Translate this page into:
An Unusual Radiological Presentation of a Pulmonary Hydatid Cyst in a Child
Address for correspondence: Dr. Servet Kayhan, Department of Pulmonary Disease, Recep Tayyip Erdogan University, School of Medicine, Rize, Turkey. E-mail: kayhanservet@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Giant pulmonary hydatid cyst is usually encountered in adolescents and children who are older than 10 years. A relatively higher elasticity of the lung tissue allows rapid growth of cysts. We present a case of a 15-year-old male who was admitted with complaint of frequent and persistent dry cough for over a month. Computed tomographic scan revealed a giant cyst with thick enhancing rim and an “air bubble” sign. Diagnosis of giant hydatid cyst was confirmed by surgery and histopathological examination.
Keywords
Air bubble sign
echinococcus granulosus
giant pulmonary hydatid cyst
thoracic surgery
INTRODUCTION

Hydatid cystic disease is a significant disease in endemic regions. Giant pulmonary hydatid cyst is a parasitic disease caused by Echinococcus granulosus, and it is characterized by cystic lesions that are 10 cm or larger in diameter in the lungs.[12] This entity is most frequently encountered in adolescents and in children older than 10 years. The relatively higher elasticity of the lung tissue allows rapid growth of cysts.[3] Liver is the most commonly affected organ in adults, and the lung is the predominant site of cyst formation in children.[34]
We present here a case of unique unruptured hydatid cyst with thick enhancing rim and an "air bubble" sign resembling a lung abscess or ruptured cyst. The patient was a previously healthy, 15-year-old child who presented with frequent dry cough that had persisted for a month.
RADIOLOGICAL FEATURES
Postero-anterior chest radiograph showed a very large dense homogenous opacity in the right lower hemithorax [Figure 1]. Computed tomography (CT) scan of the thorax revealed a giant pulmonary cyst (14.4 × 11.2 × 9.3 cm) with a thick enhancing rim (1.29 cm) [Figure 2] and an “air bubble” sign [Figure 3]. Abdominal ultrasonography was normal. Fiberoptic bronchoscopy showed external compression and narrowing in the middle and lower bronchi of the right lung.
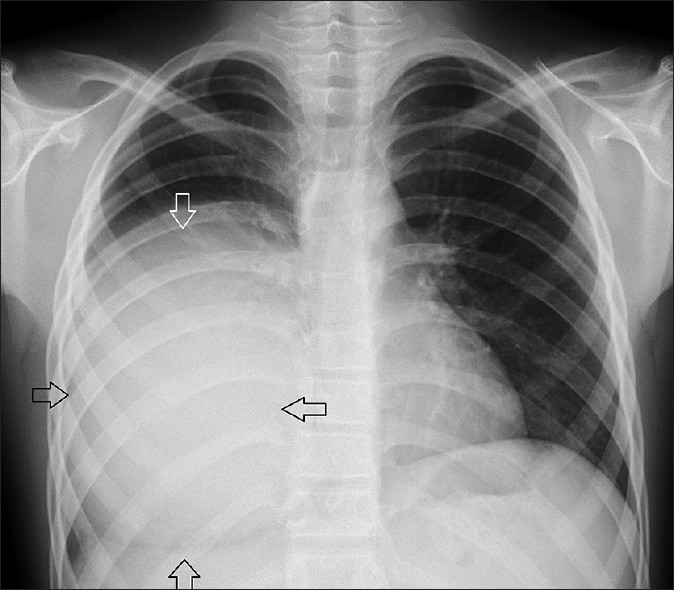
- 15-year-old male patient with frequent cough. Postero-anterior chest radiograph shows a very large dense homogenous opacity (arrows) in the right lower hemithorax.
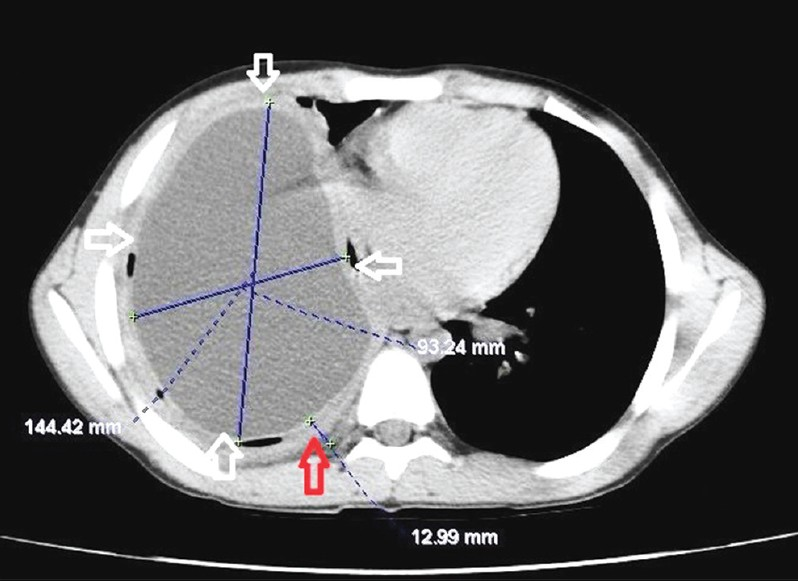
- Giant pulmonary hydatid cyst. Axial computed tomography of chest (mediastinal window) reveals fluid containing giant cyst measuring 14.4 × 9.3 cm (white arrows) with a thick-enhancing wall (1.29 cm), (red arrow).

