Translate this page into:
Aggressive Form of Cherubism
Address for correspondence: Dr. G. Siva Prasad Reddy, Department of Oral and Maxillofacial Surgery, Panineeya Institute of Dental Sciences, Road No. 5, Kamala Nagar, Dilsukhnagar, Hyderabad – 500 060, Andhra Pradesh, India. gspreddy@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Cherubism is a rare non-neoplastic hereditary disease related to genetic mutations characterized by symmetrically swollen cheeks, particularly over the angles of the mandible, and an upward turning of the eyes. The affected mandible and maxilla begin to swell in early childhood, and gradually increase until the age of puberty. Apparently, surgical intervention is unnecessary unless significant functional, esthetic, or emotional disturbances develop. In the present paper, we report a case of cherubism, with classic features that was classified as grade 3, managed with surgery and followed up for 2-years after treatment.
Keywords
Cherubism
hereditary multilocular cystic lesion
non-neoplastic lesion
INTRODUCTION

Cherubism is an inherited, fibro-osseous condition characterized by firm, painless swelling of the jaws, and was first described by Jones in 1933.[1] Cherubism is usually diagnosed in the first decade of life. Clinically cherubism is characterized by fullness of the cheeks and jaw bones that results in a round face with retraction of the lower eyelids and exposure of the sclera below the irises; the “raised- to- heaven look” produced is suggestive of a cherub and gave rise to the name of this condition. The radiographical appearance is characterized by bilateral, multilocular radiolucent lesions, which often begin near the angle of the mandible and spread to the ramus and body of the mandible. Expanding maxillary lesions can result in obliteration of maxillary sinuses. The presence of eosinophilic, collagenous material around small capillaries in histopatholgical sections is of value in the diagnosis of cherubism.[2]
CASE REPORT
A 25-year-old male patient of non-consanguineous parents reported to our department with a complaint of bilateral painless swelling of both jaws. The patient was apparently asymptomatic till 8 years of age. Later he noticed progressive increase in the swelling in his jaws which continued till it attained the present size. The size of the swelling had been stable for the past year and had not regressed or increased. On extra-oral examination, the swellings appeared ovoid in shape, with well-defined borders. The swelling was more prominent in the parasymphysis and body of the mandible and molar regions. Eyes were upturned with sclera visible below the iris giving an “eye raised to heaven” appearance. There was a difference in the ocular levels, right eye being at a slightly higher level [Figure 1]. Intra-oral examination revealed multiple missing teeth in maxilla and mandible. Obliteration of buccal sulcus of mandible was noticed in the molar regions. In the maxilla multiple swellings were seen, which were hard, sessile, non-tender, and covered with pink mucosa.

- Extra-orally the swellings appeared ovoid in shape, with well-defined borders.
Radiographical features
The orthopantamograph revealed multiple impacted teeth in the mandible, with multiloculated osteolytic lesions involving the entire body as well as the ramus of the mandible sparing the condyles [Figure 2]. A 3-dimensional computed tomography showed multiloculated cystic lesions affecting the body and rami of the mandible and also the maxilla. Both the orbital floors were seen to be raised. The lesion caused marked expansion of the bones, with a multifocal cortical breakthrough [Figure 3].
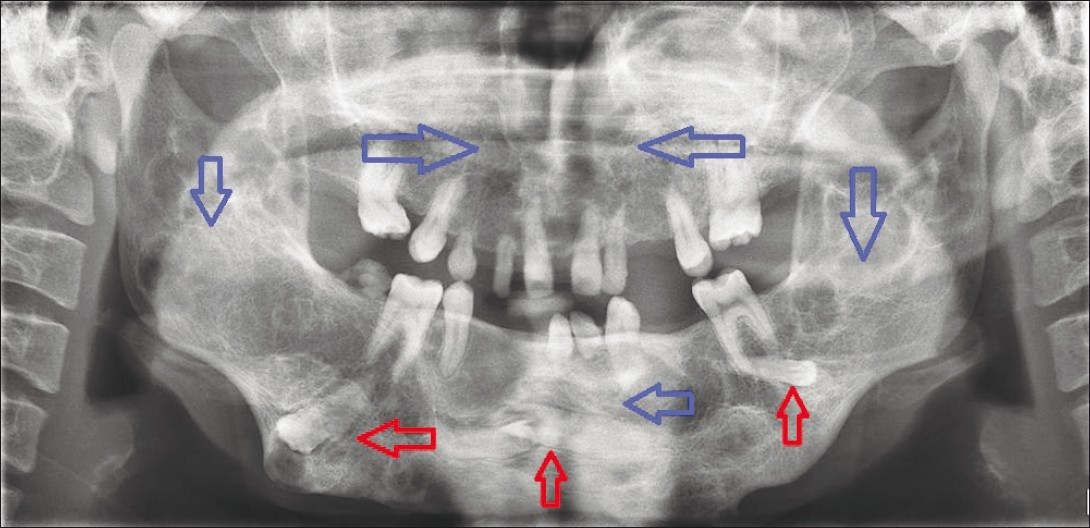
- The orthopantamograph revealed multiple impacted teeth in the mandilble (red arrows) with multiloculated osteolytic lesions involving mandible and maxilla (blue arrows).

