Translate this page into:
Adherence of Academic Radiologists in a Non-English Speaking Imaging Center to the BI-RADS Standards of Reporting Breast MRI
Address for correspondence: Dr. Sepideh Sefidbakht, Maaliabad, 35 Metri Doostan, Borje Anjelose 1, No. 104, Postal Code: 71877-15449, Shiraz, Iran. E-mail: sepidehsefidbakht@yahoo.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives:
To assess the adherence of academic radiologists in a university center to BI-RADS lexicon (BLA) and to evaluate the structural completeness of breast MRI reports.
Materials and Methods:
Breast MRI reports made during 2012 in a single academic center by six readers were scored for formal completeness (FS) including recording the MRI protocol, making relevant clinical correlation, and describing background enhancement; BLA including mass rather than lesion, describing lesion outline, enhancement characteristics, and dynamic curve; and also expressing the final conclusion using BLA, resulting in a maximal total score of 8. FS and BLA were correlated with reader characteristics including breast imaging background, years of academic experience, and number of breast MRIs reported yearly. Tests used for statistical analysis were the Mann–Whitney U test and analysis of variance (ANOVA).
Results:
Overall BLA was 38.9%. This percentage was 60.1% and 3.7% in radiologists with and without breast imaging background, respectively (P = 0.000). Mean FS among all readers was 3.81 ± 1.75. This score was 2.54 ± 1.1 for readers without breast imaging background and 4.6 ± 1.6 for the readers regularly involved in breast imaging (P = 0.000).
Conclusions:
Higher degree of BLA and higher mean FS were associated with radiologists regularly involved in breast imaging. No association was found with years of academic experience or number of breast MRIs interpreted yearly.
Keywords
Radiology report
breast MRI
BI-RADS standards
INTRODUCTION
Radiology reports represent the final outcome and the interface of a Radiology Department. Worldwide, referring physicians are becoming increasingly demanding in terms of their expectations of diagnostic accuracy, clarity, and timeliness of radiology reports.[12] In working environments where general radiologists handle various subspecialty imaging, coping with the ever-increasing requirements can become a challenging undertaking.
Content and structure of radiology reports have been evaluated occasionally.[345] Various reporting standards have been developed to ensure accurate communication of the imaging findings and interpretation of the images to the clinician.[6] The BI-RADS lexicon is among the most widely practiced and time-honored reporting guidelines worldwide.[7] This lexicon has proven most beneficial in providing clarity and consistency and to ensure proper management of the patients. The purpose of this study is to determine the degree of adherence of academic radiologists in a university center in a non-English speaking society to the BI-RADS standards of reporting breast MRI.
In addition, we also subjectively assigned a scoring system to the evaluated reports for various structural and formal indicators including adherence to BI-RADS lexicon, mentioning the MRI protocol, as well as correlation made with clinical indication and additional imaging. We correlated the formal reporting scoring system thus designed with years of experience of the radiologist as well as the number of breast MRI studies interpreted yearly, and whether the radiologists were also involved in breast imaging in general or interpreted the images as MRI experts without additional involvement in breast imaging. The final objective was to evaluate the present degree of standardization of breast MRI reports and to evaluate the factors that favorably influence consistency of the reports.
MATERIALS AND METHODS
Our University Ethics Committee approved this retrospective blind study. We evaluated all available breast MRI reports during 24 months from January 2011 to December 2012, reported by six different radiologists. The reports were evaluated for adherence to BI-RADS lexicon, including using terms of mass rather than lesion or nodule, including descriptive characteristics including mass shape and margin, and also describing background enhancement.
Also, the reports were evaluated and scored for additional structural elements including mentioning the protocol, using the BI-RADS system for communicating the conclusion and for making relevant correlation with clinical and other imaging data. An overall score was assigned to each report by adding up one score for each of the above-mentioned items (maximal total score of 8).
Mann–Whitney U test was used to compare the formal scores and adherence to BI-RADS lexicon with breast imaging background, years of experience in MRI, years of experience in breast imaging, and the number of yearly interpreted breast MRIs for each reader.
Analysis of variance (ANOVA) was used to compare adherence to the various items of the formal scoring system, as well as the total score with reader background. P values less than 0.05 were considered significant. All statistical analyses were done using Software Package for Statistical Analysis (SPSS) version 11.5.
RESULTS
Computerized search produced a total of 74 breast MRI reports, dictated by six different readers, all general radiologists. Four out of the six readers, with 3–5 years of experience in interpreting MRI images and 9–11 years of experience as general radiologists, were also regularly involved in breast imaging (mean number of mammograms interpreted yearly = 3500). They were also involved in breast ultrasound with a mean of 500 breast ultrasounds performed yearly. The readers with breast imaging background reported 63.4% of the images.
The two other readers, with 7 and 8 years of experience in interpretation of MR images and 12 and 13 years experience as general radiologists, respectively, were not involved in any form of breast imaging other than MRI. They interpreted 36.6% of the studies [Table 1].
