Translate this page into:
Angiographic Patterns of Transjugular Intrahepatic Portosystemic Shunt Dysfunction and Interventional Approaches to Shunt Revision
Address for correspondence: Dr. Ron C. Gaba, Department of Radiology, Division of Interventional Radiology, University of Illinois Hospital and Health Sciences System, 1740 West Taylor Street, MC 931, Chicago, IL 60612, USA. E-mail: rgaba@uic.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Transjugular intrahepatic portosystemic shunt (TIPS) is an established and effective treatment for the complications of portal hypertension. The non-trivial rates of shunt dysfunction inherent to TIPS mandate familiarity with the imaging diagnosis and endovascular management of this phenomenon. Herein, we present a pictorial review of the various angiographic patterns of TIPS dysfunction and illustrate traditional and innovative technical approaches to shunt revision.
Keywords
Ascites
dysfunction
encephalopathy
intervention
radiology
revision
shunt
transjugular intrahepatic portosystemic shunt
INTRODUCTION

- Dr. Ahmad Parvinian
Transjugular intrahepatic portosystemic shunt (TIPS) is an established treatment for the complications of portal hypertension.[1] However, the well-documented safety and efficacy of this procedure may be complicated by shunt dysfunction, which occurs in approximately 15% of covered stents and 44% of bare metal stents.[23] Because TIPS dysfunction may precipitate recurrence of portal hypertensive complications, it is incumbent upon interventional radiologists to be familiar with the diagnosis and management of shunt failure.[4] Herein, we review the various angiographic patterns of TIPS dysfunction and illustrate basic and advanced techniques for shunt revision. Institutional review board approval was obtained for this study.
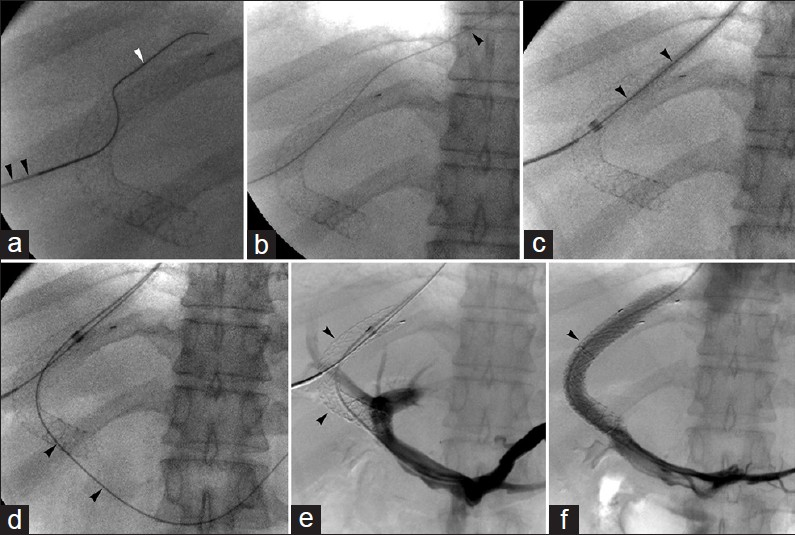
Patterns of TIPS dysfunction and basic shunt revision techniques
Conventional treatment options for TIPS dysfunction comprise various common techniques - namely, balloon angioplasty, shunt relining, and shunt extension- that may be applied alone or in combination to address an assortment of problems.[5] These approaches are particularly well-suited to the management of intimal hyperplasia [Figures 1 and 2], thrombotic occlusion [Figure 3], hepatic [Figures 4 and 5] and portal [Figure 6] venous end shunt stenosis, abnormal angulation [Figure 7], occult portosystemic pressure gradient elevation [Figure 8], and flow-sumping [Figure 9]. Awareness of benign findings such as pseudostenosis [Figure 10] is important to avoid unnecessary intervention.

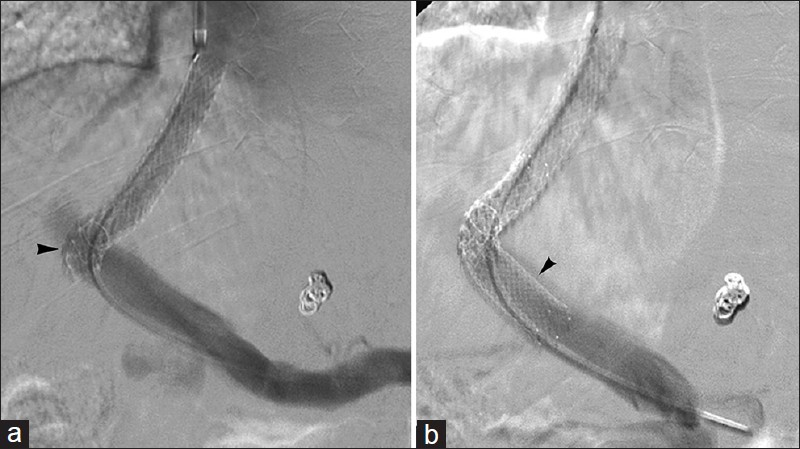
- Intimal hyperplasia. 53-year-old man with refractory ascites 5-years after bare metal TIPS. Portal venogram reveals moderate intimal hyperplasia along mid-to-distal shunt (arrowheads). Balloon angioplasty resulted in widely patent stent.
