectal surgeons. This may have led to more posterior compartment findings due to referral bias.
- Dynamic magnetic resonance imaging proctography of a 40 year old female with difficulty in defecation and micturition, in the pelvic lift phase (a), straining phase (b and c) and in the defecation phase (d) showing pelvic floor descent, widening of the pelvic cavity, small cystocele and urethral hypermobility. Video is accessible from the portal.
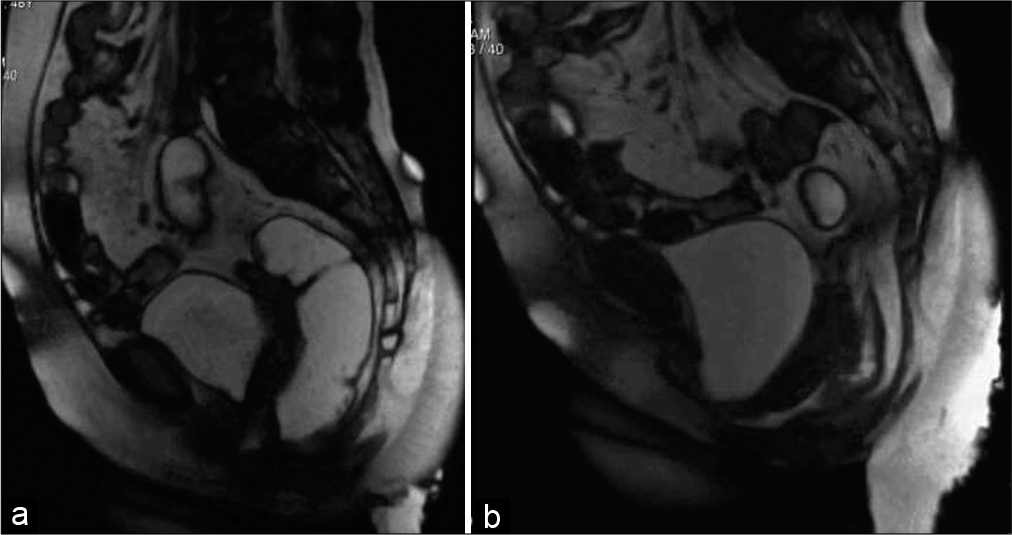
- Dynamic magnetic resonance imaging proctography (of same patient as in Figure 5 in the straining (a) and defecation phase (b) showing severe pelvic floor descent, urethral hypermobility and moderate cystocele. Video is accessible from the portal.
CONCLUSION
Assessment of the anterior and middle compartment in addition to the posterior compartment gives MRI proctography an added advantage over barium proctography. In our study, MRI proctography findings were comparable to barium proctography in the assessment of pelvic floor disorders. There was an overall better patient experience with MR proctography, though patients experienced incomplete evacuation more commonly with MR proctography compared to barium studies. However, in patients with predominantly posterior compartment symptoms, barium proctography may be adequate. There was good to substantial IOA in the assessment for most parameters on both studies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- MR imaging of the pelvic floor: Defecography. Magn Reson Imaging Clin N Am. 2013;21:427-45.
- [CrossRef] [PubMed] [Google Scholar]
- Self-reported uterine prolapse in a resettlement colony of north India. J Midwifery Womens Health. 2000;45:343-50.
- [CrossRef] [Google Scholar]
- Prevalence of urinary incontinence and other urological problems during pregnancy: A questionnaire based study. Arch Gynecol Obstet. 2009;279:845-51.
- [CrossRef] [PubMed] [Google Scholar]
- Occult stress incontinence in women with pelvic organ prolapse. Int J Gynaecol Obstet. 2007;97:31-4.
- [CrossRef] [PubMed] [Google Scholar]
- Association of compartment defects in pelvic floor dysfunction. Am J Roentgenol. 1999;172:439-44.
- [CrossRef] [PubMed] [Google Scholar]
- MR defecography in patients with fecal incontinence: Imaging findings and their effect on surgical management. Radiology. 2006;240:449-57.
- [CrossRef] [PubMed] [Google Scholar]
- Does conventional defecography has a role to play in evaluation of evacuatory disorders in Indian population? Indian J Radiol Imaging. 2013;23:92-6.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging-based assessment of the female pelvic floor. Radiographics. 2014;34:1417-39.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review of clinical studies on dynamic magnetic resonance imaging of pelvic organ prolapse: The use of reference lines and anatomical landmarks. Int Urogynecol J. 2009;20:721-9.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic floor descent in females: Comparative study of colpocystodefecography and dynamic fast MR imaging. J Magn Reson Imaging. 1999;9:373-7.
- [CrossRef] [Google Scholar]
- Dynamic half Fourier acquisition, single shot turbo spin-echo magnetic resonance imaging for evaluating the female pelvis. J Urol. 2000;164:1606-13.
- [CrossRef] [Google Scholar]
- MRI in colorectal surgery: Dynamic magnetic resonance imaging In: Wexner SD, Zbar AP, Pescatori M, eds. Complex Anorectal Disorders: Investigation and Management. London: Springer; 2005. p. :322-50.
- [CrossRef] [Google Scholar]
- MR-Based three-dimensional modelling of the normal pelvic floor in women. Am J Roentgenol. 2000;174:657-60.
- [CrossRef] [PubMed] [Google Scholar]
- Barium proctography vs magnetic resonance proctography for pelvic floor disorders: A comparative study. Colorectal Dis. 2012;14:1224-30.
- [CrossRef] [PubMed] [Google Scholar]
- Dynamic MR colpocystorectography. A new method for evaluating pelvic floor descent and genital prolapse. Aktuelle Radiol. 1996;6:182-6.
- [Google Scholar]
- Pelvic floor imaging: Comparison between magnetic resonance imaging and conventional defecography in studying outlet obstruction syndrome. Radiol Med. 2013;118:23-39.
- [CrossRef] [PubMed] [Google Scholar]






