Translate this page into:
Appearances of von Meyenburg Complex on Cross Sectional Imaging
Address for correspondence: Dr. Phillip F.C. Lung, King's College London, Department of Radiology, King's College Hospital, Denmark Hill, London SE5 9RS, UK. E-mail: lung@doctors.org.uk
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The von Meyenburg complex (VMC) is an uncommon congenital malformation and is characterized by benign bile duct hamartomas. These are usually discovered incidentally and may represent a diagnostic dilemma when liver metastases are suspected. MRI of VMC shows distinct imaging characteristics, but reporting of lesional contrast enhancement has been inconsistent, whilst microbubble contrast enhanced ultrasound provides ‘real-time’ evaluation of soft tissue vascularity. Given the diagnostic uncertainty over imaging in VMC, biopsy is often recommended as the definitive diagnosis. We report a biopsy proven case of VMC on a background of primary colonic malignancy investigated with ultrasound, contrast enhanced ultrasound, computed tomography CT, and magnetic resonance imaging MRI, and review the key imaging features.
Keywords
Biliary hamartoma
computed tomography
magnetic resonance imaging
ultrasound contrast
von Meyenburg
INTRODUCTION

The von Meyenburg complex (VMC) was first described in 1918 and is characterized by multiple bile duct hamartomas.[1] These are benign developmental malformations composed of dilated intrahepatic bile ductules embedded in fibrous stroma.[2] The prevalence on autopsy ranges from 0.6 to 2.8%.[2] In clinical practice, the majority are discovered incidentally,[1] but may present a diagnostic dilemma when the patient is undergoing staging imaging for known primary malignancy.
We describe a case of VMC with ultrasound, contrast enhanced ultrasound (CEUS), computed tomography (CT), and magnetic resonance (MR) imaging correlation.
CASE REPORT
An 81-year-old man was admitted with a one-week history of abdominal pain and constipation. On clinical examination, there was abdominal distension and guarding in the right abdomen. Contrast-enhanced CT images (Siemens Sensation 16 slice) were acquired in the portal venous phase (60 s following administration of contrast), demonstrating a focal sigmoid stricture and proximal large bowel obstruction. Multiple low-density lesions of varying sizes were identified within the liver, which were non-enhancing in the portal venous phase [Figure 1]. A sigmoid malignancy was likely, but the majority of liver lesions were near fluid density (3-20HU) and not entirely typical for metastases.
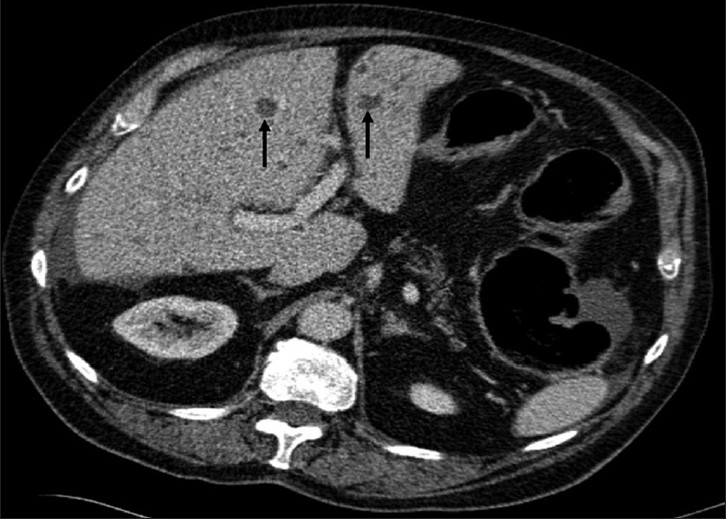
- An 81-year-old man with adenocarcinoma of the colon and hepatic lesions later diagnosed as von Meyenburg complex. Axial enhanced CT image of the abdomen, at the level of the porta, demonstrate multiple fluid density lesions (arrows) of varying sizes within the liver. Fluid surrounding the liver is related to underlying large bowel obstruction.
