Translate this page into:
An Anatomic, Imaging, and Clinical Review of the Medial Longitudinal Fasciculus
*Corresponding author: Saif Ahmed Baig, Department of Neuroradiology, University of Florida Health Jacksonville, Jacksonville, Florida, United States. saif.baigmd@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Fiester P, Baig SA, Patel J, Rao D. An anatomic, imaging, and clinical review of the medial longitudinal fasciculus. J Clin Imaging Sci 2020;10:83.
Abstract
The medial longitudinal fasciculus (MLF) is a paired, highly specialized, and heavily myelinated nerve bundle responsible for extraocular muscle movements, including the oculomotor reflex, saccadic eye movements an smooth pursuit, and the vestibular ocular reflex. Clinically, lesions of the MLF are classically associated with internuclear ophthalmoplegia. However, clinical manifestations of a lesion in the MLF may be more complex and variable. We provide an overview of the neuroanatomy, neurologic manifestations, and correlative examples of the imaging findings on brain MRI of MLF lesions to provide the clinician and radiologist with a more comprehensive understanding of the MLF and potential clinical manifestations for an MLF lesion.
Keywords
Medial longitudinal fasciculus
Internuclear opthalmoplegia
Trochlear syndrome
One-and-a-half syndrome
Wall-eyed bilateral internuclear opthalmoparesis syndrome
INTRODUCTION
Internuclear opthalmoplegia is defined as the lack of adduction of the ipsilateral eye with preserved abduction of the contralateral eye with nystagmus. It is the result of a lesion affecting the medial longitudinal fasciculus (MLF) – a paired, highly specialized, and heavily myelinated nerve bundle traveling in a craniocaudid direction near the midline within the tegmentum of the midbrain and dorsal pons. Functionally, the MLF carries excitatory and inhibitory axonal nerve between the paramedian pontine retricular formation (PPRF) and cranial nerves III, IV, and VI during activation of the frontal eye fields in the cerebral cortex. This allows for agonist and antagonist extraocular muscle movement for saccadic eye movement (horizontal eye movement allowing for change in fixation point) and smooth pursuit (eye movement allowing for following a moving object). In addition, vestibular-ocular nerve fibers traveling from cranial nerve VIII, which include both a semicircular and otolith-mediated oculomotor reflex, also run within the MLF to help coordinate balance and linear acceleration, respectively.[1,2]
While a lesion in the MLF is classically associated with internuclear opthalmoplegia, the clinical manifestations may in fact be more complex and variable than conventionally taught. This may be related to two factors: (1) Exact lesion location within the MLF tract and (2) confounding symptoms from additional pathology outside the MLF tracts. Depending on location, a lesion within the MLF may produce specific clinical signs and can be divided clinically into four distinct categories of disease: (1) Internuclear ophthalmoplegia (INO), (2) INO and trochlear syndrome, (3) INO and one- and -a -half syndrome, and (4) wall-eyed bilateral INO syndrome.[2-4] These entities are defined separately from isolated lesions of the oculomotor nuclei or abducens nuclei and/or PPRF.[5] In addition, a lesion affecting the MLF may result in dizziness with or without extraocular muscle dysfunction secondary to involvement of the vestibular-ocular reflexes (VORs) which are also located in these heavily myelinated pathways.[6,7]
Thus, we provide an overview of the neuroanatomy of the MLF and the spectrum of potential neurologic manifestations that may present on clinical examination. We offer several examples of the imaging findings on brain MRI of MLF lesions and discuss the common pathology that may lead to abnormalities in synchronized horizontal eye movement.
NEUROANATOMY AND INO-RELATED SYNDROMES
Internuclear opthalmoparesis
The neurologic pathway for synchronized and horizontal conjugate gaze runs through the MLF. Input from the frontal eye field activates the PPRF, which, in turn, transmits two signal through the CN VI nuclei [Figure 1]. One signal activates the ipsilateral lateral rectus muscle, while another signal travels in the contralateral MLF to activate the contralateral CN III nuclei and the medial rectus muscle. A lesion in the MLF classically results in INO (preserved abduction of the contralateral eye with nystagmus and weakened adduction of the ipsilateral eye); however, depending on lesion location within the MLF, several specific neurologic manifestations may result [Figure 2].
