Translate this page into:
Assessing the Performance of Imaging Health Systems in Five Selected Hospitals in Uganda
Address for correspondence: Dr. Michael G. Kawooya, ECUREI, c/o Mengo Hospital, Albert Cook Road, Albert Cook Building, P.O. BOX 7161, Kampala, Uganda kawooyagm@yahoo.co.uk
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives:
The first objective of the study was to develop an index termed as the ‘Imaging Coverage’ (IC), for measuring the performance of the imaging health systems. This index together with the Hospital-Based Utilization (HBU) would then be calculated for five Ugandan hospitals. Second, was to relate the financial resources and existing health policy to the performance of the imaging systems.
Materials and Methods:
This was a cross-sectional survey employing the triangulation methodology, conducted in Mulago National Referral Hospital. The qualitative study used cluster sampling, in-depth interviews, focus group discussions, and self-administered questionnaires to explore the non-measurable aspects of the imaging systems’ performances.
Results:
The IC developed and tested as an index for the imaging system′s performance was 36%. General X-rays had the best IC followed by ultrasound. The Hospital-Based Utilization for the five selected hospitals was 186 per thousand and was the highest for general radiography followed by ultrasound.
Conclusion:
The IC for the five selected hospitals was 36% and the HBU was 186 per thousand, reflecting low performance levels, largely attributable to inadequate funding. There were shortfalls in imaging requisitions and inefficiencies in the imaging systems, financing, and health policy. Although the proportion of inappropriate imaging was small, reducing this inappropriateness even further would lead to a significant total saving, which could be channeled into investigating more patients. Financial resources stood out as the major limitation in attaining the desired performance and there is a need to increase budget funding so as to improve the performance of the imaging health systems.
Keywords
Imaging health systems
performance
utilization
INTRODUCTION

Uganda has 102 hospitals ranging from tertiary to general.[1] There is a National Health Equipment Policy spelling out types of equipment for all health levels.[2] Performance of the imaging health systems (IHS) is a measure of how the hospitals handle the imaging demands, and is dependent on the resources, institutional processes, and the relevant policies.
Apart from the shortage of human resources, the IHS is bedevilled by infrastructural and budgetary limitations.[34] The ceiling imposed on the National Health Budget has resulted in only 30% of the budget being funded.[56] The ceiling is in order to maintain macroeconomic stability.[78] The budget estimate for imaging for the years 2000 - 2005 had been based on a possibly underestimated and non-evidence based assumption of imaging utilization levels of 20% and 5% for inpatients and outpatients, respectively.[5]
Performance indicators are important for inculcating the best practices and are linked to improved patient outcomes in healthcare, monitoring organizational health, and tracking progress toward institutional goals. Radiology-specific key performance indicators have been grouped as: Operations management, financial management, patient safety, and quality of care – those relating to external and internal stake holders.[9]
Varying departmental performance indicators have been suggested for evaluating organization, volume and productivity, radiology reporting, customer satisfaction, and finance, among others. A study carried out in the USA showed that many academic Radiology Departments do not use indicators and there is no agreement as to which indicators to use. The most commonly used indicators aim at monitoring productivity, especially through measurement of examination volumes. Those departments that measure productivity couple this with the financial indicators. It has, however, also been noted that the results of the measured indicators are often not communicated to the stakeholders, and even when communicated, are not always bench marked.[910]
Operational definitions of the imaging health system performance
Imaging coverage
This is the proportion of the imaging load addressed by the available imaging resources. The denominator is the number per 1000 hospital patients who deserve imaging (IB) and the numerator is the number per 1000 hospital-registered patients per year, who get the imaging investigations done. The imaging coverage numerator refers only to appropriate imaging.
Hospital-based utilization
This is the proportion per thousand hospital patients, who have undergone imaging investigations.
OBJECTIVES
The main objective was to develop an index (IC), for measuring the performance of imaging health systems and to pilot and measure the IC and hospital-based utilization (HBU) for the five hospitals. Second was to relate the financial resources and existing health policy to the performance of the imaging systems.
MATERIALS AND METHODS
Study design
This was a cross-sectional survey with triangulation. Triangulation was defined as combining two or more theories, data sources, methods or investigations when studying one phenomenon.[11–16] It was used because of its ability to improve the validity of the results, as errors that would result from the use of a single method were counteracted. Findings arising from such holistic triangulation studies could be used to generate interventions that were faithful to their qualitative and quantitative origins.
For the quantitative part of the study, cluster sampling was applied. A cluster was defined as one or more mutually exclusive groups within a sample. The grouping was based on geographical or administrative structures.[17]
The clusters were Obstetrics and Gynecology (OBS / GYN), Surgery, Internal Medicine, and Pediatrics. The qualitative part employed purposive sampling.
Study areas
Five health units were selected for inclusion, namely:
-
One government National Referral (tertiary level) hospital - Mulago Hospital.
