Translate this page into:
Asymptomatic Urolithiasis Complicated by Nephrocutaneous Fistula
Address for correspondence: Dr. Marion Hamard, Department of Imaging and Medical Information Sciences, Service of Radiology, University Hospitals of Geneva, Rue Gabrielle-Perret-Gentil 4, CH-1205 Genève, Switzerland. E-mail: marion.hamard@hcuge.ch
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Asymptomatic spontaneous nephrocutaneous fistula is a rare and severe complication of chronic urolithiasis. We report a case of 56-year-old woman with a nephrocutaneous fistula (NFC) which developed from a superinfected urinoma following calyceal rupture due to an obstructing calculus in the left ureter. The patient was clinically asymptomatic and came to the emergency department for a painless left flank fluctuating mass. This urinoma was superinfected, with a delayed development of renal abscesses and perirenal phlegmon found on contrast-enhanced uro-computed tomography (CT), responsible for left renal vein thrombophlebitis and left psoas abscess. Thereafter, a 99 mTc dimercaptosuccinic acid (DMSA) scintigraphy revealed a nonfunctional left kidney, leading to the decision of left nephrectomy. Chronic urolithiasis complications are rare and only few cases are reported in medical literature. A systematic medical approach helped selecting the best imaging modality to help diagnosis and treatment. Indeed, uro-CT scan and renal scintigraphy with 99 mTc-DMSA are the most sensitive imaging modalities to investigate morphological and functional urinary tract consequences of NFC, secondary to chronic urolithiasis.
Keywords
Calyceal rupture
hydronephrosis
nephrectomy
nephrocutaneous fistula
surinfected urinoma
thrombophlebitis

Introduction
Asymptomatic NFC is a rare phenomenon and only few cases are reported in literature. It is usually associated with urinary tract infection secondary to chronic obstructive urolithiasis. We report this unusual asymptomatic complication of a superinfected urinoma and explain the associated diagnostic imaging workup that helped define therapeutic decisions.
Case Report
A healthy 56-year-old-woman was admitted to the emergency department for a painless left flank fluctuating mass, progressively growing over 3 months [Figure 1e], with recent externalization of pus. Blood tests were almost normal, excepted a slight elevation of white blood cell (11.5 G/L), and of C-reactive protein (47 mg/L).
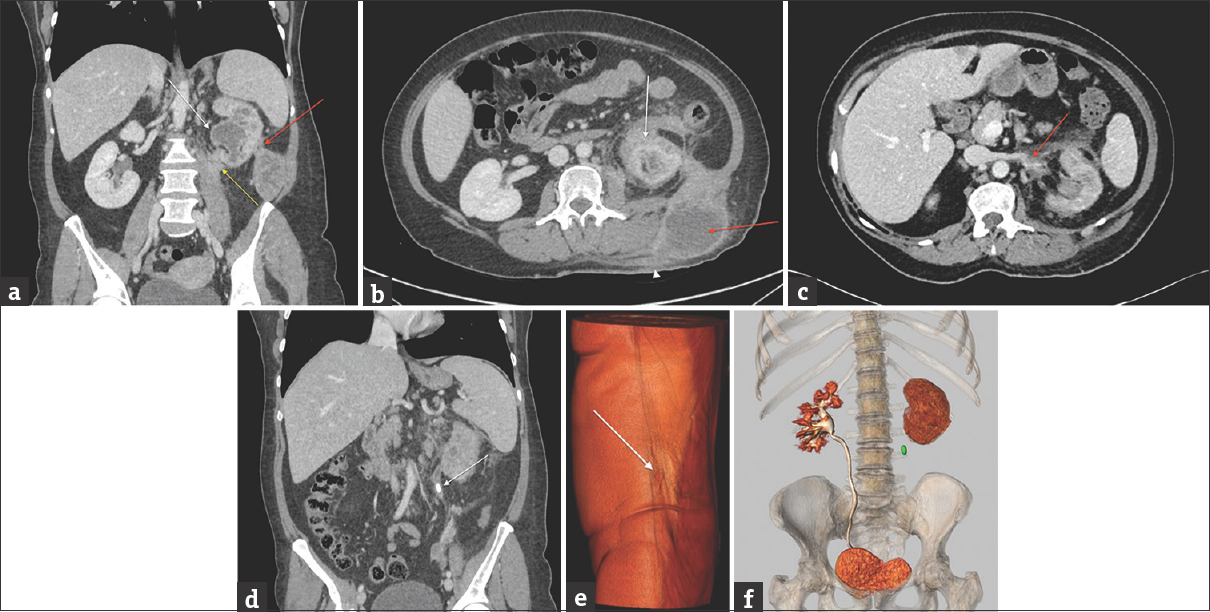