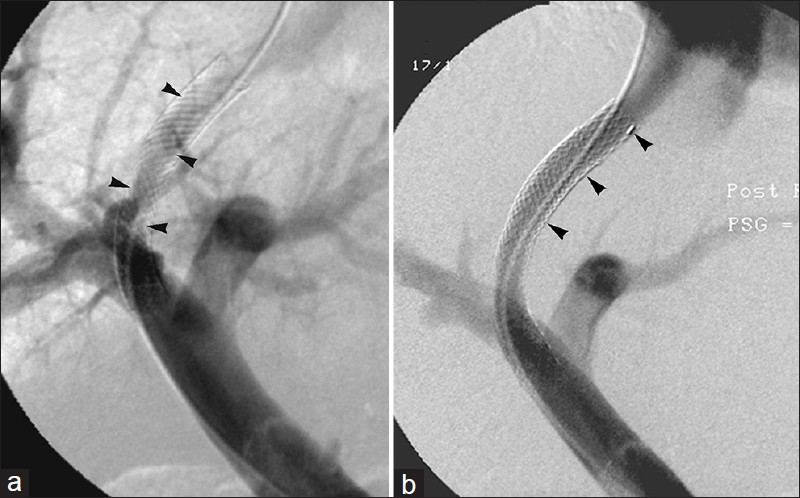
- Intimal hyperplasia treated with shunt relining. 63-year-old man with intractable ascites 1-month after bare metal TIPS. (a) Venogram reveals in-stent stenosis (arrowheads). (b) Shunt relining with covered stent (arrowheads) results in improved flow and no residual stenosis.

- Intra-graft thrombus. 72-year-old man with recurrent variceal hemorrhage 24-hours after TIPS. Venogram shows thrombus formation (arrowheads) within parenchymal portion of shunt. Portography following balloon maceration revealed no evidence of residual thrombus.
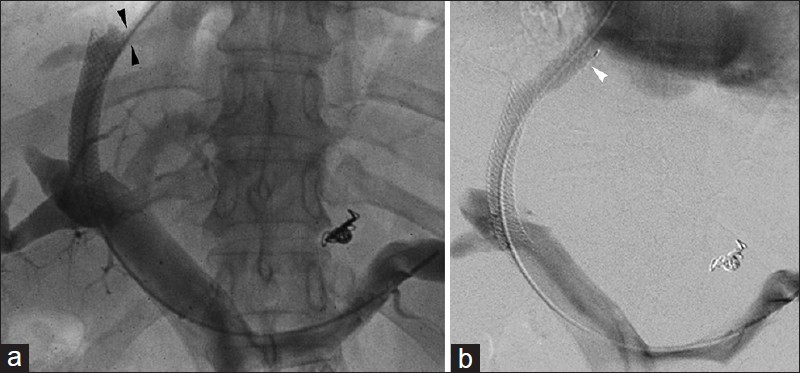
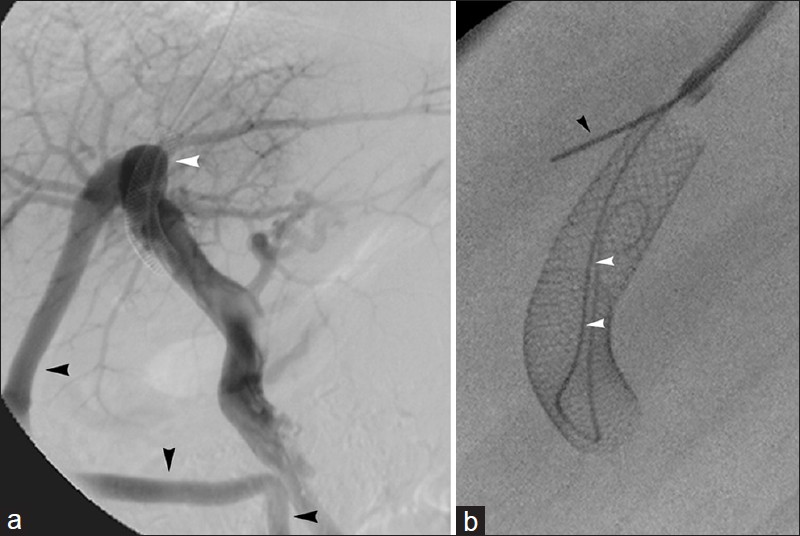
- Bare metal TIPS hepatic venous end stenosis in 50-year-old man. Recurrent variceal hemorrhage 8-years post-TIPS prompted imaging. (a) Venogram reveals significant hepatic venous end stenosis (arrowheads). (b) Relining with covered stent (arrowhead) eliminated stenosis.