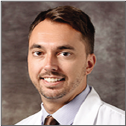
- The medial longitudinal fasciculus (MLF) carries excitatory and inhibitory axonal nerves between the paramedian pontine retricular formation and cranial nerves III, IV, and VI during activation of the frontal eye fields in the cerebral cortex. Axial T2-weighted sequence (a) of the midbrain demonstrating MLF (magenta circles), oculomotor III (blue circles), and trochlear IV (green circles) nuclei. Axial T2-weighted sequence (b) of the dorsal pons demonstrating abducens VI nuclei (orange circles) and MLF (magenta circles).

- A lesion isolated within the heavily myelinated white matter tract of the medial longitudinal fasciculus disrupts the signal from the contralateral abducens nucleus (CN VI) transmitted through the paramedian pontine retricular formation. This allows abduction of the contralateral eye with nystagmus, but disrupts the synchronized horizontal gaze of the other eye resulting in weakened or absent adduction of the opposite globe.
Internuclear opthalmoparesis and trochlear syndrome
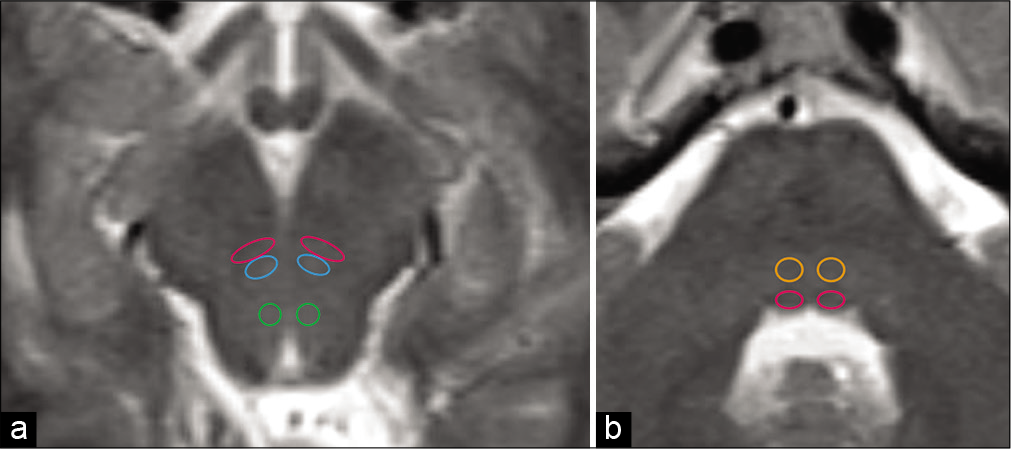
INO and trochlear syndrome results from a lesion affecting the MLF at the caudal midbrain as well as the adjacent ipsiltateral trochlear nucleus. The trochlear nucleus is embedded within the MLF between the superior and inferior colliculi in the tegmentum of the midbrain. The trochlear nerve is the only cranial nerve with fibers that decussate and exit dorsally into the superior medullary velum before coursing around the midbrain to innervate the superior oblique muscle. Thus, a lesion affecting both the MLF and ipsilateral trochlear nucleus presents clinically as INO with a contralateral globe hyperdeviation due to the loss of innervation of the contralateral superior oblique muscle [Figure 3].
- A lesion located at the level of the caudal midbrain between the superior and inferior colliculi affects both the medial longitudinal fasciculus and ipsilateral trochlear nucleus resulting in internuclear ophthalmoplegia (INO) and trochlear syndrome. Clinically, this presents as INO with a contralateral hyperdeviation of the globe due to loss of innervation of the superior oblique muscle.