- (a) Contrast-enhanced abdominal computed tomography obtained to characterize the initial ultrasound imaging findings. Contrast-enhanced abdominal computed tomography reformation in a coronal plane with soft tissue window shows the communication (red arrow) between the perinephric abscess and the posteroinferior aspect of the left kidney. Hydronephrosis (white arrow) and cortical atrophy suggest chronic obstructive uropathy. Perinephric fat infiltration extends into the left psoas muscle (yellow arrow). (b) Contrast-enhanced abdominal computed tomography in axial plane at the renal level with soft tissue window shows heterogeneous thickening adjacent to the superior pole of the left kidney, with confluent cortical abscesses and an intense inflammatory stranding of the perirenal fat (white arrow). This infiltration extends into the parietal lumbar abscess (red arrow) which fistulizes to the skin (white arrowhead). (c) Contrast-enhanced abdominal computed tomography in axial-oblique plane at the level of the left renal vein with soft tissue window shows the occlusion of the proximal aspect of this vein (red arrow), surrounded by inflammatory changes in the adjacent fat, consistent with thrombophlebitis. (d) Contrast-enhanced abdominal computed tomography reformation in the coronal plane with soft tissue window shows the obstructing left ureteral calculus (white arrow). (e) Three-dimensional volume-rendered image in coronal plane from the excretory phase of the abdominal and pelvic computed tomography shows the left lumbar ureteral calculus (green spot) and no excretion of contrast into the left collecting system. By comparison, the right collecting system is well delineated by the normal excretion of intravenously administered iodinated contrast media. (f) Three-dimensional volume-rendered abdominal computed tomography image reveals a small red spot corresponding to the nephrocutaneous fistula (white arrow) can be depicted at the level of the left dorsolumbar fluctuating mass. Based on these images and on the clinical presentation, the radiologist concludes to a nephrocutaneous fistula related to an infected urinoma secondary to an obstructing left ureteral stone and pelvicalyceal rupture.
Initial ultrasonography showed a subcutaneous left parietal dorsolumbar multiloculated collection, abutting the posteroinferior aspect of the left kidney with associated left hydronephrosis [Figure 2].
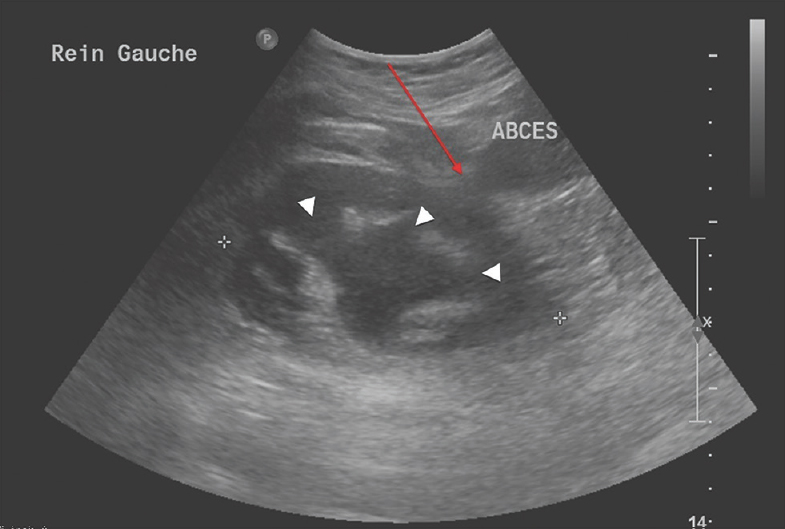
- A 56-year-old woman presents to the emergency department for a left painless dorsolumbar fluctuating mass which was progressively growing over 3 months. Ultrasonography was the first imaging study obtained. A long-axis view of the left kidney shows subcutaneous and parietal multiloculated heterogeneous hypoechoic collections, compatible with abscess adjacent to the left kidney (red arrow). Moderate left hydronephrosis is also present (white arrowheads).