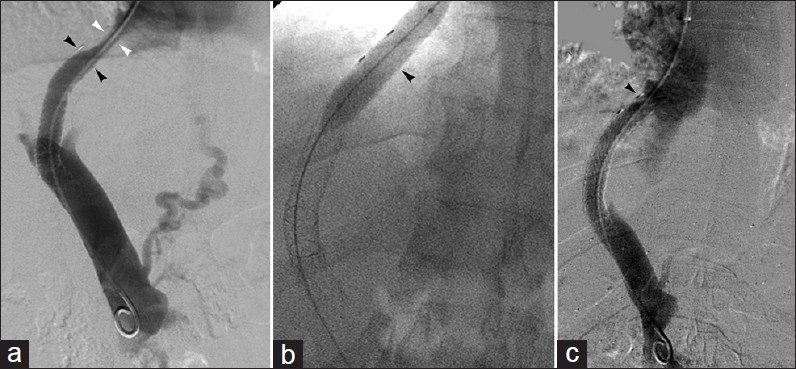
- Covered stent TIPS hepatic venous end stenosis in 50-year-old man with recurrent varices 6-months after TIPS. (a) Venogram reveals hepatic vein narrowing (white arrowheads) between stent and inferior vena cava confluence; initial stent (black arrowheads) length inadequate. (b) Balloon angioplasty (arrowhead) of narrowed segment followed by (c) covered stent (arrowhead) deployment to extend the length of the shunt.
- Portal venous end TIPS stenosis. 52-year-old man with recurrent ascites 3-years after TIPS. (a) Portal venogram reveals narrowed portal venous end (arrowhead). (b) Angioplasty and placement of a bare metal stenting (arrowhead) results in improved flow.
- Abnormal shunt angulation. 59-year-old woman with recurrent ascites 1-year after TIPS. (a) Acute angulation of stent portal venous end (arrowhead) disturbs normal flow. (b) Extension of shunt with bare metal stent (arrowhead) improves angulation and flow.

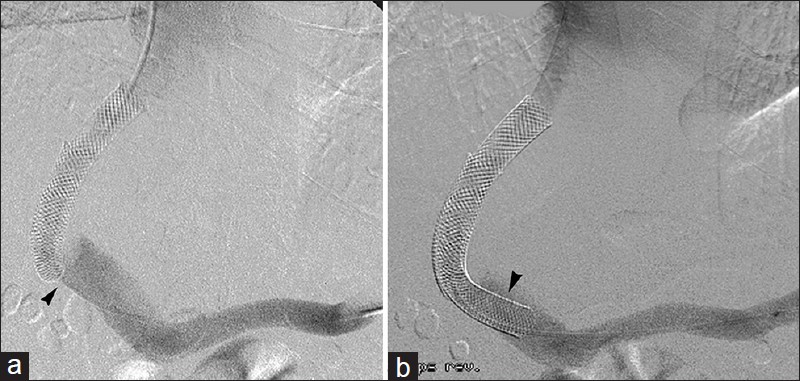
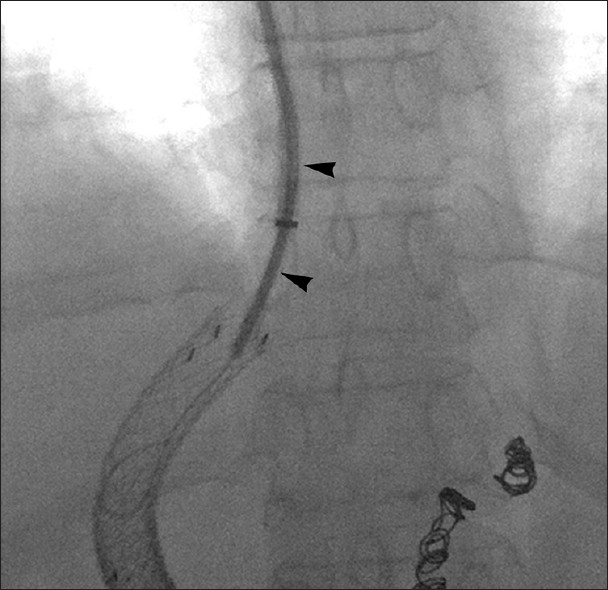
- Porto-systemic gradient (PSG) elevation. 67-year-old man with recurrent ascites and elevated 20 mm Hg PSG 3-months after TIPS. Venogram (a) demonstrates widely patent TIPS (arrowhead). (b) Balloon angioplasty lowered PSG to 10 mm Hg with no change in angiographic appearance of shunt (arrowhead).