- The “air bubble” sign. Axial computed tomographic scan of the chest (mediastinal window) shows air bubbles in regions surrounding the cyst (arrows).
PATHOLOGICAL FEATURES
Diagnostic and therapeutic thoracotomy as well as cystotomy and obliteration of the residual cavity by capitonnage were performed. Diagnosis of giant hydatid cyst was confirmed by histological examination after surgery. Macroscopic appearance of the cyst [Figure 4] and microscopic examination [Figure 5] revealed the hydatid cyst wall with eosinophilic lamellar cuticular membrane and scolex of Echinococcus granulosus. Chest radiograph showed that the right lung had completely expanded after surgery [Figure 6].

- Pathology of the specimen. Macroscopic appearance of the resected hydatid cyst (black arrow) and adherent lung tissues (white arrows).
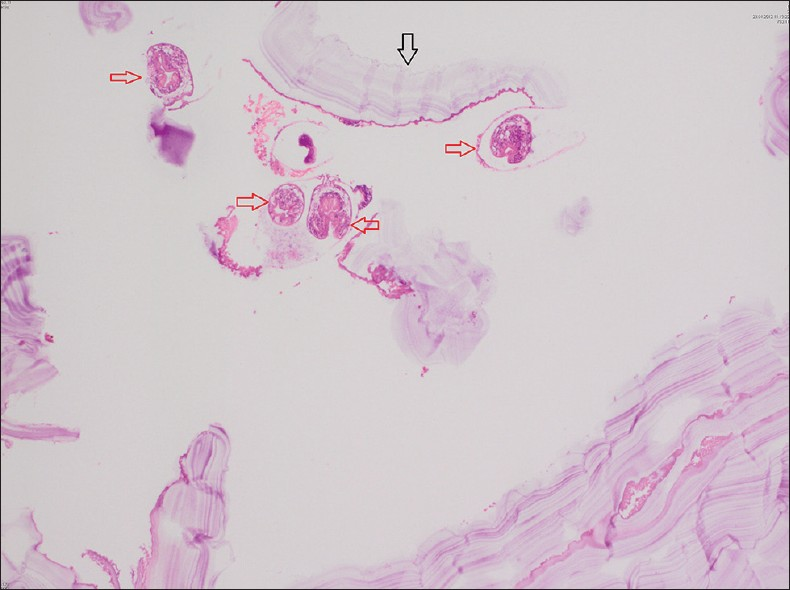
- Microscopic examination. H and E, stained sample at ×40 magnification reveals the cyst wall with eosinophilic lamellar cuticular membrane (black arrow) and scolex of Echinococcus granulosus (red arrows).
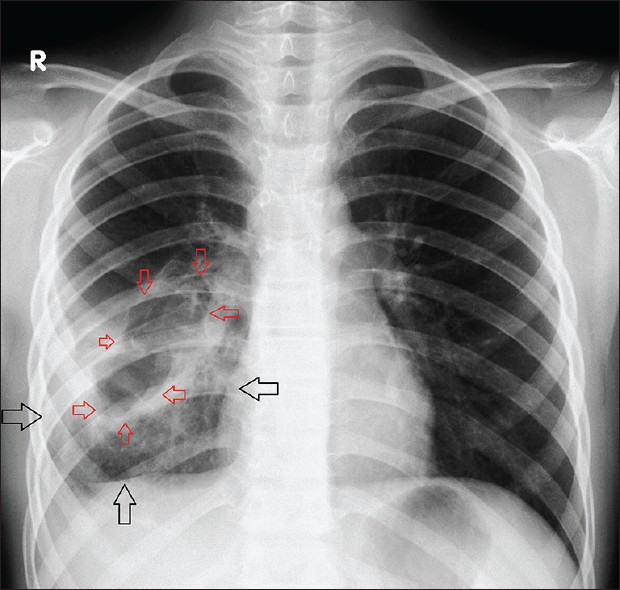
- Postoperative postero-anterior chest radiograph of the case reveals complete expansion of the right lung (black arrows). Wedge resection additional to the cavitary procedure (capitonnage) was performed because of damage to the adjacent parenchyma of the involved lung caused by infection. Postsurgical change in the right lower lobe after surgical removal of the cyst (red arrows).