B-mode ultrasound demonstrated multiple hyperechoic lesions [Figure 2] of varying sizes throughout the liver, none of which displayed signal with color Doppler ultrasound. The hepatic lesions were further interrogated with CEUS, using Sonovue™ (Bracco SpA Milan) as the microbubble contrast agent, on a Siemens S2000 (Siemens AG, Erlangen), with a 4 MHz transducer and imaged using a low mechanical index technique (CPS™, Siemens AG, Erlangen). No appreciable vascularity was seen within the hepatic lesions in all three phases of the study (arterial, early portal venous, and late portal venous phase) with imaging performed for 3 min [Figure 3]. The patient proceeded to laparotomy where a Hartmann's procedure was performed and multiple liver biopsies were obtained.
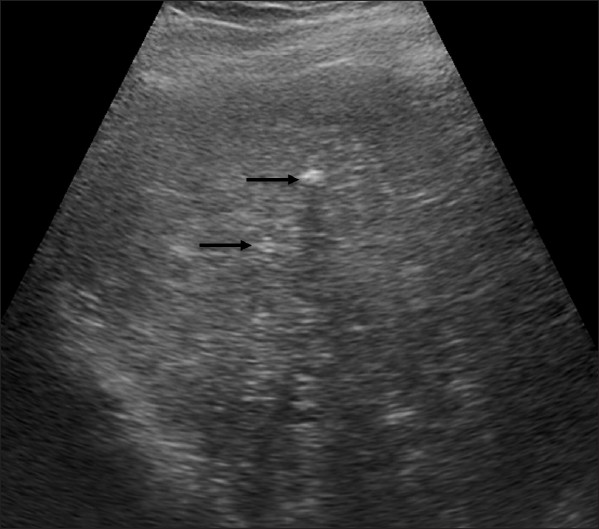
- An 81-year-old man with adenocarcinoma of the colon. Hepatic lesions later diagnosed as von Meyenburg complex. B-mode ultrasound image of the liver shows several hyperechoic focal lesions (arrows).
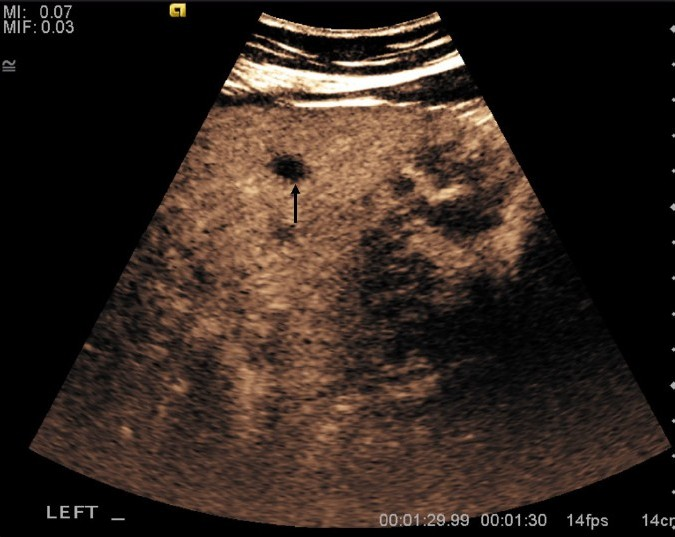
- An 81-year-old man with adenocarcinoma of the colon and hepatic lesions later diagnosed as von Meyenburg complex. Contrast enhanced ultrasound of the liver in the late portal venous phase (1 min 30 sec following injection of contrast) demonstrates non-enhancing lesions (arrow).
Histology of the resected colon confirmed moderately differentiated adenocarcinoma invading through the muscularis propria, but not penetrating the serosal surface. No involvement of the regional lymph nodes was identified. Liver biopsies revealed normal background hepatic parenchyma. Histology of the focal lesions demonstrated expanded portal tracts with dense stroma, containing dilated bile ducts; a few of which contained inspissated bile [Figure 4]. A dilated congested blood vessel within the specimens was presumed to be responsible for the hepatic nodularity. The appearances were in keeping with a diagnosis of VMC.