-
Two government Regional Referral (secondary level) hospitals - Kabale and Mbale Hospitals.
-
Two government General (primary level) hospitals - Rakai and Masindi Hospitals.
The selection of these hospitals was to allow hierarchical and geographical representation, and thereby, improve both internal validity and generalizability.
Mulago Hospital, the main National Tertiary referral hospital, located in the capital city, Kampala, has a bed capacity of 2000. The outpatients’ visits per month are 60,000. There are four general Outpatient Clinics, including Surgery, Internal Medicine, Gynecology, and Pediatrics. There are up to 15 specialized Outpatient Clinics, which include among others, Neurosurgery, Orthopedics, and Chest. The imaging facilities include: Computed Tomography (CT), mammography, fluoroscopy, general-purpose X-ray machines, and a gamma camera. The Radiology Department is manned by 15 radiologists.
The Kabale Hospital is a regional referral hospital located 300 km west of Kampala city. It has a bed capacity of 250, and the outpatient monthly visits total up to 6000. The hospital has several clinical specialists and one radiologist. The imaging equipment available is general radiography and ultrasound.
The Mbale Hospital is a regional referral hospital located 200 km east of Kampala city. It has a bed capacity of 500, and outpatient monthly visits total up to 10,000. The hospital has several specialists and a radiologist. The imaging equipment includes ultrasound and general radiography.
Rakai hospital is a sub-district hospital. It is located 150 km south west of Kampala city. It has a bed capacity of 150, and outpatient monthly visits total up to 1500. The hospital does not have specialists and has no radiologist. The imaging facility used is general radiography.
Masindi Hospital is a general (district) hospital. It is located 200 km north west of Kampala city. It has a bed capacity of 150, and outpatient monthly visits total up to 1500. The hospital does not have specialists and has no radiologist. The imaging equipment available is general radiography.
Sample size and sampling procedure for the quantitative component of the study
The sample size was estimated using the formula by Kish and Leslie. Cluster sampling was employed and a design effect E applied, with E=1 and sample size of 384, for smaller hospitals, and E=2 and a sample size of 786 for regional and tertiary hospitals.
The systematic sampling procedure was applied. Systematic sampling is a method of sampling by which the Nth unit from a study population is selected as the sample, starting with a randomly selected sample unit N.[18]
The period of data collection was fixed at three months, due to logistical limitations.
Methods of data collection for the quantitative component of the study
Relevant information was extracted from the patients’ case notes. A group of three peer raters, excluding the principal investigator (PI), rated each patient’s case information, to assess whether the imaging would have been appropriate. Each case note was initially rated by two raters. Rating was independent and each rater was blinded to the score of the other raters. The rating was based on a set of criteria, previously agreed upon and designed by the raters, together with the PI, for the purpose of this study. The predetermined criteria drew from the American College of Radiologists (ACR) and Royal College of Radiologists RCR other local conditions like tropical diseases, malaria, malnutrition, and bilharzias, which are not addressed by these criteria.[1920]
If the two raters agreed, there was no need for a third rater, but if they disagreed, then the third rater came in as a tie breaker. Raters 1 and 2 agreed in 30.5% of the cases and rater 3 had to be brought in as a tie in 69.5% of the cases.
This information was used to calculate the number per 1000 hospital patients who needed imaging, also referred to as the Imaging Burden (IB); the case notes were also studied, to ascertain which of these patients, who needed to be imaged, had actually obtained the imaging examination. The proportion of those who needed to be imaged and had their imaging done, termed as the Imaging Coverage (IC), was then calculated, with the IB as the denominator and the patients who actually did receive the imaging as the numerator.
Data collection for the qualitative component of the study
This was to explore the non-measurable aspects of the imaging health system's performance.
Twenty-two in-depth interviews (IDI), four focus group discussions (FGDs), and 42 self-administered questionnaires (SAQ) were employed. These were administered to clinicians and radiologists.
Focus group discussions, IDIs, participant observation, and self-administered questionnaires (SAQ) were the qualitative methods of data collection.
There were four FGDs, corresponding to each cluster. Each FGD had a minimum of six members (excluding the moderator and recorder). These six participants were four specialists from that discipline cluster and two radiologists. The reason for including radiologists and clinicians in the FGD was to create a forum similar to a real-life situation, where radiologists and clinicians consult each other for decision-making, regarding difficult clinical cases. The interdisciplinary meeting created a healthy brainstorming atmosphere for an exhaustive discussion of issues. There was also a spillover, whereby both teams appreciated each other′s roles and obligations. Participant observation was applied to the study with the aim of the researcher striving to see things from the perspective of the participants. It is this that made sense of the researcher's stated intention, to observe the behavior and respondents' attitudes as they replied to the questions.
There were 22 respondents for the IDI and these were senior clinicians from each of the four clusters. Sampling stopped because a saturation point had been reached and information redundancy had started to occur. Junior and radiologist doctors filled in a total of 42 SAQs.