- 3-Dimensional computed tomography scan showing multiloculated cystic lesions affecting the body and rami of the mandible (blue arrows) and maxilla with raised orbital floor (red arrows).
Histopathology
Biopsy to obtain specimen from both the jaws in the alveolar region was performed under local anesthesia.Microscopy revealed highly cellular stroma with many multinucleated giant cells. The cellular stroma showed spindle cell fibroblasts with vesicular nuclei arranged in fascicles, whorled pattern and irregularly in few areas. The giant cells were unequally distributed and were of different sizes with varied number of nuclei resembling osteoclasts. There were few blood vessels and areas of extravasated blood and minimal amount of collagen was seen. There was no evidence of atypia [Figure 4].

- Microscopy revealed highly cellular stroma consisting of plenty of multinucleated giant cells (black arrow). The cellular stroma consists of spindle cell fibroblasts with vesicular nuclei arranged in fascicles (blue arrow).
Surgery
The grotesque appearance and the parent's insistence on esthetic improvement compelled the surgeon to attempt cosmetic surgical recontouring of the jaws under general anaesthesia. The entire mandible and maxilla was degloved intraorally. The exposed lesion tissue consisted of multiple locules with reddish hue and semi-hard consistency. Buccal surfaces of maxilla and mandible were decorticated and curetted as much as possible to provide optimal cosmetic improvement. Impacted and loose teeth were removed. Specimen was sent for final histopathological examination [Figure 5]. The diagnosis of cherubism was confirmed. Patient had no recurrence of the lesion during the 2-year follow-up period [Figure 6].

- Surgical specimen showing decorticated and curetted material along with impacted teeth.

