Translate this page into:
Anatomic Variations of the Right Portal Vein: Prevalence, Imaging Features, and Implications for Successful Transjugular Intrahepatic Portosystemic Shunt Creation
Address for correspondence: Dr. Ron C Gaba, Department of Radiology, Division of Interventional Radiology, University of Illinois Hospital and Health Sciences System, 1740 West Taylor Street, MC 931, Chicago, IL 60612, USA. E-mail: rgaba@uic.edu
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Given the widespread use of transjugular intrahepatic portosystemic shunt (TIPS) creation for the treatment of portal hypertensive complications, a working knowledge of portal venous anatomy is critical for interventional radiologists. The right portal vein – which is most commonly accessed during TIPS – is subject to various anatomic variants that may potentially impact procedure success. This pictorial essay characterizes the anatomic patterns of the right portal vein branching in terms of type and frequency based on case series review. The work also explains the potential procedural implications of the right portal vein anatomic variations as they pertain to TIPS technical success.
Keywords
Anatomy
portal vein
transjugular intrahepatic portosystemic shunt
variation

Introduction
For the past 25 years, transjugular intrahepatic portosystemic shunts (TIPS) have been employed worldwide as a recognized treatment for portal hypertensive complications[1] and have supplanted surgical shunts as the most frequently utilized portal decompression procedure.[2] Most commonly, TIPS creation involves transhepatic puncture of the right portal vein branch from the right hepatic vein approach. Although TIPS is commonly utilized in current clinical practice, transhepatic portal venous puncture may be technically demanding, requiring a firm understanding of the anatomy and spatial positioning of the right portal venous branch targets. Given the potential implications of portal venous anatomic variation on the right portal vein targeting, a better understanding of the right portal vein anatomic variations can optimize TIPS technical success among interventional radiology (IR) operators. With this in mind, this paper aims to describe the common anatomic branching patterns of the right portal vein, to define the prevalence of the right portal vein anatomic variations, to recognize right portal vein anatomic variations on cross-sectional imaging and portal venography during TIPS, and to explain potential procedural implications of the right portal vein anatomic variations as they pertain to TIPS technical success.
Methods
Computed tomography (CT) or magnetic resonance (MR) imaging cross-sectional imaging studies obtained before TIPS procedures as well as angiographic images during TIPS creation from 107 patients undergoing TIPS at a single tertiary care institution between 2010 and 2016 were retrospectively analyzed. Seven patients with cavernous transformation of the portal vein were excluded from analysis given vessel occlusion, yielding a final study population of 100. Right portal venous anatomy was classified according to the right portal vein variants as described in current literature.[3] The relative prevalence of each anatomic variation was calculated, and the anatomic implications for TIPS creation were assessed.
Right portal vein anatomic variations
Five common branching patterns were identified at our institution. The relative prevalence of each anatomic pattern is reported in Table 1, alongside comparative frequencies of the same variations in other published series.[345] Case-based imaging findings and implications for TIPS creation for each of the common right portal vein variations are described below.

Type 1: Conventional branching
In Type 1 (conventional) branching [Figure 1], the main portal vein bifurcates into right and left portal vein trunks. The right portal vein further bifurcates into an anterior branch supplying liver segments 5 and 8 and a posterior branch supplying liver segments 6 and 7. Type 1 anatomy facilitates TIPS creation in that it allows for a sizeable caliber right portal trunk target in a predictable location – positioned anterior and inferior to the right hepatic vein – while further permitting an obtuse shunt angulation when the right portal vein trunk is punctured. An obtuse shunt angle can facilitate device (e.g., catheter, sheath, stent) advancement through the transhepatic tract given inline access from the right jugular vein. As more acute shunt angulation has been associated with shunt dysfunction,[6] the obtuse angle also enhances shunt inflow from the portal vein, consequently improving portal decompression. In addition, Type 1 anatomy provides the option for selective puncture of the right anterior vessel, which can help to ensure that the posterior segmental portal vein branch is unobstructed by the covered component of a deployed TIPS stent-graft; this is relevant as a recent series demonstrated a possible association between post-TIPS segmental portal vein thrombosis and possible hepatic ischemia.[7]