The patient then underwent a contrast-enhanced abdominal computed tomography (CT) with uro-CT protocol. The left kidney was smaller than the contralateral kidney, with diffuse cortical atrophy and hydronephrosis [Figure 1a], suggestive of a chronic obstructive nephropathy. There were small confluent renal cortical abscesses, irregular perinephric fluid attenuation collections, and inflammatory changes in the perinephric fat [Figure 1b]. This phlegmon surrounded the distal portion of the left renal vein, which was occluded [Figure 1c]. Infiltrative changes extended into the left psoas muscle [Figure 1a] and a fistulous tract was demonstrated between the perinephric collections and the skin [Figure 1e and b].
A large obstructing calculus was present in the left lumbar ureter [Figure 1d], and there was no excretion of iodinated contrast from the left kidney on excretory phase images [Figure 1f] of uro-CT.
First, the calculus was removed endoscopically with a left ureteral stent placed, and antibiotics were administrated.
Because the clinical condition of the patient did not improve after few days of antibiotic therapy, a renal scintigraphy with 99 mTc-dimercaptosuccinic acid (DMSA) was proceeded and revealed a nonfunctional left kidney with normal radionuclide uptake by the right kidney [Figure 3]. Decision was then made to perform total left nephrectomy.
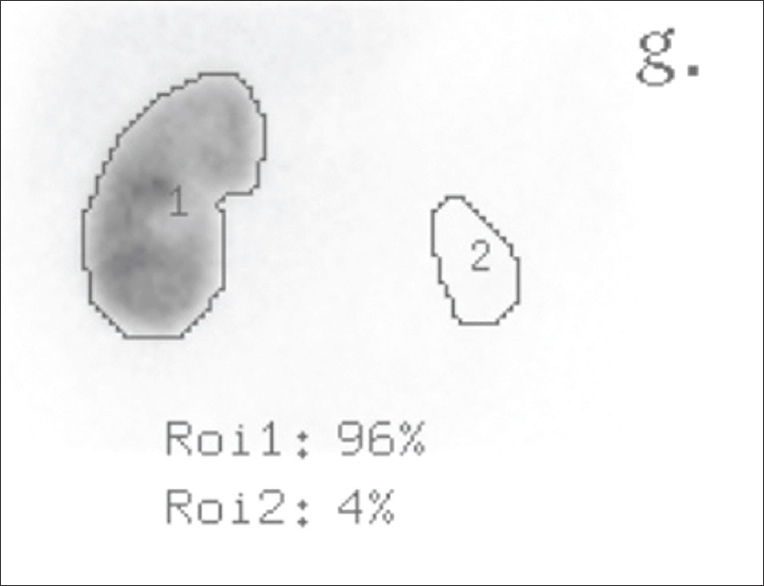
- Ultrasonography and computed tomography showed an infected urinoma with left pelvicalyceal rupture, secondary to an obstructive calculus with nephrocutaneous fistula. The calculus was endoscopically removed and a left ureteral stent was placed, with an antibiotic coverage. The clinical condition of the patient did not improve after antibiotic therapy. A planar image from 99 mTc-dimercaptosuccinic acid cortical renal scintigraphy was performed to estimate the remaining left kidney function and shows the uptake percentages of the radionuclide by the normal right kidney (Roi 1) and by the nonfunctional left kidney (Roi 2), estimated to 4%. The miniscule remaining left renal function leads to the decision to perform total left nephrectomy.
Pathology of the operatory specimen revealed subacute pyelonephritis with severe glomerular sclerosis and tubular atrophy, with an aspect of pseudothyroidization. This thyroid-like appearance is a common finding in chronic pyelonephritis, obstructive nephropathy, and sometimes in renal allograft specimens, which is made up of a colloid-like hyaline cast formation of Tamm-Horsfall glycoprotein.[1]
Many conglomerate microcalculi were seen in the ureter [Figure 4]. Chronic fibroinflammatory tissue was present in the perinephric fat and cultures grew Escherichia coli.
