Translate this page into:
Infantile Hemangioendothelioma of the Parotid Gland
Address for correspondence: Dr. Rajas Chaubal, Department of Radiology, Dr. D.Y. Patil Medical College, Navi Mumbai, Maharashtra, India. E-mail: rajas.chaubal@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A 4-month-old infant presented with a painless swelling overlying the left angle of mandible. Ultrasound and magnetic resonance imaging (MRI) revealed a large lesion replacing the entire left parotid gland, with multiple enlarged vessels. Homogeneous enhancement of the lesion was seen on the postcontrast MRI scans. Based on the imaging features, a diagnosis of infantile hemangioendothelioma of the parotid gland was offered. This helped in avoiding any further invasive testing.
Keywords
Infantile hemangioendothelioma
magnetic resonance imaging
parotid tumor
pediatric
ultrasound

Introduction
Hemangioendothelioma (HAE) is a rare tumor. However, it is the most common parotid gland tumor in children. It presents as a painless, rapidly progressive swelling in infancy. The lesion is benign and self-limiting, and hence, proper diagnosis of the lesion is required to prevent unnecessary invasive testing.
Case Report
A 4-month-old infant presented with a painless swelling overlying the left angle of the mandible [Figure 1]. The swelling was soft and nontender on palpation, with normal appearance of the overlying skin.

- A 4-month-old infant with a history of soft-tissue swelling overlying the left angle of mandible (white arrow).
Ultrasound (USG) of the parotid swelling was performed using a linear 4–7 MHz transducer. USG examination revealed a largely homogeneous, isoechoic lesion replacing the entire parotid gland. The lesion had lobulated margins. The normal parotid gland parenchyma was not visualized. A few echogenic internal septae were seen within the parotid mass lesion [Figures 2 and 3]. Color flow Doppler examination revealed the presence of multiple, dilated vascular channels [Figure 4].

- A 4-month-old infant with a history of soft-tissue swelling overlying the left angle of the mandible. Ultrasound image of the left parotid gland shows a large isoechoic lesion (white arrow) with echogenic septae within the gland (white arrowhead).
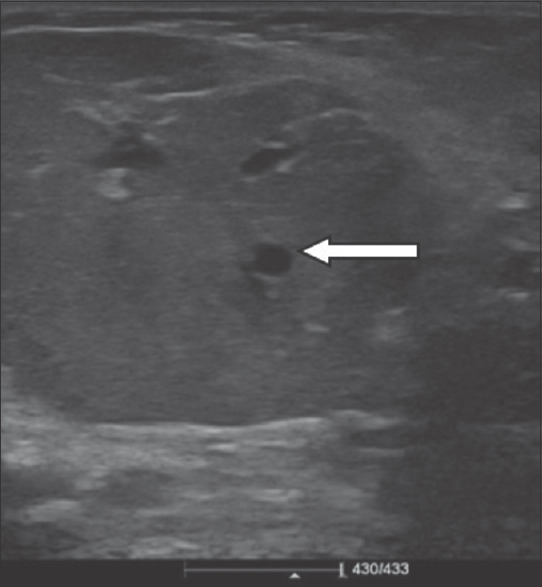
- A 4-month-old infant with a history of soft-tissue swelling overlying the left angle of the mandible. Ultrasound image of the left parotid gland shows an isoechoic lesion in the parotid gland with prominent vessels within (white arrow).
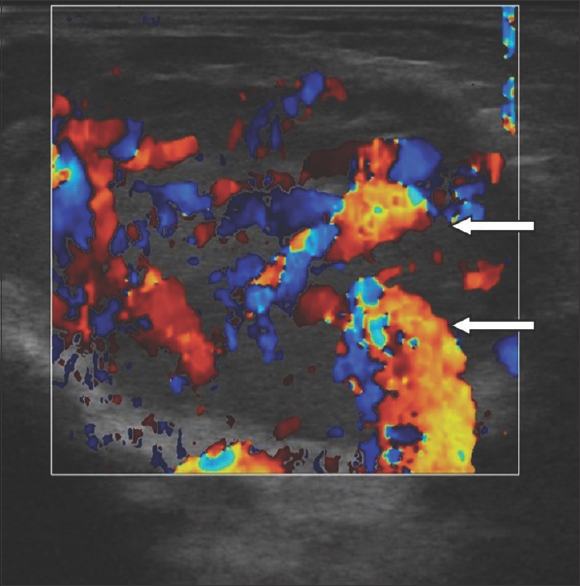
- A 4-month-old infant with a history of soft-tissue swelling overlying the left angle of the mandible. Color Doppler of the left parotid gland shows multiple dilated vascular channels within the lesion (white arrows).
Magnetic resonance imaging (MRI) of the parotid lesion was subsequently performed with a 1.5-T MRI machine using head coils. Axial and coronal T1-weighted, fat-suppressed T2-weighted, coronal short tau inversion recovery (STIR) as well as gadolinium-enhanced T1-weighted axial images were obtained.