- Type 1 right portal venous branching in an 89-year-old man with variceal hemorrhage. Axial contrast-enhanced magnetic resonance image (a) demonstrates bifurcation of the main portal vein into the left portal vein (white arrow) and right portal vein (black arrow) from which anterior branch (white arrowhead) supplying liver segments 5 and 8 and posterior vessel (black arrowhead) supplying segments 6 and 7 arise. Direct portal venogram (b) during transjugular intrahepatic portosystemic shunt creation confirms conventional right portal vein (black arrow) branching into anterior (white arrowhead) and posterior (black arrowhead) vessels.
Type 2: Trifurcation branching
In Type 2 (trifurcation) portal vein anatomy [Figure 2], the main portal vein trifurcates into a left portal vein, right anterior portal vein supplying liver segments 5 and 8, and right posterior portal vein supplying liver segments 6 and 7 at the same craniocaudal level. Type 2 anatomy can potentially make TIPS creation more challenging by requiring puncture of a segmental right portal vein target vessel – either the right anterior or posterior portal vein branches – which is typically smaller than in caliber than the right portal trunk target in Type 1 anatomy. In addition, a right anterior, posterior, or more peripheral puncture may result in challenging marginal access, which can be associated with acute shunt angulation that renders device advancement through the intrahepatic tract more difficult, while also potentially disturbing shunt inflow. However, similar to Type 1 anatomy, Type 2 anatomy provides the option for selective puncture of the right anterior portal vessel, which can help to ensure that the posterior segmental portal vein branch is unobstructed by the covered component of a deployed TIPS stent-graft to optimize patency. The portal vein trifurcation can also be punctured in lieu of targeting a segmental portal venous branch.
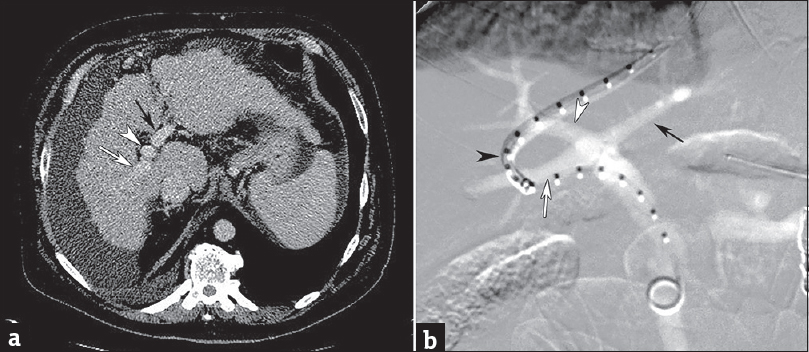
- Type 2 right portal venous branching in a 58-year-old man with medically refractory ascites. Axial contrast enhanced computed tomography image (a) shows trifurcation of portal vein, giving rise to the left portal vein (black arrow), right anterior vessel (arrowhead) supplying liver segments 5 and 8, and right posterior branch (white arrow) supplying liver segments 6 and 7 at same craniocaudal anatomic level. Direct portal venogram (b) during transjugular intrahepatic portosystemic shunt creation better delineates trifurcation of main portal vein into left portal vein (black arrow), right anterior portal vein (white arrowhead), and right posterior portal vein (white arrow). Note peripheral portal venous access with associated acute angulation (black arrowhead).
Type 3: Early branching
In Type 3 (early) branching of the right posterior portal vein [Figure 3], the first branch arising from the main portal vein is the right posterior segmental branch supplying liver segments 6 and 7. Beyond this early branch, the left portal vein supplying the left hepatic lobe and the right anterior portal vein supplying liver segments 5 and 8 bifurcate at the same level. Type 3 anatomy can make TIPS creation more challenging by providing a smaller caliber right anterior or posterior portal vein puncture target in a less predictable location compared to the larger right main portal trunk target positioned in a more expected location as in Type 1 anatomy. Furthermore, smaller caliber vessel segmental target vessels – such as the right anterior or right posterior portal vein – may necessitate a more peripheral access that can result in acute shunt angulation similar to Type 2 anatomy. On the contrary, much like Type 1 and Type 2 anatomy, Type 3 right portal vein branching can facilitate TIPS creation by again allowing for selective puncture of the right anterior segmental vessel, which can theoretically maintain portal flow to the right posterior segments, limiting hepatic ischemia. If puncture of the right posterior portal vein is desired, this may require that access be obtained from a more peripheral right hepatic venous location.