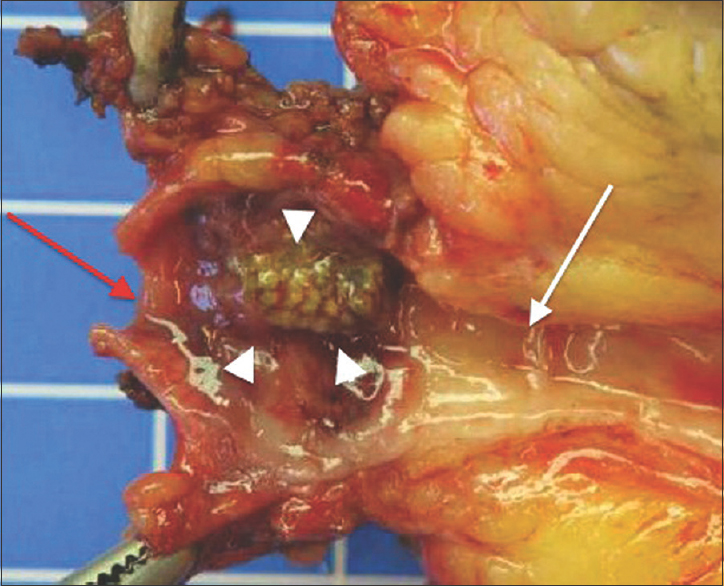
- This patient undergoes a left nephrectomy for infected urinoma with nonfunctional kidney, secondary to an obstructive calculus, calyceal rupture, and nephrocutaneous fistula. A picture of the pathological specimen of the left ureter at the level of the obstruction shows a left ureteral obstruction by a conglomerate of microstones (white arrowheads). The proximal ureter (white arrow) is surrounded by an intense chronic fibroinflammatory process while the distal ureter is normal (red arrow).
Discussion
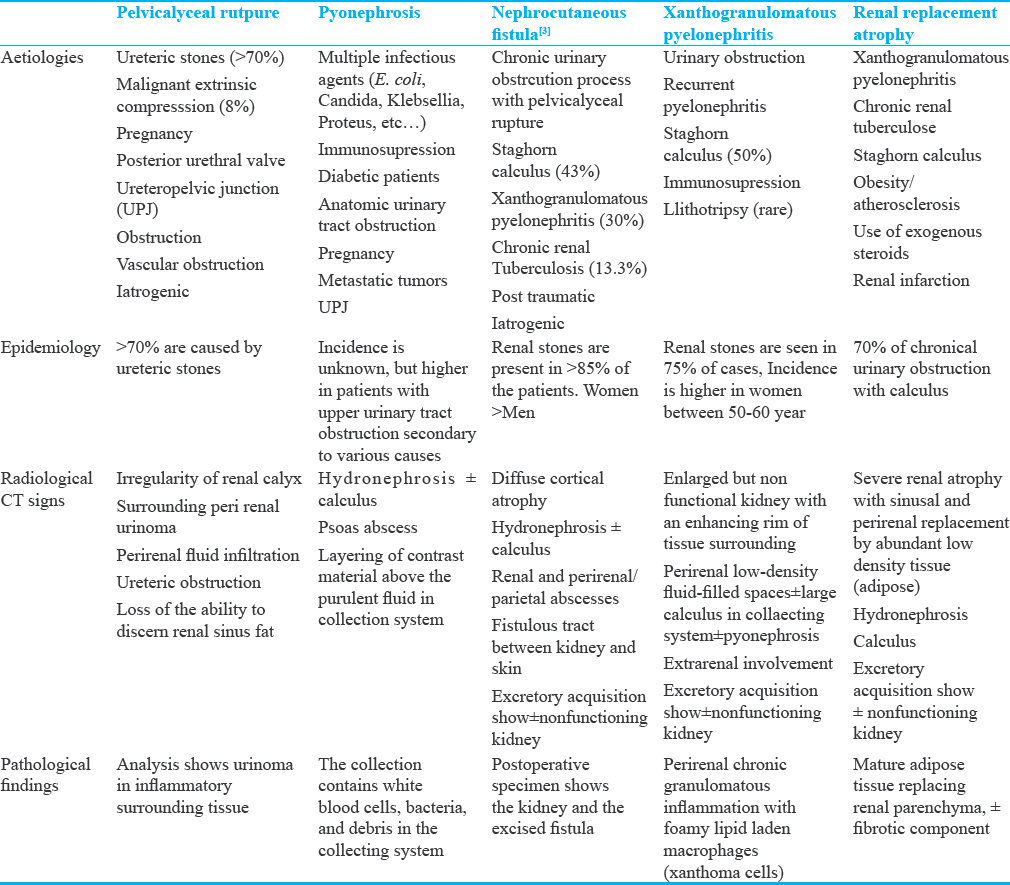
Rare complications of chronic urolithiasis include pelvicalyceal rupture,[2] pyonephrosis,[3] nephrocutaneous fistula (NCF),[456] xanthogranulomatosis pyelonephritis,[789] and renal replacement lipomatosis;[10] their characteristics are summarized in Table 1.