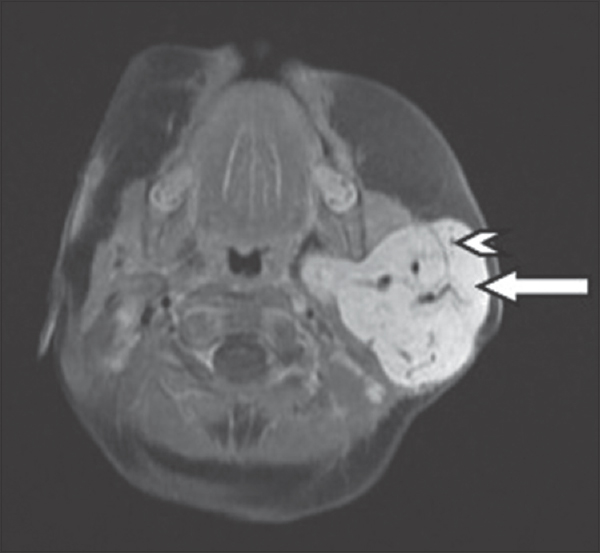
Axial T2-weighted, fat-suppressed [Figure 5] and coronal STIR MRI images [Figure 6] demonstrated a hyperintense lesion involving the left parotid gland. Multiple thin septae were seen within the parotid lesion. Prominent flow voids were also noted within the lesion [Figure 7]. The lesion had a homogeneous enhancement on the postcontrast scan [Figures 8 and 9]. The right parotid gland appeared unremarkable. The overlying skin appeared normal.
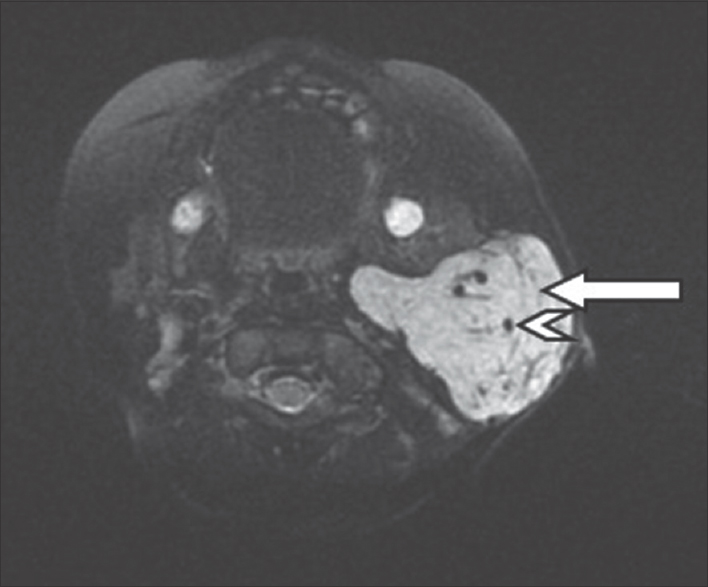
- A 4-month-old infant with a history of soft-tissue swelling overlying the left angle of the mandible. Axial fat-suppressed, T2-weighted magnetic resonance imaging image of the left parotid gland shows a hyperintense lesion in the left parotid gland with few thin septae (white arrows) and flow voids within (white arrowheads).

- A 4-month-old infant with a history of soft-tissue swelling overlying the left angle of the mandible. Coronal short tau inversion recovery magnetic resonance imaging image of the left parotid gland shows a hyperintense lesion in the left parotid gland with few thin septae (white arrows) and flow voids within (white arrowheads).
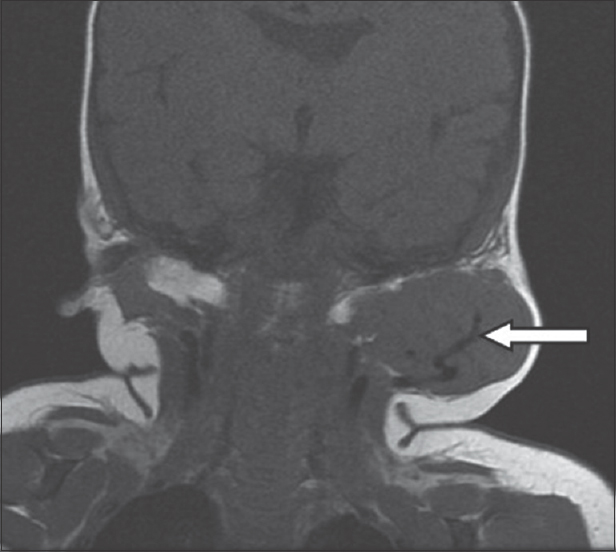
- A 4-month-old infant with a history of soft-tissue swelling overlying the left angle of the mandible. Coronal T1-weighted magnetic resonance imaging image of the left parotid gland shows an isointense lesion in the left parotid gland with a flow void within (white arrow).
- A 4-month-old infant with a history of soft-tissue swelling overlying the left angle of mandible. Contrast-enhanced T1-weighted axial magnetic resonance imaging images of the left parotid gland demonstrates homogeneous enhancement of the entire lesion (white arrows), with thin nonenhancing septae (white arrowheads).