- Two-year postoperative follow-up photograph with acceptable esthetics.
DISCUSSION
The pathogenesis of cherubism remains controversial. No cause and effect relationship with trauma, infection, or hemorrhage has ever been verified. Anderson suggested that a genetically induced biochemical abnormality stimulates the giant cell lesions characteristic of cherubism. A molecular pathogenesis of cherubism has been proposed; SH3BP2 gene mutations cause dysregulation of the Msx-1 gene, which is involved in regulating mesenchymal interaction in craniofacial morphogenesis.[3]
Affected children appear normal at birth. Bilateral swellings tend to occur between 2 and 4 years of age. Males tend to be affected twice as often as females. In our case, the disease manifested itself in the first decade, at 8 years of age. Clinically the lesion of cherubism produces painless, typically slow expansion of the affected area of jaw. The facial expansion maybe quite mild or may result in considerable deformity. More extensive involvement may result in enlargement and widening of the alveolar bone. The bony expansion is firm and non tender to intraoral palpation. Maxilla is less commonly involved than the mandible. But involvement of the anterior maxillary segment produces one of the most characteristic deformities. Progressive involvement of the anterior maxillary segment bone stretches the skin and the lower eyelid beneath the orbit, exposing the lower sclera. This results in the patient's eyes appearing to constantly gaze upward. The palatal vault may also be reduced due to the expansion of the maxilla. The developing permanent teeth in the areas of involvement may be displaced, malformed, or absent. Regional lymphadenopathy is also a common finding.[4] History, clinical course, and the findings in our case corresponds to the classic features of cherubism.
Cherubism is usually recognized radiographically between 18 months and 2 years of age. The bilateral progressive bony changes are classic for the condition. Irregular, multilocular, well-defined, translucent, cystic spaces causing expansion of bone and sparing only a thin layer of cortex are usually seen. The cortex may be perforated. The teeth may be displaced, unerupted, or appear to be floating in the cyst-like spaces. In the mandible, the inferior alveolar canal maybe displaced and lesion may involve the alveolar process, the angle and ramus. It may advance toward the incisors and obliterate the sigmoid notch, but the condyles may be spared. Periosteal new bone formation is never present. In the maxilla the lesion is similar and is mainly found in the maxillary tuberosities and adjacent alveolar bone. The maxillary antra may be completely obliterated only to become normally pneumatized as the lesion regress.[5]
Seward and Hankey have proposed a grading system based on the radiographical location of the lesions in the jaws. It is as follows:
Grade 1: Involvement of bilateral mandibular molar regions and ascending rami, mandible body, or mentis.
Grade 2: Involvement of bilateral maxillary tuberosities (in addition to grade 1 lesions) and diffuse mandibular involvement.
Grade 3: Massive involvement of the entire maxilla and mandible, except the condyles.
Grade 4: Involvement of both jaws, including the condyles. According to Ramon and Engelberg grade 4 lesions not only push the orbital floor upward but also penetrate it.[6]
Our case could possibly be classified as above grade 3 cherubism as there was huge deformity of the mandible, especially the bilateral posterolaterosuperior extension of maxillary lesions with slight elevation of orbital floor. The lesions of cherubism are not distinctive histologically and are difficult to differentiate from other giant cells containing fibro-osseous lesions, making diagnosis dependent on the clinical findings impossible. Numerous investigators have observed the presence of eosinophilic material around small capillaries. Hamner histochemically demonstrated this perivascular cuffing to be collagen protein and felt its presence was of value in the diagnosis of cherubism.[7]
Treatment of cherubism has not been standardized. Surgical treatment appears to be unnecessary for grade 1 and 2 cases, in the absence of secondary disturbances. Curettage appears to be necessary in more aggressive cases (grade 3), to reduce maxillofacial deformity that occurs after puberty. Dukart et al., found that surgical curettage and recontouring performed during a period of rapid growth of cherubism lesions not only offer a favorable immediate result but also arrests active growth of remnant lesions while stimulating bone regeneration.[8] Calcitonin therapy seemed to be effective and resulted in remission of the lesion. The administration of calcitonin was done with nasal spray instead of by subcutaneous injections. The rationale of calcitonin administration is that it inhibits the osteoclastic activity of the giant cells.[9] Radiation therapy is ineffective and contraindicated in view of the risk of osteoradionecrosis, interference with dentofacial growth and development, and the effect on future surgical procedure.[10]
In our case, the patient was an adolescent affected psychologically by his grotesque appearance, which was also a concern for his parents. Therefore, a conservative surgical curettage and recontouring of the jaws was performed under general anesthesia to address his esthetic concern. Two years of postoperative follow-up showed a sustained esthetic improvement achieved by surgery of the grade 3 lesion. There was a radical improvement in the patient's psychological and behavioral problems.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/8/93275
REFERENCES
- Novel mutation in the gene encoding c-Abl-binding protein SH3BP2 causes cherubism. Am J Med Genet A. 2003;121A:37-40.
- [Google Scholar]
- Oral and Maxillofacial Surgery: Surgical Pathology. Vol 5. Philadelphia: Saunders; 2000.
- [Google Scholar]
- The demonstration of perivascular collagen deposition in cherubism. Oral Surg Oral Med Oral Pathol. 1969;27:129-41.
- [Google Scholar]
- Cherubism treated with Calcitonin: Report of a Case. In: J Oral Maxillofac Surg. Vol 65. 2007. p. :1665-7.
- [Google Scholar]
- Cherubism: A Study of twenty cases from one family. Oral Surg Oral Med Oral Pathol. 1979;47:307-11.
- [Google Scholar]