Internuclear opthalmoparesis and one-and-a-half syndrome
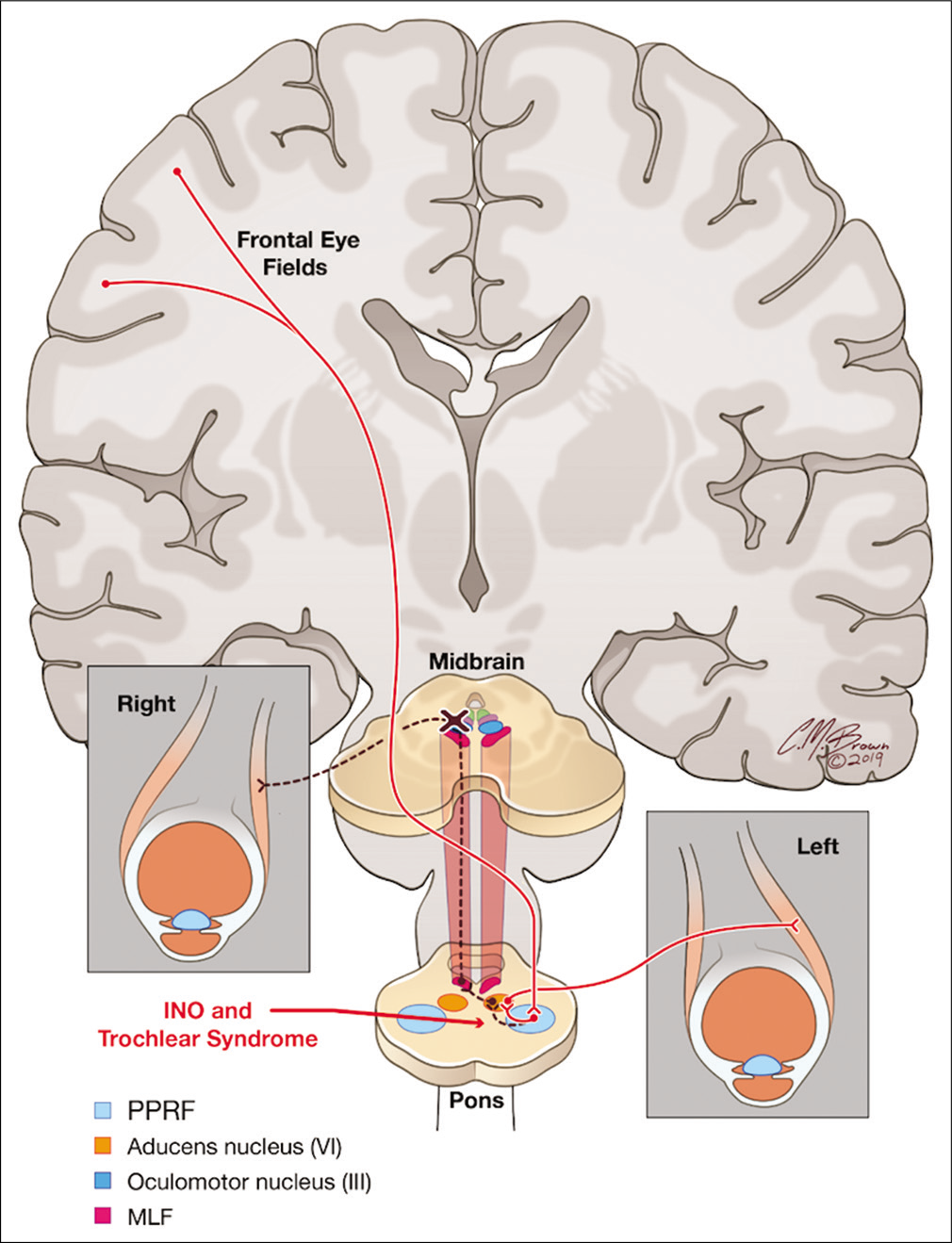
INO and one-in-a-half syndrome result from a lesion affecting the MLF at the dorsal pontine tegmentum and the ipsilateral abducens nuclei or paramedian pontine reticular formation (PPRF). The PPRF receives input from the frontal eye field in the cerebral cortex and relays a signal to activate the abducens nuclei and lateral rectus muscle. Thus, a lesion involving the MLF and adjacent PPRF or abducens nucleus results clinically in INO in one direction and a lateral gaze palsy in the other direction [Figure 4].
- A lesion located in the dorsal pontine tegmentum affects both the medial longitudinal fasciculus and the ipsilateral abducens nuclei and/or paramedian pontine retricular formation. Clinically, this presents with internuclear ophthalmoplegia with horizontal gaze in one direction and lateral gaze palsy in the other direction.