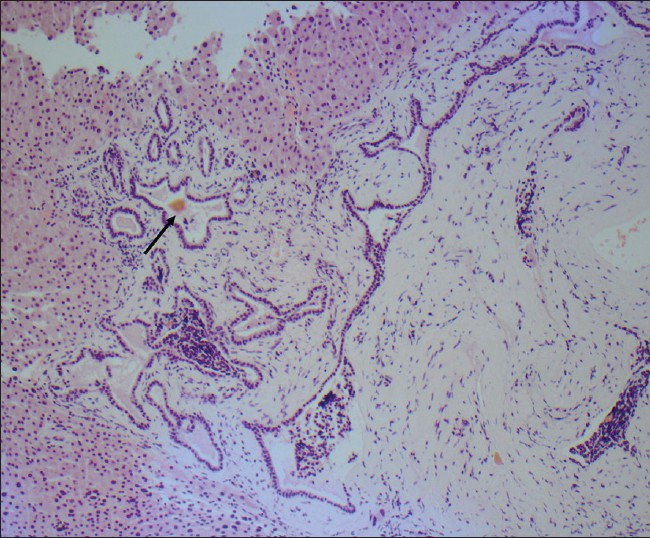
- An 81-year-old man with adenocarcinoma of the colon and hepatic lesions later diagnosed as von Meyenburg complex. Hemotoxylin and eosin stained biopsy specimen shows dilated ducts with inspissated bile (arrow) in an expanded and fibrotic portal tract.
MR imaging was performed to further evaluate the liver and to identify any lesions characteristic of metastases. Multiple hepatic lesions were again visualized and displayed moderate to high T2 (TR: 2410; TE: 103) signal intensity [Figure 5] and T1 hypointensity with no contrast enhancement [Figure 6]. The multiple liver lesions displayed decreasing signal intensity [Figure 7] with increasing b-values on diffusion-weighted imaging, indicating free diffusion. The imaging findings were in keeping with VMC in addition to simple cysts; metastases being less likely.
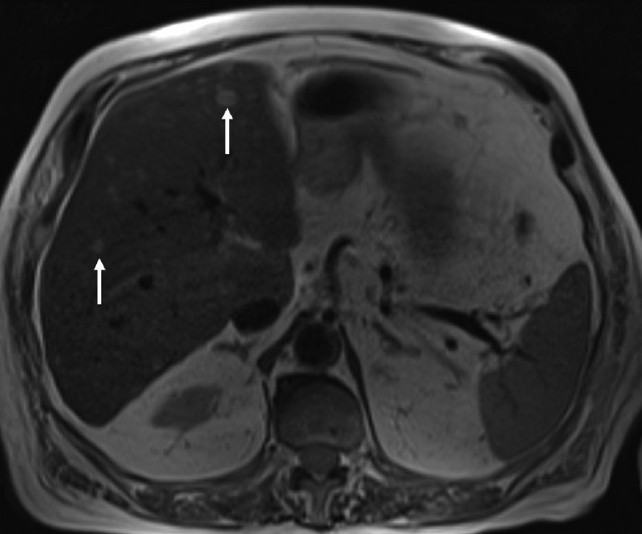
- An 81-year-old man with adenocarcinoma of the colon and hepatic lesions later diagnosed as von Meyenburg complex. In T2-weighted MR sequence of the liver; the focal lesions exhibit high T2 signal (arrows).