Sources of bias in the calculation of efficiency indices
The possible causes of bias in this study were two, namely: Inability to accurately define the outcome variable (appropriate and non-appropriate requisitions) and an inability to get a gold test or gold standard for appropriateness. As a solution, a criterion for appropriateness was developed and applied. Using two raters to agree on appropriateness, helped to overcome subjectivity by just one observer and where the two disagreed, a third rater was brought in as a tie-breaker.
Ethical clearance
Ethical clearance was obtained from the Uganda National Council for Science and Technology.
RESULTS
Imaging coverage
The overall IC for the five hospitals was 36%. The coverage was highest for the Mulago Tertiary Hospital, 56%, followed by Mbale Regional Hospital, 27%, and Masindi District Hospital 19%. The Kabale Regional Hospital and Rakai District Hospital had the lowest coverage at 13 and 10%, respectively.
Among the clusters, the IC was highest for the pediatric cluster (38%) followed by the internal medicine cluster (34%). The surgery cluster and the OBS/GYNAE cluster had lower coverage, 24% and 21% respectively [Figure 1].
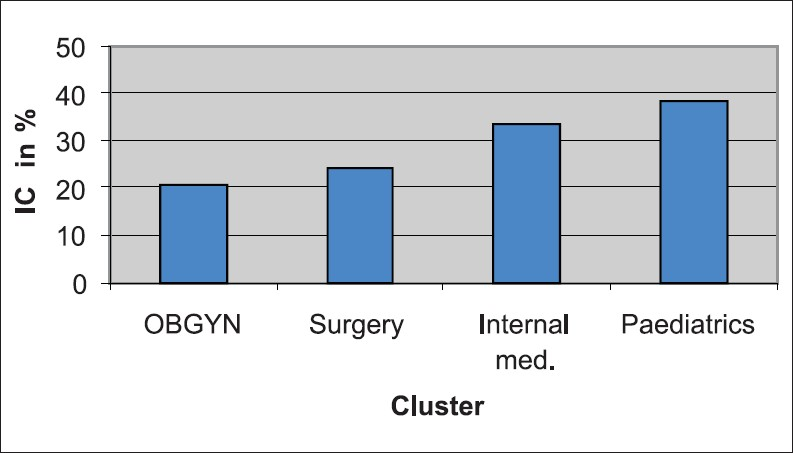
- IC within clusters
With regard to IC for types of examinations, general X-rays had the best IC (36%) followed by ultrasound (29%), computed tomography/magnetic resonance imaging/nuclear medicine (CT/MRI/NI) (18%), and X-ray contrast studies (7%).
Hospital-based utilization
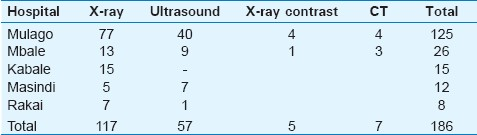
There were a total of 1111 inpatients from all the five hospitals, making up 57% of the total sample size of 1961 patients. Out of these inpatients, 207 received imaging giving a hospital-based utilization of 186 per thousand inpatients. The relative contribution by each imaging modality was 63.0%, 31.0%, 3.8%, and 2.7% for general X-ray, ultrasound, CT, and contrast X-ray studies, respectively. The different HBUs for each hospital, broken down per modality, are shown in Table 1.
Results of the qualitative component of the study
Imaging requisitioning
Flaws in the IHS leading to problems in imaging requisitioning were categorized as: Inadequate supervision of junior doctors during requisition writing, anomalies in the hierarchical chain, work overload for junior doctors, routine requisitioning, patient self-referral, and inadequate interactions between radiologists and clinicians.
Junior doctors were partly blamed for writing poor imaging requisitions, but the junior doctors claimed they were not well supervised. Senior clinicians stated that they were busy with many hospital activities. One commented, “There is a tendency for senior doctors to be rather busy, basically there is inadequate manpower.” One senior clinician saw this extra responsibility for junior doctors not only as a tradition within the health system, but also an opportunity for the juniors to perfect their requisition skills. He stated,“I think it is a tradition we have carried on from when we entered medical practice, but I think it is also an opportunity given to the juniors to learn.”
Anomalies in the hierarchical chain were thought to account for some of the flaws in imaging requisitioning, manifesting as shifting of requisitioning duties to the junior cadre.
Work overload, especially for junior doctors, was also blamed for flaws in requisitioning. One doctor stated, “But I think that the major issue is time; there are too many patients and you are filling in requests for about five other investigations for that same patient!”
The habit of routine requisitioning was said to partly account for requisitioning flaws.
A radiologist, unhappy with the misuse of ultrasound in the Emergency Department, stated: “The doctors do not examine the patients properly; they think ultrasound will show everything, so they just make a requisition.”