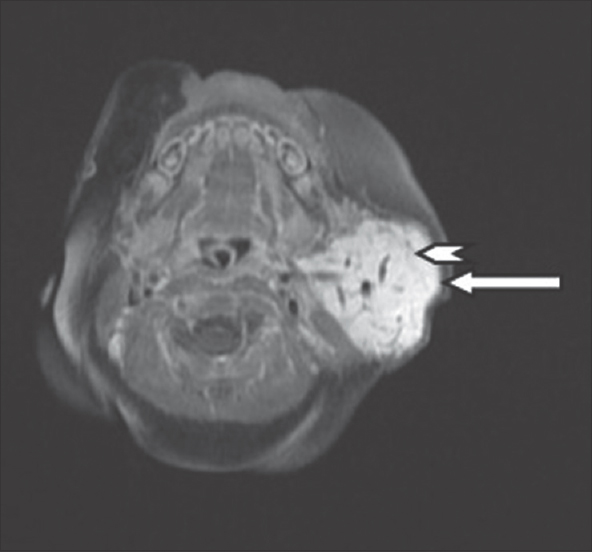
- A 4-month-old infant with a history of soft-tissue swelling overlying the left angle of mandible. Another contrast-enhanced T1-weighted axial magnetic resonance imaging images of the left parotid gland demonstrates homogeneous enhancement of the entire lesion (white arrows), with thin nonenhancing septae (white arrowheads).
Discussion
HAE is the most common parotid tumor in children. The median age of presentation is approximately 4 months. Girls are more commonly affected than boys (3:1).[12] HAE are often multiple. HAE shows rapid enlargement in infancy and gradual regression starting at 8–18 months of age.[3]
The USG findings in our case were consistent with previously described case reports, showing inhomogeneous enlargement of the parotid gland, with retention of its overall shape and preservation of the lobular pattern.[34] The presence of multiple large vessels within the lesion is the characteristic of HAE.[34] Significant extension beyond the parotid gland is uncommon.[4] HAE is known to occur in accessory parotid glands as well.
On MRI, HAE appears isointense to muscle on T1-weighted images and hyperintense on T2-weighted images.[5] It shows homogeneous contrast enhancement with the presence of characteristic prominent flow voids.[4] MRI is a better modality for evaluating the deep lobe of the parotid gland.
Computed tomography (CT) scan provides no significant advantage over MRI and thus can be avoided in view of the radiation dose received by the patient.
Red cell scintigraphy is considered highly accurate in the diagnosis of head and neck hemangiomas in children.[4] It shows the presence of a uniform, well-circumscribed uptake, similar to that in the heart.
Differential diagnoses of HAE in the parotid gland include the following:
-
Congenital infantile fibrosarcoma – In this lesion, color flow Doppler pattern may be similar; however, mass appears inhomogeneous[6]
-
Solitary infantile myofibromatosis – This lesion may show rapid growth followed by involution. However, infantile myofibromatosis is hypovascular, with poorly circumscribed margins[7]
-
Sialoblastoma – On MRI, sialoblastoma shows inhomogeneous signal on T2-weighted images and inhomogeneous contrast enhancement. No flow voids are demonstrated within the tumor.[8]
Surgical resection is not recommended because of the risk of damage to the facial nerve and favorable prognosis with expectant management.[1] Treatment with oral corticosteroids or interferon α2a may be carried out when rare systemic complications such as cardiac failure or Kasabach–Merritt syndrome are present. However, parotid hemangiomas do not respond well to this therapy.[4]
Conclusion
Thus, it is important to identify this lesion on radiological studies so as to avoid any unnecessary biopsies/fine needle aspiration cytologies. Recent studies have indicated that USG with high-frequency transducer alone can also be adequate in the diagnosis of HAEs in the presence of an appropriate clinical setting.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2017/7/1/5/199056.
References
- Histopathologic review of salivary gland tumors in childhood. Arch Otolaryngol Head Neck Surg. 1988;114:898-906.
- [Google Scholar]
- Histopathologic studies of benign infantile hemangioendothelioma of the parotid gland. Cancer. 1980;46:2250-6.
- [Google Scholar]
- Hemangioma of the parotid gland in an infant: MR and Doppler US findings. Eurasian J Med. 2009;41:141.
- [Google Scholar]
- Hemangioendothelioma of the parotid gland in infants: Sonography and correlative MR imaging. AJNR Am J Neuroradiol. 2000;21:219-23.
- [Google Scholar]
- Parotid haemangioma in infants: MR imaging at 1.5 T. Pediatr Radiol. 1991;21:483-5.
- [Google Scholar]
- Congenital fibrosarcoma masquerading as congenital hemangioma: Report of two cases. J Pediatr Surg. 1995;30:1378-81.
- [Google Scholar]
- Soft-tissue hemangiomas in infants and children: Diagnosis using Doppler sonography. AJR Am J Roentgenol. 1998;171:247-52.
- [Google Scholar]
- Sialoblastoma (embryoma): MR findings of a rare pediatric salivary gland tumor. AJNR Am J Neuroradiol. 1997;18:847-50.
- [Google Scholar]