NFC is a rare complication of renal stone disease, clinically characterized by flank sinus discharging material, with generally normal blood analyses. Other rarer fistulae have been described, for example, a fistula between the kidney and adjacent organs (pleura, colon, or lungs).[6] Asymptomatic spontaneous NCF in renal stone disease is relative common (63%)[5] and only 30% complained of loin pain, but the reason is still unknown. Usually, fistulae development after renal pelvicalyceal rupture relieves pain and diminishes the tensile stress in the collecting system. Therefore, fistulae always take the shorter path, generally throught the superior or inferior lumbar triangle.[46]
The beginning of obstructive uropathy is disability of urine to flow forward, which causes accumulation and distension of the urinary tract by increased wall pressure. Many symptoms could be seen in intrinsic urinary tract obstruction as colic flank pain. This symptom reflects a vicious circle caused by increasing intraluminal pressure, responsible of contractions of smooth muscle cells, which accentuate the ureteral wall pressure. As the obstruction persists, smooth muscle cells continue to contract, with less force and ureteral wall dilatation appears. Superimposed urinary infection associated to the progressive loss of muscle tone exacerbate the dilatation with no further consequence in wall pressure.[11]
Rubilotta et al.,[5] reported that fistulae develop in the setting of renal stones in approximately 43.3%, staghorn calculi in 43.3%, xanthogranulomatosis pyelonephritis in 30%, and chronic renal tuberculosis in 13.3%.[12] E. coli is a potential causing germ leading to a NCF, but infections are quietly rare. In the case report of Rubilotta, 0.07% of patients had positive culture with E. coli. Immunosuppressed and diabetic patients are more likely to develop renal or perirenal abscess.[6]
In case of NFC, ultrasonography may be the first choice of radiologic modality obtained as it is widely available, but contrast-enhanced uro-CT is necessary to confirm the diagnosis and investigate more precisely the urinary tract.
The best CT protocol used to analyze urinary tract, particularly urinoma and calyceal rupture, is the uro-CT protocol. This imaging modality helps make the differential diagnosis of acute abdomen, allows to obtain more information about the location and the size of the urinoma, and it is more reproducible and reliable for the follow-up. In our institution, we three acquisitions after administration of furosemide in the absence of contraindications. The first one is a native acquisition to see the spontaneous dense calculus. The second is proceeded at arterial time (30 s after administration of 2/3 of contrast medium) to appreciate the tissue enhancement. The last is a mixed acquisition after administration of 1/3 of contrast medium, which combined the nephrographic and excretory phases in one time. Of course, integration of imaging and clinical finding, along with blood tests, allows a greater diagnostic precision.[3]
Most cases of NFC (90%) are associated with chronically obstructed nonfunctioning kidneys, which can be demonstrated with renal scintigraphy using 99 mTc-DMSA, a technique which permits evaluation of renal function and localization of scarring or nonfunctional parenchyma.[13] Urinary obstruction from a ureteral stone could result at the chronic stage in hydroureteronephrosis. If the obstruction persists, chronic renal failure secondary to renal atrophy and parenchymal scarring develop, resulting in a nonfunctioning kidney.
The therapeutic approach depends on the patient's underlying medical comorbidities, on the remaining renal function in the obstructed kidney and the cause of NCF. The first-line treatment consists of targeted antibiotic therapy followed by endourological procedures but are habitually insufficient in advanced disease. These procedures consist in temporary percutaneous nephrostomy with fulguration of the fistulous tract, double-J stent, or the endoscopic removal of the obstructing calculus. Indeed, the main treatment for spontaneous NCF is the surgical approach in 90% of patients.[5] Partial nephrectomy is proceeded when the renal function is preserved and total nephrectomy is selected when the renal function is poor or absent. The fistulous tract is always excised in the same operating time, to avoid recurrence and diminish the morbidity.[4]
Xanthogranulomatosis pyelonephritis[789] is an uncommon chronic granulomatous inflammation with parenchymal destruction replaced by macrophages with lipoic content (xanthoma cells). The absence of the latter findings at pathological examination in the current case excludes the diagnosis of xanthogranulomatosis pyelonephritis [Table 1]. It is important to recognize that stone disease can coexist with renal replacement lipomatosis.