Patient self-referral and pressure from patients were cited by some as a possible cause of flaws in requisitioning. One clinician expressed, "Sometimes you get twisted by your patient and you request an investigation just because somebody is insisting."
Commenting on the absence of mutual feedback, one clinician stated, "The radiologists themselves do not give feedback when inadequate information is given, so it has come to be accepted that whatever you write is OK."
It was suggested that these flaws could be rectified by a closer support supervision of the junior doctors, rectifying anomalies in the hierarchical chain, taking more care while requisitioning, educating the patients on the role of imaging in their disease conditions, and a provision for the radiologist to communicate a formal rejection to the referring clinician for those cases in whom the radiologists judged the requisition to be inappropriate”.
Imaging reports
Inefficiencies in the imaging system were thought to lead to delays in reporting, dispatch, and delivery of reports. Some films were delivered to the clinician, unreported.
It was thought that in order to improve performance, there should be prompt delivery of imaging findings to clinicians and the interaction between the radiologist and clinician should be augmented. One clinician commented, “I think we need to improve speed of delivery of results to the units, so that we can quickly make decisions.”
Some clinicians thought that if the images were digital instead of analog, - hard, bulky formats - dispatch, delivery, storage, and retrieval would be easier, more efficient, and faster.
Giving feedback to radiologists as a way of correlating imaging findings, with results from the subsequent procedure, was identified as one way of improving the quality of imaging reports. One clinician highlighted this stating, “We surgeons should give radiologists feedback and interact with them as much as possible; radiologists never get to know what we found at surgery.”
Impact of resources on the performance of imaging health systems
Financial, human resource, and equipment distribution in the five study hospitals
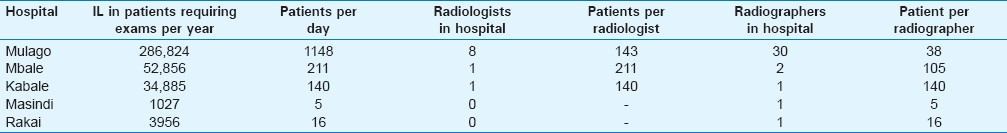
It was noted that the all hospitals received less than 30 % of the required budget. The workforce and the equipment were also limited [Tables 2–4].


Resource limitations related to low imaging health systems performance
The qualitative part of the study revealed resource-related low performance of the HIS manifesting as: Delays in performing some of the imaging investigations or a failure to perform them, as a result of lack of resources and high fees of some of the examinations, rendering them unaffordable to some patients. It was generally thought that the frequent breakdown of machines, with long downtime, further complicated by shortages of consumables, were the deterrents. One radiologist commented, “Of course there may be no films or chemicals, so shortage of materials is a big problem. Quite often the equipment breaks down, so all these cause delays.” Non-requisitioning of potentially beneficial examinations was also partly attributed to inadequate resources.
High costs of some imaging investigations were thought to account for some cases of inappropriate non-requisitioning. Doctors, at times, declined requisitioning for CT scan, even when it would have been appropriate, assuming that the patient might not be able to afford it. Clinicians suggested that if there were any shortages of sundries or machine malfunction, the radiologist should get in touch with them so that they could come up with the next best imaging option.
There was a suggestion that the imaging requisition form should be structured and should have leading questions. Many pointed out that the form should be redesigned by making it larger, to accommodate more information.
Policy standards and guidelines related to performance of imaging health systems
During the qualitative interviews, the participants voiced some contextual factors, which could impact efficiency. In particular, the absence of policy standards and guidelines was cited.
One clinician quoted one doctor as stating, “But if we had clear guidelines it would go a long way in minimizing inappropriate requisitions.” It was thought that guidelines would be a way to reduce unnecessary imaging; one radiologist concluded, “The guidelines will ensure that only those who need imaging are imaged so there will not be so many unnecessary reports to write.” Imaging guidelines were also thought to improve imaging reports. One doctor put it in these words, “Probably there could be developed some schedule or some format of report writing.”
DISCUSSION
Overall imaging coverage and the hospitalbased utilization
The IC of only 36% shows that the imaging system performance with regard to handling the prevailing IB is only 36%. This is an indication of the low response capacity of the system to the demand. The coverage is higher for the Mulago Hospital, which is an urban hospital, in comparison to rural-based hospitals like the Rakai and Masindi. This is thought to be due to limited resources in rural areas. The radiology utilization rates in non-rural health facilities in the US were found to be almost five times those in the rural and this was also thought to be due to fewer resources in rural areas.[21]
The closest indices to the IC are the hospital-based and population-based utilization indices. This HBU for all the five hospitals was 186 per thousand patients [Table 1]. This is less compared to similar values for the USA. In the USA, the non-invasive diagnostic imaging utilization for Medicare patients have been seen in one study to be 4404 per 1000.[22] In Uganda examination to patient ratio stands at 0.165 examinations per patient compared to a case-mixed ratio for the USA of 2.35 examinations per patient.[23] There is no literature on imaging utilization for any other African country.