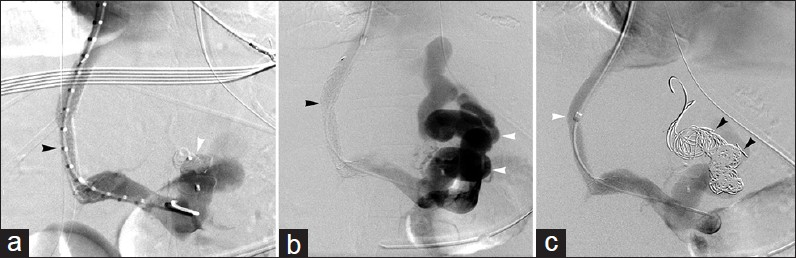
- TIPS flow consolidation. (a) 49-year-old woman with variceal bleeding underwent TIPS (black arrowhead) with embolization of large gastroesophageal varix using metallic vascular plug (white arrowhead). (b) Venogram after recurrent bleeding demonstrates reduced flow through TIPS (black arrowhead) due to siphoning of blood by recanalized varix (white arrowheads). (c) Variceal embolization using metallic coils (black arrowheads) consolidated flow through TIPS (white arrowhead).

- Pseudostenosis. (a) 57-year-old man with TIPS (white arrowhead) performed for refractory hepatic hydrothorax. Portal venography at time of shunt creation demonstrates antegrade flow in left portal vein (black arrowhead). Abnormal follow-up ultrasound flow velocity prompted (b) TIPS venogram which reveals pseudostenosis (black arrowheads) secondary to unopacified blood inflow (white arrowheads) from left portal vein, which showed physiologically reversed flow.
Advanced revision techniques
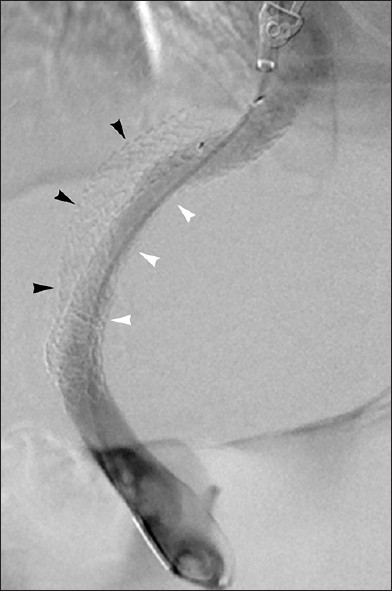
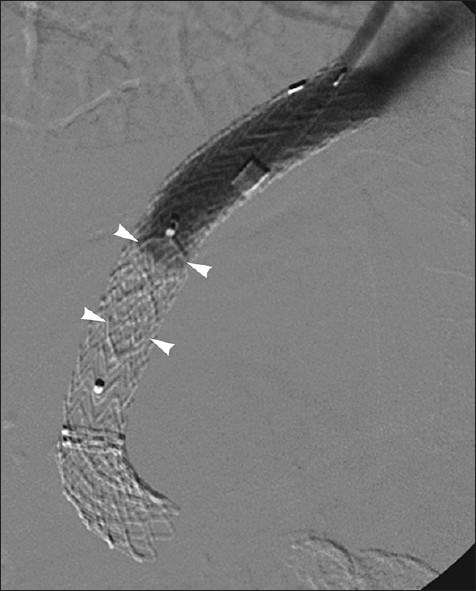
In technically difficult cases, conventional approaches to TIPS revision may not be feasible. For instance, complete shunt occlusion may preclude transjugular wire access and necessitate use of advanced methods such as back-end stiff guide wire [Figure 11] or metal cannula-supported shunt access [Figure 12], or even percutaneous transhepatic recanalization [Figure 13]. Patients with tumor vascular invasion and TIPS occlusion may require shunt extension [Figure 14]. Cases of insufficient portosystemic shunting may call for parallel TIPS [Figure 15] in order to achieve satisfactory clinical response; this technique also permits circumvention of an unsalvageable primary shunt [Figure 16]. Conversely, individuals who develop hepatic encephalopathy or liver failure due to excess portosystemic shunting necessitate TIPS reduction [Figure 17] or occlusion [Figure 18].