- Type 3 right portal venous branching in a 44-year-old man with medically refractory ascites. Axial contrast-enhanced magnetic resonance image (a) depicts early branching of right posterior portal vein (arrow) supplying liver segments 6 and 7 as the first branch of main portal vein (arrowhead). Direct portal venogram (b) during transjugular intrahepatic portosystemic shunt creation illustrates left portal vein (black arrow) and right anterior portal vein branch supplying liver segments 5 and 8 (arrowhead) arising from the main portal vein beyond the origin of early right posterior portal vein branch (white arrow). Note access of right posterior portal vein branch in this case.
Type 4: Separate segment 7 branching
In Type 4 (separate segment 7) anatomy [Figure 4], the right portal vein bifurcates into two vessels – one larger vessel supplying liver segments 5, 6, and 8 and a smaller vessel supplying liver segment 7 only – beyond the left portal vein origin from the main portal vein. Type 4 anatomy impacts TIPS creation in much the same way as Type 1 anatomy. This variant allows for a sizeable caliber right portal trunk generally positioned in a predictable location anterior and inferior to the right hepatic vein. In addition, similar to Type 1 anatomy, if the right main portal trunk is targeted, an obtuse shunt angulation can be achieved which would facilitate inline device advancement through the transhepatic tract and optimize shunt inflow for portal decompression.

- Type 4 right portal venous branching in a 56-year-old woman with variceal hemorrhage. Axial contrast enhanced computed tomography image (a) demonstrates separate segment 7 anatomy. After left portal vein origin (black arrow), right portal vein bifurcates into two vessels, one supplying liver segment 7 only (white arrow) and another supplying liver segments 5, 6, and 8 (arrowhead). Direct portal venogram (b) during transjugular intrahepatic portosystemic shunt creation corroborates cross-sectional imaging and shows bifurcation of the right portal vein into two vessels, one supplying liver segment 7 only (white arrow) and another supplying liver segments 5, 6, and 8 (arrowhead).
Type 5: Separate segment 6 branching
In Type 5 (separate segment 6) anatomy [Figure 5], the right portal vein bifurcates into two vessels – one supplying liver segment 6 only and another branch supplying liver segments 5, 7, and 8 – beyond the left portal vein origin from the main portal vein. Type 5 anatomy can facilitate TIPS creation in much the same way as Type 1 and Type 4 anatomy. This variant allows for a sizeable caliber right portal trunk situated in a predictable location anterior and inferior to the right hepatic vein. Moreover, being able to target a right portal trunk can enable straight device advancement through the transhepatic tract while maximizing inline shunt flow and portal decompression.

- Type 5 right portal venous branching in a 51-year-old man with medically refractory ascites. Coronal reconstructed contrast enhanced computed tomography image (a) depicts right portal vein bifurcation into two vessels, one supplying liver segment 6 only (white arrow) and another branch supplying liver segments 5, 7, and 8 (arrowhead). Wedged hepatic venogram (b) during transjugular intrahepatic portosystemic shunt creation substantiates this finding and illustrates the right portal vein bifurcation into two vessels, one supplying liver segment 6 only (white arrow) and another branch supplying liver segments 5, 7, and 8 (arrowhead), beyond the origin of left portal vein (black arrow).
Miscellaneous branching patterns
Examples of described nonstandard anatomic variants include quadrification and separate origin of the liver segments 6 and 7 branch from the main portal vein.[4] The most common miscellaneous variant seen in the current series was the right portal vein bifurcation into separate superior and inferior branches supplying liver segments 6/7 and 5/6, respectively (3% of total, 38% of miscellaneous branching patterns) [Figure 6].