We sampled only five hospitals out of a total of almost 70 government plus NGO hospitals. We therefore, cannot calculate a nationwide population-based utilization index. However, the hospital-based utilization of 186 per 1000 [Table 1] is much lower than the population-based index of 600 per thousand for Nordic countries and 4176 per 1000 for USA.[24]
For Africa, the population-based utilization levels available in literature were calculated by Cockshott, way back in 1979.[25] These are 13, 18, 29, 22, and 28 per thousand for Senegal, Ghana, Congo, Kenya, and the Ivory Coast, respectively. Cockshott did not include Uganda in his research. These figures from Africa are probably outdated. Nonetheless, they portray a gloomy picture of the services.
Regarding the relative applicability of hospital- and population-based utilization for Uganda, the hospital-based indices are likely to be more applicable, as they are more representative of the utilization status, and are easier to measure. The marked variation in the IC between the various health levels (tertiary, regional, and general) indicates that there is no uniform utilization across the country. Burkahardt and Sunshine, commenting on the population-based utilization indices for the USA have made a similar observation.[26] They concluded that much variability exists in population-based utilization rates, and that the national or regional averages are not a good guide to utilization in specific patient populations. They advocated the use of actual data from patient populations as a better predictor for future utilization trends; even generalization of the hospital-based utilization of 165, for all levels of service delivery, may be realistic, because of variations in the IC among the levels.
With regard to the utilization for specific imaging modalities, the utilization was 117, 57, 7, and 5 per thousand for general X-ray, ultrasound, CT, and contrast X-ray, respectively [Table 1]. These figures are much lower than for the USA, for which the population-based indices per one thousand in 2003 were: 2057, 921, 391, 114, 215, 221, and 249 for general radiography, ultrasound, CT, MRI, interventional radiology, mammography, and nuclear medicine, respectively.[24] In 2008, the utilization per 1000 Medicare patients was 292, 262, 145, 405, and 292 for CT, Nuclear medicine, MRI, echocardiography, and ultrasound, respectively.[22]
The relative contribution by each imaging modality was 63.0, 31.0, 3.8, and 2.7% for general X-ray, ultrasound, CT, and contrast X-ray studies, respectively. This pattern differs from the USA where general radiography takes a significant majority of 55-58%, followed by CT, 11-20%, and ultrasound contributes to only 11%.[27] The differences may be due to patient population characteristics and Uganda′s lower level of technology sophistication.
This article has measured the HBU at one point in time, but for evidence-based policy and planning, it is ideal to record the trend of the HBU over time. This enables the projection of utilization levels for future planning. Uganda is undergoing rapid change in technology acquisition. Kampala city currently has five multi-slice CTs, and two low-field strength MRIs, and a 1.5 Tesla MRI is being purchased for installation next year. As the proportion and number of educated Ugandans rise, due to the recently introduced Universal Primary and Secondary Education, the population is becoming more aware of the capabilities of newer imaging technologies. Uganda's GDP per capita is growing at 6% per anum. It was 1283 US Dollars in 2010.[28]
The observed escalation of imaging utilization in developed countries, is therefore, likely to be played out in Uganda and other developing countries, but to a much lesser, although not an insignificant scale. It is therefore important to borrow a lead from trends in developed countries.
Interest in imaging utilization trends started in the early 1990s, and was most likely prompted by the advent and escalation of utilization and imaging costs, possibly attributed to the sophisticated cross-sectional imaging techniques like CT, MRI, ultrasound, and nuclear medicine, and the continuous and rapid developments in these technologies.