Pelvicalyceal rupture occurs when the pressure in the collecting system from an obstructing process results in extravasation of urine through the path of least resistance in the renal parenchyma. Most calyceal ruptures are caused by proximal ureteral stones (74%) followed by malignant extrinsic compression (8%).[2] Radiological images show perirenal urinoma associated with ureteral obstruction [Table 1].
Renal replacement lipomatosis is sometimes encountered in chronic urinary obstruction and represents the extreme form of renal sinus lipomatosis, usually occurring unilaterally.[13] This benign condition is characterized by the replacement of normal renal parenchymal tissue by the proliferation of sinus and perirenal fatty tissue, secondary to severe renal atrophy.[14] Renal replacement lipomatosis is seen in 70% of cases with renal calculus, less frequently renal tuberculosis, and occasionally after renal infarction,[1516] associated with hydronephrosis and inflammation. The differential diagnosis for renal replacement lipomatosis is fatty renal masses (liposarcoma, lipoma, angiomyolipoma), transitional carcinoma of the renal sinus, and xanthogranulomatosis pyelonephritis.
Many complications can be seen secondary to chronic obstructive uropathy including NFC secondary to a calyceal rupture, xanthogranulomatosis pyelonephritis, or a chronic renal tuberculosis.
This case illustrates that a ureteral stone responsible of calyceal rupture and resultant NFC can remain asymptomatic during the subacute and chronic phases and eventually results in a chronic nonfunctioning kidney. Ultrasonography and contrast-enhanced CT with uro-CT protocol, generally available in emergencies section, help establish the diagnosis along with blood tests and clinical examination. Renal scintigraphy with 99 mTc-DMSA determines the remaining functioning renal tissue and guides further treatment decisions between surgical or noninvasive treatment. If the NFC causes renal impaired function, a complete nephrectomy with excision of the fistulous tract is performed because of the risk of recurrence or morbidity. A preserved renal function permits a partial nephrectomy or endourological procedures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2017/7/1/9/200573
References
- Fundamentals of Diagnostic Radiology: Fourth Volume Set (4th ed). Philadelphia: LWW; 2012.
- Nephrocutaneous fistula as the initial manifestation of asymptomatic nephrolithiasis: A call for radical management. Urol Ann. 2015;7:94-6.
- [Google Scholar]
- Spontaneous nephrocutaneous fistula: A case report, update of the literature and management algorithm. Urol Int. 2016;97:241-6.
- [Google Scholar]
- Xanthogranulomatous pyelonephritis with a nephrocutaneous fistula. J Emerg Med. 2005;29:337-8.
- [Google Scholar]
- Xanthogranulomatous pyelonephritis with spontaneous nephrocutaneous fistula. Korean J Urol. 2008;49:1158-60.
- [Google Scholar]
- Xanthogranulomatous pyelonephritis: A retrospective review of 16 cases. Korean J Urol. 2011;52:421-4.
- [Google Scholar]
- Bienvenu JM, Urinary Tract Obstruction Treatment and Management, 14 November 2014
- Spontaneous nephrocutaneous fistula in tuberculous pyelonephritis. J Coll Physicians Surg Pak. 2007;17:367-8.
- [Google Scholar]
- The renal sinus: Pathologic spectrum and multimodality imaging approach. Radiographics. 2004;24(Suppl 1):S117-31.
- [Google Scholar]
- Dimercaptosuccinic acid renal scintigraphy for the evaluation of pyelonephritis and scarring: A review of experimental and clinical studies. J Urol. 1992;148(5 Pt 2):1726-32.
- [Google Scholar]
- Idiopathic renal replacement lipomatosis: A case report and review of literature. Indian J Pathol Microbiol. 2009;52:552-3.
- [Google Scholar]
- Renal replacement lipomatosis: A rare type of renal pseudotumor. Indian J Nephrol. 2010;20:92-3.
- [Google Scholar]