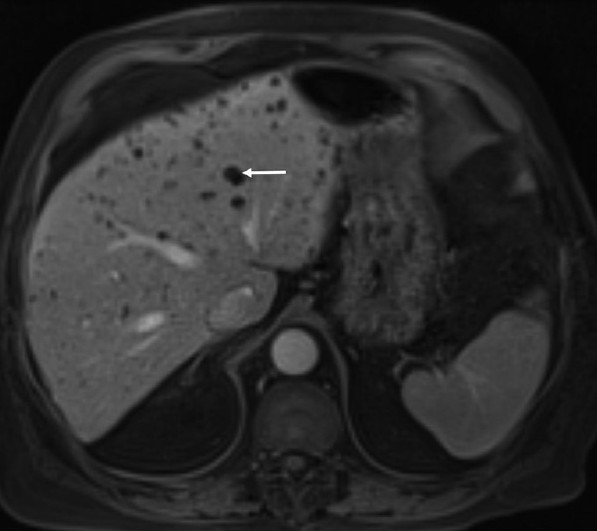
- An 81-year-old man with colon cancer and lesions in the liver diagnosed as von Meyenburg complex. Post-contrast T1-weighted sequence demonstrate multiple non-enhancing lesions (arrow) throughout the liver.
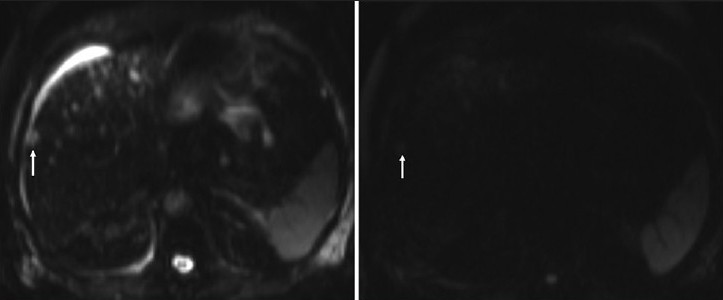
- An 81-year-old man with adenocarcinoma of the colon and hepatic lesions later diagnosed as von Meyenburg complex. Diffusion weighted images of the liver at different b-values reveal negative correlation between the signal intensity of the focal liver lesions (arrow) compared to the b-value, in keeping with free diffusion, which favors benign disease.
The patient had an uncomplicated post-operative course and was discharged. Surveillance imaging 3 years post-surgery demonstrated identical appearances of the liver, with no new abnormalities present and no disease recurrence.
DISCUSSION
von Meyenburg complex (VMC) is an uncommon abnormality and affected patients are usually asymptomatic, although jaundice and portal hypertension may arise as a result of mass effect.[3] The imaging findings of VMC have been documented through case reports and a single case series.[2] The biliary hamartomas of VMC may be single or multiple, ranging in size from 1 to 15 mm; not all lesions are identifiable on imaging[2] and given the small size of the lesions, definitive characterization may be difficult. In the presence of multiple low-density lesions within the liver, differentiation from metastases remains the key clinical question, particularly in the presence of a known primary.
Sonographic appearances of VMC are varied, being described as multiple hypoechoic lesions,[24] hyperechoic lesions[5] and also a mixture of both hypo- and hyper-echoic lesions.[3] It has been postulated that lesional reflectivity may be dependent on the size and number of the dilated bile ducts and degree of fibrosis.[3] Other features of VMC include the presence of a comet tail artifact[2] and association with liver cysts.[5]
Contrast enhanced ultrasound (CEUS) allows a true assessment of lesional vascularity, with no escape of contrast through the interstitium.[6] This enables dynamic visualization of the lesion of interest through arterial, venous, and delayed phases. CEUS of two cases of VMC have been described. Berry et al.,[4] reported a case of multiple VMCs that did not demonstrate contrast enhancement in all phases; exclusion of hypovascular metastases was not possible. Hohmann et al.,[7] highlighted the presence of enhancement in a biliary hamartoma on CEUS with ‘washout’ in the delayed phase. However, this was a single biliary hamartoma, measuring 5 mm, which may have affected interpretation. Recently Murphy-Lavallee et al.,[8] has suggested that all metastases invariably display arterial vascularity on CEUS albeit transiently, despite hypovascular appearances on CT and MR imaging. This particular phenomenon is only evident through continuous dynamic observation unique to CEUS examination. In the present case, none of the lesions demonstrated contrast enhancement throughout all phases of the study, confirming the avascular nature of the abnormality.