A panoramic view of trends in the USA is given by in an article by Rajas et al. Over a 20-year period from 1990 to 2009, X-ray utilization per 1000 Emergency Department patients fell by 86% in contrast to an increase in utilization of advanced imaging modalities like CT, MRI, and ultrasound. The highest increase was in CT, which increased 17.5-fold, and ultrasound increased by 51.6%. The clinical decision tools and appropriate criteria were recommended by the authors to curb the unnecessary utilization of expensive imaging modalities.[29]
As early as the mid 1980s, the curiosity in utilization trends had already sparked off. Khorsani R et al., in a retrospective study conducted from 1984 to 1993, in Boston, USA, for a 751-bed tertiary hospital, evaluated trends based on utilization per case-mix adjusted admission (CMAA), using linear regression analysis. In general, there was a decrease in the number of studies per CMAA. More specifically the utilization of ultrasound and conventional imaging (plain radiography and fluoroscopy) decreased, whereas, the use of more sophisticated techniques namely CT and MRI rose. Nuclear medicine trends showed no change. They recommended studies to understand the pattern of the usage of CT and MRI, so as to reduce inappropriate usage, and furthermore that the application of expensive imaging techniques should be justified by impact on patient outcomes and reduction in length of hospital admissions.[30]
The 1990s saw a rapid escalation in the utilization of non-invasive diagnostic imaging (NID). Based on information from the Medicare Part B claim files, for the six-year period between 1993 and 1996, there was an overall increased utilization of NID by radiologists and non-radiologist groups. The increase was most marked among non-radiologists in comparison to radiologists, with the proportion of NID performed by radiologists falling from 73.0% in 1993 to 67.4% in 1996.[3132]
In a retrospective study by Matin et al., spanning a period of ten years, (1993-2002), in Boston, USA, there was an overall decrease in number of studies per case-mix adjusted admission (CMAA), from 1.55 to 1.33. More specifically the utilization per CMAA of ultrasound and radiography decreased, whereas, use of more sophisticated techniques like nuclear medicine, CT, and MRI rose. The increase in utilization of the sophisticated imaging techniques was thought to be due to the rapid increase in the clinical use of these techniques, practice pattern, social expectations, and patient complexity. The authors recommended that there should be efforts to reduce inappropriate utilization. Requisitioning should be justified by impact on clinical decision-making and patient outcomes. [23]
Surveys carried out between 2000 and 2005 showed an unabated upward trend for utilization of sophisticated imaging techniques in the US. Mitchel JM et al. evaluated the utilization of highly re-imbursed advanced imaging techniques among privately insured individuals in California and recorded the increase in utilization. The increase in PET was 400%, and in MRI and CT 50%. The increase was most marked in independent diagnostic testing and in physician self-referral arrangement facilities, but less marked in a hospital setting. The author concluded that imaging guidelines could play a role in reducing unnecessary utilization of highly reimbursed advanced imaging techniques, resulting in a considerable potential for saving.[33]
In order to obtain a detailed understanding of the population-based utilization trends for different modalities, regions, and population in the USA, between 1988 and 2001, Bhargavan M et al., studied the aggregate claims data of 25,000 Medicare enrolees. In 2001, the utilization was 4176 per 1000 for diagnostic imaging and 274 per 1000 for interventional procedures. Almost 50% of imaging utilization was due to radiography and the rest due to cross-sectional imaging (CT, MRI, ultrasound, interventional radiology, nuclear medicine, and mammography). Between 1988 and 2001, there had been an increase in utilization, with advanced imaging techniques increasing up to 16% in contrast to radiography, which increased by only 1%. Increase in utilization varied per region and state, with the North-East having the highest increase. States with higher populations, higher number of radiologists, and Medicare services also had higher increases.[34]
The turning point came after 2005, and it was exposed by Levin CD et al., who through analysis of the annual nationwide Medicare Part B databases for the period 2005 to 2008, demonstrated a slowdown of the compounded annual growth (CAGR) rate from 4.8 to 1.4%, between 1988 and 2005. Specifically the slowdown was for fee-for-service, noninvasive diagnostic imaging. The utilization had grown rapidly from 3,190 noninvasive procedures per 1000 climbing steeply to 4,230 in 2005, and then surprisingly less rapidly to 4,404, in 2008. In 2008, the utilization per 1000 Medicare patients was 292, 262, 145, 405, and 292 for CT, Nuclear medicine, MRI, echocardiography, and ultrasound, respectively. The slowdown had been mostly for MRI and nuclear imaging. It abated for CT, ultrasound, and echocardiography as well. The earlier higher growth was thought to be due to a growth in the utilization of sophisticated imaging techniques. Furthermore, the growth in utilization had been shown to be twice by non-radiologists and self-referring physicians (6.6%) as compared to radiologists (3.4%). The recently observed slowdown was believed to be due to reduction in re-imbursement for imaging.[22]
To further illustrate the general trend in increased utilization, the workload for radiologists has shown a steady rise, increasing by 8.5% between 1995-1996 and 1998-1999.[243536]
There have been several attempts to analyze the causes of increased and inappropriate utilization and to recommend solutions. Kessler D and McClellan M pointed at “defensive medicine” as a major driver to escalating medical costs in the management of cardiac disease. They observed that malpractice liability reforms that directly limit awards and benefits from lawsuits lead to a substantial reduction in the escalation of medical costs, with no negative impact on the treatment outcomes.[37] Lysdahl KB and Hofmann BM, in Norway, through interviews of radiologists, found that the major reasons were introduction of newer technologies, demand from patients, the referrers' inability to tolerate what they think is wrong, expanded clinical information, and availability of the technique. They recommended that it was important to instill a measure, which supported the decision process, possibly through guidelines.[38] The type of payment system could have an impact on the utilization rates. Bhurkhardt JH et al., using data from Medicare, Health Management Organizations (HMO), and conventional insurances, demonstrated a great variability in utilization, for patients in different payment systems. Utilization was found to be almost three times more for Medicare enrolees in comparison to HMO.[26] Physician self-referral is thought to be a major contributor to unnecessary imaging utilization. Levin DC et al., reviewed the different measures undertaken to overcome unnecessary utilization of imaging through physician self-referral arrangement.[39]
This study has identified anomalies in the hierarchical chain, routine requisitioning, patient self-referral, pressure from patients, and lack of clinical imaging guidelines, as the major drivers to inappropriate requisitioning and utilization in our health facilities. Defensive medicine is not yet a key factor, but is bound to increase as patients get more enlightened. Increase in the number and distribution of sophisticated technologies, compounded by lack of imaging guidelines for these technologies, may in the future be a major driver to overutilization in our health facilities.