Wall-eyed bilateral internuclear opthalmoparesis syndrome
Finally, wall-eyed bilateral INO syndrome results from a lesion affecting the bilateral MLF without involvement of the extraocular muscle nuclei. Most commonly, this presents with a lesion located between the trochlear and abducens nuclei and is typically the result of a demyelinating plaque. Clinically, this results in a failure of globe convergence in a horizontal plane and produces a characteristic divergence, or “wall-eyed,” appearance of the eyes [Figure 5].
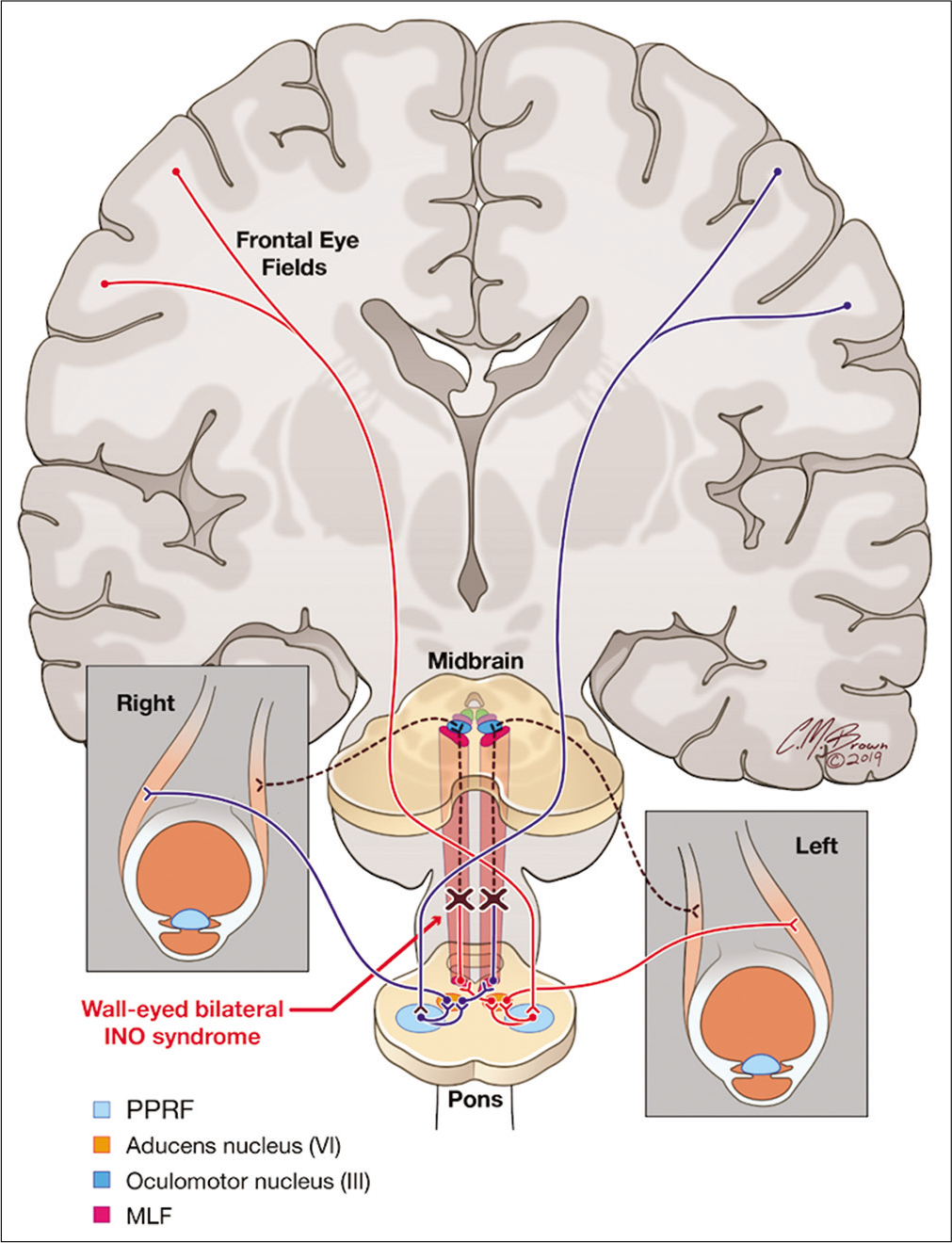
- A lesion located in the dorsal brainstem affecting the bilateral medial longitudinal fasciculus with sparing of the extraocular muscle nuclei. Clinically, this presents with divergence, or “wall-eyed” appearance, of the globes in the horizontal plane.