- Miscellaneous right portal vein branching pattern in a 63-year-old man with variceal hemorrhage. Axial contrast enhanced computed tomography image (a) demonstrates bifurcation of the right portal vein into separate superior (black arrow) and inferior (white arrow) branches supplying liver segments 6/7 and 5/6, respectively; left portal trunk denoted by an arrowhead. Direct portal venogram (b) during transjugular intrahepatic portosystemic shunt creation supports this finding and shows right portal trunk (black arrowhead) bifurcation into superior (black arrow) and inferior (white arrow) segmental branches; left portal trunk denoted by an arrowhead.
Discussion
Embryologically, the portal vein develops from the vitelline (omphalomesenteric vein), one of the three major venous systems of the developing embryo (in addition to the umbilical and cardinal veins).[89] At 5 weeks gestational age, the right and left vitelline veins forms a branching venous plexus around the duodenum, comprising two components ventral to the duodenum and one component dorsal to the duodenum, before terminating in the sinus venous. By 10 weeks, selective involution of portions of this venous plexus gives rise to the adult portal vein. The main portal vein arises from the left vitelline vein and dorsal anastomoses, the right portal vein arises from the right vitteline vein, and the left portal vein arises from the left vitteline vein and ventral anastomoses. Deviations in the development and selective involution of this venous plexus lead to portal vein variation.
Anatomic variations of the right portal vein are often encountered during TIPS creation. Conventional Type 1 portal venous anatomy – in which the portal vein arborization follows the lobar and segmental anatomy of the liver as described by Couinaud[10] – was the most commonly encountered branching pattern in the current study, corroborating the high prevalence reported in other published series.[345] However, the portal vein demonstrates other variations in up to one-third of cases, with trifurcation type branching occurring with the second highest frequency. Interestingly, nonstandard miscellaneous variations beyond the described Types 1–5 variants were seen in 8% of cases, with the most common being right portal vein bifurcation into separate superior and inferior branches supplying liver segments 6/7 and 5/6, respectively. Notably, while the right portal vein shows substantial anatomic variation, left portal venous anomalies are less frequently encountered, although some variants – such as a separate origin of the liver segment 4 portal vein branch from the main portal vein – have been described.[4]
The relative prevalence of portal vein anatomic variants mandates attentive consideration to portal vein anatomy prior to undertaking interventions such as TIPS. As described herein, anomalous portal venous anatomy can potentially impact transhepatic access, and contrast-enhanced CT or MR imaging prior to TIPS is thus critical for preprocedural planning given the high frequency of right portal variation. Cross-sectional imaging can help to identify optimal portal vein puncture targets and their spatial relationship with each of the hepatic veins as well as other anatomic landmarks (e.g., vertebral bodies or ribs). While preprocedural ultrasound cannot provide the same anatomic detail. Doppler imaging may be prudent to ensure portal venous patency in individuals who cannot undergo CT or MR imaging. As a final note, use of intravascular ultrasound guidance for TIPS creation[111213] provides an additional means for IR operators to identify and target portal vein branches during TIPS procedures and may render some of the more challenging anatomic cases technically easier given the ability to visualize and puncture vessels with real-time observation.
While the current series are smaller in sample size than prior reported studies,[345] those prior publications merely utilized CT imaging for portal venous anatomic delineation. In contrast, the strengths of the current series lie in its correlation of CT and MR imaging cross-sectional imaging with angiographic images obtained during TIPS procedures and description of the implications of portal venous variants on TIPS creation. It should be noted, however, that the described consequences represent observations based on both anatomy and operator experiences and those generalizations may not hold in individual cases depending on factors such as size, morphology, degree of fibrosis or cirrhosis, and orientation of the liver as well as presence or absence of portosystemic shunts and patency of the spleno-mesenterico-portal venous system.
Conclusion
Portal venous anatomic variation – particularly those involving the right portal vein – is a common occurrence. Given the increasing utilization of TIPS, a greater understanding of right portal venous branching patterns will enhance the ability of IR operators to complete technically successful shunt creation while optimizing patient safety.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2017/7/1/14/203163
References
- Portosystemic shunts: Stable utilization and improved outcomes, two decades after the transjugular intrahepatic portosystemic shunt. J Am Coll Radiol. 2015;12(12 Pt B):1427-33.
- [Google Scholar]
- Incidence, patterns, and clinical relevance of variant portal vein anatomy. AJR Am J Roentgenol. 2004;183:1055-64.
- [Google Scholar]
- Portal vein variations: Clinical implications and frequencies in routine abdominal multidetector CT. Diagn Interv Radiol. 2007;13:75-80.
- [Google Scholar]
- Portal vein variations in 1000 patients: Surgical and radiological importance. Br J Radiol. 2015;88:20150326.
- [Google Scholar]
- Segmental liver ischemia/infarction after elective transjugular intrahepatic portosystemic shunt creation: Clinical outcomes in 10 patients. J Vasc Interv Radiol. 2015;26:835-41.
- [Google Scholar]
- Insight into congenital absence of the portal vein: Is it rare? World J Gastroenterol. 2008;14:5969-79.
- [Google Scholar]
- Definition of hepatic anatomical regions and their value during hepatectomy (author's transl) Chirurgie. 1980;106:103-8.
- [Google Scholar]
- Intravascular US-guided portal vein access: Improved procedural metrics during TIPS creation. J Vasc Interv Radiol. 2016;27:1140-7.
- [Google Scholar]
- Intravascular ultrasound in the creation of transhepatic portosystemic shunts reduces needle passes, radiation dose, and procedure time: A retrospective study of a single-institution experience. J Vasc Interv Radiol. 2016;27:1148-53.
- [Google Scholar]
- Utility of intravascular US-guided portal vein access during transjugular intrahepatic portosystemic shunt creation: Retrospective comparison with conventional technique in 109 patients. J Vasc Interv Radiol. 2016;27:1154-9.
- [Google Scholar]