Impact of resources on the efficiency of the imaging system
Less than 30% of the budget for imagimg is funded [Tables 2–4]. Even if the actual budget was 100% realized, it would not cater to the Imaging Burden, because the budgets were based on non-evidence-based 5 - 20% utilization. The shortfall in the budget may explain why there are chronic shortages of consumables and almost half the total number of machines are non-functional at any given time.
The Masindi Hospital has a higher annual expenditure per patient, in comparison to the other four hospitals [Table 2]. The explanation is that the government allocates a uniform annual recurrent fee of 12,000,000.00 shillings per general (district) hospital, per year, but the yearly patient imaging load for Masindi, of 1027 patients, is the lowest, among all the five hospitals. The study found that patients attending the Masindi Hospital had fewer conditions that required imaging, in comparison to the other four hospitals. Therefore, each patient takes a larger share of the total allocation, in comparison to the other hospitals, which have a higher proportion of patients requiring imaging.
The fact that Uganda's national imaging budget is based on a presumptive utilization of 15-20% sets a policy limit for the IC and the utilization levels.[40] This is further worsened by the fact that only 30% of the national health budget is financed.[1] This under-funding is automatically reflected in the IC, which is 36%.
Odaga and Lachoro pointed out that health budget ceiling was the single most important hindrance to health service delivery in Uganda.[8] The ceiling on the budget for MoH was to ensure macro-economic stability. This policy on budget ceiling directly impacts the efficiency of the imaging system, and is most likely the basis for 30% funding of the imaging budget, with a resultant 36% IC. Cockshott also partly attributed the inefficiencies in Africa's imaging services to inadequate budgets.[25]
Only 68% of the established posts for imaging staff are in the city. Posts for radiologists only exist at the tertiary and regional level hospitals, and these hospitals total to only 14. There is an unmanageable workload of 140 to 211 examinations per radiologist, per day. Cockshott observed a shortage of radiologists and radiographers in several African countries and coined the phrase, ‘capital city syndrome’.[25] In the USA, the average annual workload per radiologist is 14,900, examinations.[36] From the figures in this study, the workload for the Ugandan radiologists averages 16,000 examinations per radiologist per year.
Frequent breakdown of equipment and long downtimes were reported at all five hospitals [Table 4]. The supplies of consumables were irregular. Contrast X-rays and CT/MRI had the lowest IC. This could be explained by the frequent breakdowns and / or total absence of these more technically sophisticated imaging modalities. The country does not have enough equipment maintenance and service personnel.
It should be noted that appropriate requisitioning was 94%. Based on the total imaging load of all the five hospitals, which is 379,548 patients [Table 2], and on the fact that 6% of all requisitions were inappropriate, a total of 22,772 examinations were inappropriate. Based on a calculation that takes into consideration the total imaging load of all the five hospitals and the total budget of all these hospitals, which is 340,000,000.00 shillings [Table 2], 895 shillings are budgeted to be spent on each patient. This implies that for the 22,772 inappropriate examinations, 20,385,415.00 shillings were wasted in inappropriate imaging.
Policy standards and guidelines
From the results of the qualitative component of the study, it was the general opinion that imaging guidelines would improve the efficiency.
There are potential benefits when guidelines are applied. Roberts demonstrated a reduction in utilization of preoperative chest X-rays in two UK district general hospitals by 42 and 26%, respectively, following introduction of guidelines, without any harmful effects on postoperative mortality or morbidity.[41] There may be a selective compliance of imaging staff for certain procedures in the guidelines.[42]
CONCLUSION
The IC for the five selected hospitals is 36% and the HBU is 186 per thousand, reflecting low performance levels, largely attributable to inadequate funding. There have been shortfalls in imaging requisitions and imaging reports, related to inefficiencies in the imaging systems, financing, and health policy. Although the proportion of inappropriate imaging is small, reducing this inappropriateness even further, will lead to a significant total saving, which may be channeled into investigating more patients. Financial resources stand out as the major limitation in attaining the desired performance and there is a need to increase budget funding so as to improve the performance of the imaging health systems.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/12/94225
REFERENCES
- Ministry of Health Uganda. Health Sector Strategic Plan II, 2005/06 - 2009/10. Vol 1. Kampala, Ministry of Health: Uganda; 2005.