MLF-associated dizziness
Aside from the neural pathways responsible for synchronized, horizontal gaze, a VOR runs in the MLF that is responsible for keeping a fixed gaze during head movement. The semicircular canals drive the rotational VOR component. With head rotation, the semicircular canals are activated which transmit the neural signal through the vestibular nerve to the vestibular nuclei in the brainstem. These fibers decussate to the contralateral abducens nuclei, where one neural pathway activates the lateral rectus muscle and a second pathway travels in the MLF to the oculomotor nuclei to activate the medial rectus muscle. This helps allow an image to maintain fixed on the retina during head rotation. Similarly, the translational VOR component is mediated by the otoliths in the inner ear and mediate horizontal eye position during linear acceleration [Figure 6].[8,9]

- A 63-year-old male presented with diplopia, dizziness, and right internuclear ophthalmoplegia. Diffusion-weighted sequence (a) with corresponding attenuation diffusion coefficient map (b) demonstrating focal water restriction in the right dorsal pons of the medial longitudinal fasciculus (arrows) consistent with a small acute infarct.
MLF PATHOLOGY AND IMAGING FINDINGS
The most common causative pathology affecting the MLF is cerebrovascular accident (CVA) and primary demyelination typically related to multiple sclerosis (MS).[10] Less common etiologies include lesions related to tumor, infection, and post-traumatic injury; however, these are relatively rare causes.[11]
CVA is regarded as the most common cause for an MLF lesion in older adults (pearls) with typical age of onset of 62– 66 years. Arterial vascular supply of the MLF in the dorsal tegmentum of the midbrain is supplied by small perforating branches of the P2 segment of the posterior cerebral artery. The MLF in the dorsal pons is supplied by small, perforating paramedian arteries that arise from the basilar artery. An isolated CVA in the MLF is a relatively rare finding.[12,13] Small embolic events, hypertensive stroke, vascular dissection, and vasculitides may all be responsible for a CVA affecting the MLF. CVA in the MLF is best depicted on brain MRI using diffusion-weighted imaging as an area of water restriction related to cytotoxic edema in the MLF. Depending on the age of the ischemic event, a CVA in the MLF may also be visualized on T2-weighted and FLAIR sequences [Figure 7].

- A 57-year-old male presented with multifocal embolic stroke. Diffusion-weighted sequence (a) with corresponding attenuation diffusion coefficient map and (b) demonstrating a small, foci of water restriction in the right inferior midbrain consistent with an acute infarct of the medial longitudinal fasciculus (arrows). Diffusion-weighted sequence at the level of the lateral ventricles (c) demonstrating two additional foci of acute ischemic change in the left caudate and splenium of the corpus callosum (arrows).
Multiple sclerosis constitutes the second most common cause of a lesion in the MLF and is overall the most common cause in younger patients (<45 years old).[14] A demyelinating plaque related to MS may involve any portion of the MLF and is more commonly bilateral.[14,15] Brain MRI is the primary method to evaluate the remitting/relapsing course of MS as demonstrated by the change in white matter plaques in space and time. While patients often present with the typical inflammatory plaques spreading along the perpendicular-oriented, deep medullary veins in the periventricular white matter (Dawson’s fingers), a demyelinating plaque may also present in isolation in the brainstem. Primary demyelinating plaques are best depicted on brain MRI using T2-weighted and FLAIR sequences [Figure 8]. Intravenous gadolinium may be utilized to depict a leading edge of enhancement related to blood brain barrier breakdown from active and ongoing inflammation [Figure 9].