On contrast enhanced CT, biliary hamartomas are predominantly of low attenuation, and may demonstrate an irregular border. The majority of cases reported suggest that VMC does not exhibit contrast enhancement, although one case of homogeneous enhancement has been reported.[2] Evaluation of lesional contrast enhancement on CT is not truly dynamic, unlike the evaluation of lesional enhancement on contrast ultrasound, and so CT scanning cannot definitively differentiate VMC from metastatic disease.
There have been several reports detailing MR imaging appearances of VMCs. All agree that VMCs appear hypointense on T1-weighted imaging and are hyperintense on heavily T2-weighted sequences with similar signal intensity to the spleen, but less than liver cysts;[13] our observations corroborate these findings. However, MR enhancement characteristics are difficult to establish with contradicting reports showing both enhancement[3] and no enhancement[1] on gadolinium-enhanced T1-weighted sequences. Our case did not demonstrate enhancement post-gadolinium. More recently, diffusion-weighted imaging (DWI) has gained recognition for its potential to differentiate metastatic lesions, showing restricted diffusion, from benign lesions, demonstrating free diffusion.[9] Although there are no published reports on DWI for VMC, our findings of free diffusion support a benign diagnosis.
There are a number of other potential causes for these appearances. Multiple cysts typically appear as anechoic areas with posterior acoustic shadowing on ultrasound and display very high T2 signal characteristics, with no enhancement with contrast. In abscess formation, peripheral enhancement, edema and gas may be demonstrated on a background of clinical sepsis.
While VMC has been described as a benign condition, there have been isolated reports of hepatic malignancies on a background of VMC, including hepatocellular carcinoma[10] and cholangiocarcinoma,[1] but given the paucity of reports, a clear association with VMC has not yet been established.
We report a case of von Meyenburg's complex that has been investigated with US, CEUS, CT, and MRI. B-mode ultrasound and CT do not help to differentiate hepatic metastases from VMC. However, lack of enhancement on CEUS, increased signal intensity on heavily T2-weighted MR sequences and free diffusion on DWI all favor benign disease, but currently biopsy must remain the gold standard for diagnosis.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2013/3/1/22/112804
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Bile duct hamartomas (von Meyenburg complexes): Value of MR imaging in diagnosis. Abdominal Imaging. 1999;24:171-3.
- [Google Scholar]
- The radiologic and pathologic spectrum of biliary hamartomas. Am J Roentgenol. 1995;165:309-13.
- [Google Scholar]
- MRI, CT, US and ERCP in the evaluation of bile duct hamartomas (von Meyenburg complex): A case report. Eur Radiol. 1998;8:1623-6.
- [Google Scholar]
- Case report: Microbubble contrast-enhanced ultrasound characteristics of multiple biliary hamartomas (von Meyenberg complexes) Ultrasound. 2004;12:95-7.
- [Google Scholar]
- Sonographic features of biliary hamartomas with histopathologic correlation. J Ultrasound Med. 2006;25:1631-3.
- [Google Scholar]
- Focal liver masses: Enhancement patterns on contrast-enhanced images-concordance of US scans with CT scans and MR images. Radiology. 2007;242:162-74.
- [Google Scholar]
- Assessment of a Biliary Hamartoma with Contrast-Enhanced Sonography using two Different Contrast Agents. Ultraschall Med. 2009;30:185-8.
- [Google Scholar]
- Are metastases really hypovascular in the arterial phase? The perspective based on contrast-enhanced ultrasonography. J Ultrasound Med. 2007;26:1545-56.
- [Google Scholar]
- Respiratory gated diffusion-weighted imaging of the liver: value of apparent diffusion coefficient measurements in the differentiation between most commonly encountered benign and malignant focal liver lesions. Eur Radiol. 2008;18:486-92.
- [Google Scholar]
- Hepatocellular carcinoma in association with bile duct hamartomas: Report on 2 cases and review of the literature. Ann Diagn Pathol. 2008;12:208-11.
- [Google Scholar]