- [Google Scholar]
- Ministry of Health Uganda. National Health Equipment Policy Document. Vol 1. The Republic of Uganda: Ministry of Health; 2005.
- [Google Scholar]
- The Poverty Eradication Action Plan 2004/05-2007/08. Uganda: Ministry of Finance Planning and Economic Development; 2004.
- [Google Scholar]
- Dying for economic growth? Evidence of a flawed economic policy in Uganda? Lancet. 2004;364:1632-7.
- [Google Scholar]
- Background to the Budget 2005/06. Uganda: Ministry of Finance Planning and Economic Development; 2005.
- [Google Scholar]
- Key performance indicators for measuring and improving radiology department performance. Radiographics. 2010;30:571-83.
- [Google Scholar]
- Practice Management, Performance Indicators, in Academic Radiology Departments. Radiology. 2004;233:716-22.
- [Google Scholar]
- The research art: A theoretical introduction to sociological methods. (3rd ed). Chicago: Aldine; 1989.
- [Google Scholar]
- Triangulation in nursing research: Issues of conceptual clarity and purpose. J Adv Nurs. 1998;28:631-41.
- [Google Scholar]
- Qualitative Vs Quantitative research or qualitative and quantitative research? Nurs Res. 1984;33:378-80.
- [Google Scholar]
- Methodological triangulation in public health research - advancement or mirage? Trop Med Int Health. 1999;4:243-4.
- [Google Scholar]
- Cluster randomised trials in the medical literature: Two bibliometric surveys. BMC Med Res Methodol. 2004;4:21.
- [Google Scholar]
- Royal College of Radiologists Working Party, 1992, Influence of the Royal College of Radiologists′ guidelines on hospital practice: A multicentre study. BMJ. 1992;304:740-3.
- [Google Scholar]
- Radiology Business Management Association. Radiology Business Management Association 2009
- [Google Scholar]
- Bending the Curve: The recent marked slowdown in growth of noninvasive diagnostic imaging. AJR Am J Roentgenol. 2011;196:W25-9.
- [Google Scholar]
- Inpatient Radiology Utilization: Trends over the Past Decade. AJR Am J Roentgenol. 2006;186:7-11.
- [Google Scholar]
- Workload of Radiologists in the United States in 2002-2003 and Trends Since 1991-1992. Radiology. 2005;234:824-32.
- [Google Scholar]
- Diagnostic radiology: Geography of a high technology. AJR Am J Roentgenol. 1979;132:339-44.
- [Google Scholar]
- Utilization of radiologic services in different payment systems and patient populations. Radiology. 1996;200:201-7.
- [Google Scholar]
- Uganda Country Report: GDP data and GDP forecasts; economic, financial and trade information; the best banks in Uganda; country and population overview. Global Finance.
- Abdominal imaging utilization in the emergency department: Trends over two decades. Int J Emerg Med. 2011;4:19.
- [Google Scholar]
- Trends in the use of radiology with inpatients: What has changed in a decade? AJR Am J Roentgenol. 1998;170:859-61.
- [Google Scholar]
- Nationwide trends in rates of utilization of noninvasive diagnostic imaging among the Medicare population between 1993 and 1999. Radiology. 2003;227:113-7.
- [Google Scholar]
- Practice Patterns of Radiologists and Nonradiologists in Utilization of Noninvasive Diagnostic Imaging among the Medicare Population 1993-1999. Radiology. 2003;228:795-801.
- [Google Scholar]
- Utilization trends for advanced imaging procedures: Evidence from individuals with private insurance coverage in California. Med Care. 2008;46:460-6.
- [Google Scholar]
- Utilization of Radiology Services in the United States: Levels and Trends in Modalities, Regions, and Populations. Radiology. 2005;234:824-32.
- [Google Scholar]
- Workload of Radiologists in the United States in 1998-1999 and Trends Since 1995-1996. AJR Am J Roentgenol. 2002;179:1123-8.
- [Google Scholar]
- Workload of Radiologists in United States in 2006-2007 and Trends Since 1991-1992. Radiology. 2011;252:458-67.
- [Google Scholar]
- What causes increasing and unnecessary use of radiological investigations? A survey of radiologists’ perceptions. BMC Health Serv Res. 2009;9:155.
- [Google Scholar]
- Turf wars in radiology: Recent actions against self-referral by state governments, commercial payers, and medicare--hope is on the horizon. J Am Coll Radiol. 2008;5:972-7.
- [Google Scholar]
- Poverty Eradication Action Plan 1997. Uganda: Ministry of Finance and Economic Development; 1997.
- [Google Scholar]
- Toward the effective use of diagnostic radiology in surgical practice: Discussion paper. J Royal Soc Med. 2011;76:755-9.
- [Google Scholar]
- Compliance with guidelines for choice of radiographic projections: A multicentre study. Clin Radiol. 1994;49:537-40.
- [Google Scholar]