- Back-end stiff guidewire technique for shunt access. (a) 51-year-old man with occluded TIPS (white arrowhead) and outflow via recanalized paraumbilical vein (black arrowhead). (b) Due to technically challenging TIPS access, operator embedded back-end of stiff guidewire into liver parenchyma (black arrowhead) to secure sheath and allow wire access into shunt (white arrowheads) for revision.
- Metal transjugular cannula-supported shunt access. 60-year-old woman with occluded TIPS. 7 French angled stiffening cannula (arrowheads) advanced over guidewire to venous end of occluded stent. With cannula support, guidewire advanced through TIPS into portal vein, permitting successful revision.
- Percutaneous TIPS recanalization. 52-year-old man with bile leak-related TIPS occlusion. Operators failed access via transvenous approach, subsequently percutaneous recanalization approach was pursued. (a) Ultrasound-guided transhepatic needle (black arrowheads) access into occluded shunt followed by guidewire (white arrowhead) passage. (b) Wire (arrowhead) advanced into right atrium, and pulled out via internal jugular venous access using loop snare introduced into central circulation, establishing through-and-through access. (c) Sheath (arrowheads) then pulled into occluded TIPS, and (d) wire (arrowheads) guided into main portal vein. (e) Subsequent venogram confirmed TIPS occlusion (arrowheads). (f) Widely patent shunt following angioplasty and covered stent relining.

- Portal vein tumor. 53-year-old man with hepatocellular carcinoma and refractory ascites. (a) Large portal venous tumor filling defect (arrowheads) present at time of TIPS. (b) TIPS restored portal vein patency and improved ascites. Symptomatic recurrence 4-months later prompted venography (c), which revealed new tumor invasion at portal aspect of shunt (arrowheads). (d) Successful TIPS recanalization after further covered stent extension (arrowheads).

- Optimization of clinical response with parallel TIPS. 58-year-old man with refractory ascites. Primary TIPS (white arrowhead) resulted in insufficient PSG reduction to 22 mm Hg. Creation of parallel TIPS (black arrowhead) reduced PSG to 7 mm Hg and resulted in marked clinical improvement.
- Shunt occlusion treated with parallel TIPS. 58-year-old man with recurrent variceal hemorrhage. Unsuccessful recanalization of occluded TIPS (black arrowheads) prompted placement of second TIPS spanning middle hepatic vein to left portal vein (white arrowheads).

- Liver failure treated with shunt reduction. 52-year-old woman developed rising bilirubin after 10 mm TIPS with 6 mm Hg final PSG. (a) 6 mm balloon expandable stent and 10 mm covered stent introduced in parallel into TIPS. (b) Covered stent deployed to pin balloon expandable stent, which was subsequently dilated to 6 mm (c). (d) Compression of covered stent by balloon expandable stent results in reduced shunt diameter (arrowheads), PSG increased to 15 mm Hg, and resolved liver failure.
- Refractory hepatic encephalopathy in 58-year-old man 1-month after TIPS. Hepatic encephalopathy following TIPS is usually transitory but in this case encephalopathy failed to resolve. It was decided to completely occlude the TIP shunt with 10 mm metallic vascular plug (arrowheads). Patient recovered from encephalopathy and discharged home.
CONCLUSION
TIPS dysfunction is a common phenomenon that requires timely diagnosis and intervention. An understanding of the different causes of shunt failure and the approaches – both standard and innovative – to restoring patency of the shunt will optimize clinical outcomes in patients with portal hypertensive complications.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2013/3/1/19/111237
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- The role of transjugular intrahepatic portosystemic shunt (TIPS) in the management of portal hypertension. J Clin Gastroenterol. 2007;41(Suppl 3):S344-51.
- [Google Scholar]
- The transjugular intrahepatic portosystemic shunt: An update. AJR Am J Roentgenol. 2012;199:746-55.
- [Google Scholar]
- Patency of stents covered with polytetrafluoroethylene in patients treated by transjugular intrahepatic portosystemic shunts: Long-term results of a randomized multicentre study. Liver Int. 2007;27:742-7.
- [Google Scholar]
- Transjugular intrahepatic portosystemic shunt patency and the importance of stenosis location in the development of recurrent symptoms. Radiology. 1998;207:683-93.
- [Google Scholar]
- Evaluation and management of transjugular intrahepatic portosystemic shunts. AJR Am J Roentgenol. 2012;199:730-6.
- [Google Scholar]