DISCUSSION
Pulmonary hydatid cystic disease caused by Echinococcus granulosus is still an important problem in endemic areas of Middle and Eastern Europe including Turkey, South America, Australia, and South Africa. Pulmonary hydatid cystic disease is frequently asymptomatic in children.[2] Common presenting symptoms of giant pulmonary hydatid cyst are related to compression of tissue and they present as dry cough, chest pain, dyspnea, and ruptured cyst can cause productive cough and very rarely anaphylaxis.[2] In our patient, dry cough was the single symptom present at admission. Biochemical and physical examination findings have limited value in diagnosis of pulmonary hydatid disease.[5] In our patient, on examination of the respiratory system, breath sounds were decreased and percussion note was dull in right infrascapular area. In laboratory investigation, total leucocyte count was 16700/mm3 cells with 73.2% neutrophils, 16.3% lymphocytes, 9.5% monocytes, and 0.4% eosinophils. Erythrocyte sedimentation rate was 98 mm/h, c-reactive protein (CRP) level was 9.1 mg/dL, hematocrit level was 32%, and hemoglobin level was 11.3 mg/dL. Serological tests have limited diagnostic value and enzyme-linked immunoabsorbent assay was positive only in less than 50% cases of pulmonary hydatid cyst. Indirect hemaglutination test for E. granulosus was negative in this case. The chest X-ray and thoracic CT are generally sufficient for diagnosis of hydatid cyst.[6] Giant pulmonary hydatid cysts are usually located in the right lower lobe. Giant pulmonary hydatid cyst may mimic diaphragmatic elevation on chest radiograph and cause an error in its diagnosis.[7] Unruptured pulmonary hydatid cyst shows one or more homogenous round or oval masses with smooth borders surrounded by normal lung tissue on chest radiograph.[6]
The “air bubble” sign, although a relatively newly recognized radiological sign, has been now established as a very sensitive and specific sign in diagnosis of ruptured, infected hydatid cyst. The “air bubble” sign may develop as a consequence of cyst rupture, secondary to bacterial infections like bronchopneumonia or lung abscess.[8] The diagnosis of unruptured hydatid cyst was straightforward in our case according to the clinical presentation and imaging.
Surgery revealed that the present case had an unruptured cyst. It is thought that the presence of air within the pericystic area was caused by obstructive pulmonary infection and passive atelectasis secondary to giant cyst. Hydatid cyst was intact during operation and the excision of the cyst was performed including a wedge of the adjacent lung tissue.
Water lily sign, crescent sign, cumbo's sign, serpent sign, and monod's sign are the other pathognomic radiologic signs for ruptured hydatid cyst.[6] CT scan can demonstrate the cystic nature of lung lesion and a thin enhancing rim, if the cyst is intact. We presented here a unique case of unruptured hydatid cyst showing a thick enhancing rim with "air bubble" sign mimicking lung abcess or ruptured cyst.
A definite diagnosis of hydatid cyst was based on surgery and pathological confirmation. Surgery is the first treatment modality of choice for hydatid cystic disease and medical treatment can be used during the postoperative period in order to prevent recurrence.
CONCLUSION
Hydatid cystic disease may mimic other pulmonary diseases such as pulmonary abscess and should be considered in the differential diagnosis of uncertain chest pathologies, especially in rural areas of endemic countries.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2013/3/1/20/111238
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Atypical pulmonary giant hydatid cyst as bilaterally symmetrical solitary cysts. Asian Cardiovasc Thorac Ann. 2004;12:257-9.
- [Google Scholar]
- Radiological characteristics of pulmonary hydatid disease in children: Less common radiological appearances. Eur J Radiol. 2003;45:123-8.
- [Google Scholar]
- Histopathologically diagnosed pulmonary complicated hydatid cyst cases. Turkiye Parazitol Derg. 2011;35:189-93.
- [Google Scholar]
- Giant pulmonary hydatid cyst mimicking elevated diaphragm: A diagnostic dilemma. Ann Afr Med. 2012;11:122-3.
- [Google Scholar]
- “Air-bubble” signs in the CT diagnosis of perforated pulmonary hydatid cyst: Three case reports. Minerva Pediatr. 2008;60:361-4.
- [Google Scholar]