- A 38-year-old female presented with dizziness and weakness, without extraocular muscle dysfunction. Axial T2-weighted (a) and FLAIR sequence (b) demonstrating a small, focal demyelinating plaque in the left dorsal pons (arrows). Sagittal FLAIR sequence (c) demonstrating the characteristic periventricular appearance of whiter matter plaques in a patient with multiple sclerosis (arrows).

- A 44-year-old female with a known clinical history of multiple sclerosis presented with bilateral internuclear ophthalmoplegia. Axial FLAIR sequence (a) demonstrates a lesion in the dorsal pons in the medial longitudinal fasciculus (arrow). Axial diffusion-weighted imaging sequence (b) demonstrates no restricted diffusion (arrows) to suggest an acute infact. Axial and sagittal post-contrast T1 axial images (c and d) demonstrate solid enhancement in this location (arrows).
CONCLUSION
Lesions affecting the MLF are most commonly related to CVA or a demyelinating plaque and classically present with INO. However, depending on location, an MLF lesion may affect the adjacent extraocular muscle nuclei or the VOR producing more variable clinical symptoms than typically seen. Hence, a familiarity with the neuroanatomy of the MLF and subsequent spectrum of clinical symptoms is necessary for appropriate clinical management and screening for potential causative pathology.
Acknowledgments
We would like to thank Chris Brown for the illustrations for our research project.
Declaration of patient consent
Institutional Review Board permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Brainstem pathways for horizontal eye movement: Pathologic correlation with MR imaging. Radiographics. 2013;33:47-59.
- [CrossRef] [PubMed] [Google Scholar]
- Pearls and oy-sters: The medial longitudinal fasciculus in ocular motor physiology. Neurology. 2008;70:e57-67.
- [CrossRef] [PubMed] [Google Scholar]
- Wall-eyed bilateral internuclear ophthalmoplegia from lesions at different levels in the brainstem. J Neuroophthalmol. 2007;27:9-15.
- [CrossRef] [PubMed] [Google Scholar]
- MRI characteristics of the MLF in MS patients with chronic internuclear ophthalmoparesis. Neurology. 2001;57:762-8.
- [CrossRef] [PubMed] [Google Scholar]
- Internuclear ophthalmoplegia, I. Saccades and dissociated nystagmus. Arch Neurol. 1978;35:484-9.
- [CrossRef] [PubMed] [Google Scholar]
- Vestibular nuclei: Afferent and efferent projections In: Pompeiano O, Allum JH, eds. Vestibulospinal Control of Posture and Locomotion. Vol 76. Netherlands: Elsevier; 1988. p. :5-15. Ch. 1
- [CrossRef] [Google Scholar]
- Vertical vestibulo-ocular reflex, smooth pursuit and eye-head tracking dysfunction in internuclear ophthalmoplegia. Brain. 1988;111:1299-317.
- [CrossRef] [PubMed] [Google Scholar]
- Internuclear ophthalmoplegia: MR-anatomic correlation. AJNR Am J Neuroradiol. 1987;8:243-7.
- [Google Scholar]
- Vestibulo-ocular reflex pathways in internuclear ophthalmoplegia. Ann Neurol. 1999;45:529-33.
- [CrossRef] [Google Scholar]
- Basic and Clinical Science Course (BCSC): Neuro-ophthalmology (1st ed). San Francisco, CA: American Academy of Opthalmology; 2014.
- [Google Scholar]
- Internuclear ophthalmoplegia: Unusual causes in 114 of 410 patients. Arch Neurol. 2005;62:714-7.
- [CrossRef] [PubMed] [Google Scholar]
- Internuclear ophthalmoplegia as an isolated or predominant symptom of brainstem infarction. Neurology. 2004;62:1491-6.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated medial longitudinal fasciculus syndrome due to small midbrain infarction. Neurol Clin Neurosci. 2014;2:112-3.
- [CrossRef] [Google Scholar]
- Clinical and oculographic examinations of saccadic eye movements in the diagnosis of multiple sclerosis. Arch Neurol. 1986;43:438-43.
- [CrossRef] [PubMed] [Google Scholar]
- Internuclear ophthalmoplegia: Causes and long-term follow-up in 65 patients. Acta Neurol Scand. 2004;110:161-5.
- [CrossRef] [PubMed] [Google Scholar]