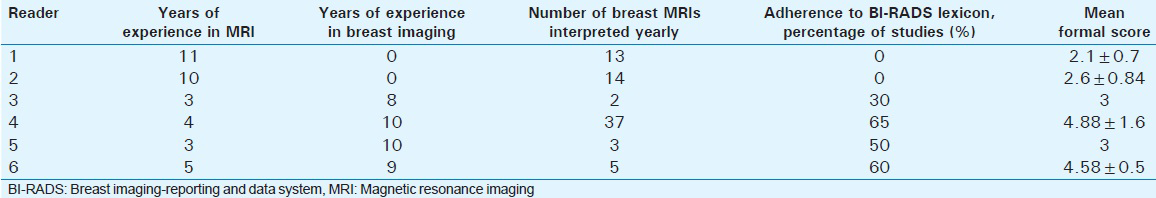
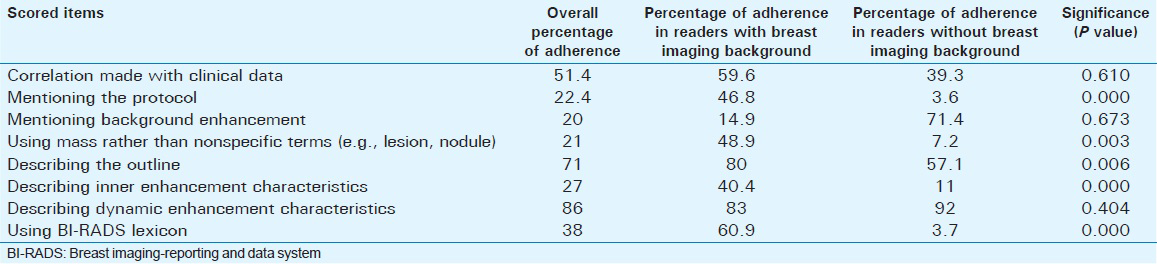
Overall percentage of adherence to BI-RADS lexicon among the studies was 39.4%; this percentage was 59.8% in readers with and 3.4% in readers without regular involvement in breast imaging. The formal scores were calculated by adding up one score for each of the following items: Mentioning the protocol, mentioning clinical indication and correlating with additional breast imaging, mentioning background enhancement, using BI-RADS lexicon terms, including mass rather than nonspecific terms (e.g., lesion or nodule), describing the outline and dynamic characteristics, and also using BI-RADS lexicon for final conclusion.
Mean total formal score among all readers was 3.79 ± 1.74. This score was 2.4 ± 1.02 in readers without breast imaging background and 4.63 ± 1.58 for the readers regularly involved in breast imaging (P = 0.000).
Most frequent indications for requesting the studies included known malignancy, to rule out multifocal disease, status post operation for ruling out possible recurrent tumor, and further evaluation of abnormal mammogram (39.2% of the studies).
No statistically significant correlation was found between the mean formal scores and years of MRI or academic experience (P = 0.057). In contrast, having a breast imaging background was significantly related to higher formal scores and BI-RADS lexicon utilization (P = 0.000). Various items of the scoring system were correlated with presence of breast imaging background. The results are summarized in Table 2.
DISCUSSION
In this series, the degree of adherence to BI-RADS lexicon was far from perfect (38.9%). There have been inconsistencies in using the BI-RADS lexicon reported before;[8] however, unlike Baker et al., who stressed inter-observer variability in interpretation, we found significant non-adherence to the lexicon. Also, other items recommended in ACR guidelines, including mentioning the protocol and clinical correlation, were suboptimally adhered to (29.7% and 45.9%, respectively).
Inadequacies in the quality of radiology reports have been reported before, with both structural and content flaws stressed in previous studies.[39] This has resulted in many attempts to further improve the quality and standardize radiology reporting systems.[101112] In a study conducted in the Netherlands and Flanders, the authors evaluated abdominal CT scan reports for length and various structural and formal elements including technical information, describing the findings, and including a conclusion, recommendation, and also a note section. Unlike our study, this was an evaluation of abdominal CT scan reports, for which a formal reporting system similar to BI-RADS is not present. They assessed the length and structural completeness of the report and found statistically significant differences between countries and also between staff members and residents.[8]
To our knowledge, no study has been conducted to evaluate the structure of radiology reports in this part of the world. We are basically a non-English speaking country with a tradition of English communication among the medical society in one imaging center. Readers participating in this study are general radiologists, all with additional MRI fellowship training. Like in many other countries, they receive no formal training in reporting, but pick up as much as possible with apprenticeship model during their own residency and fellowship training. Thus, they had similar qualifications overall, but different lengths of experience as academic radiologists. According to our findings, there was no correlation between years of academic experience or years of MRI experience with the formal and structural completeness of the reports or with adherence to the BI-RADS lexicon. The major reader characteristic correlating to the report quality was regular involvement in breast imaging, in general.
To select the items included in our scoring system, we used the ACR practice guideline for communication of diagnostic imaging findings (2010) as a basic template.[6] Correspondingly, we scored technical description of the MRI procedure performed. For description of the findings, we included adherence to BI-RADS lexicon as four separate items including description of lesion shape and outline, inner enhancement, and dynamic characteristics. We also included clinical correlation as an independent item. Based on ACR practice guidelines, the reports should also be concluded with an impression section; corresponding to this item, we scored adherence to BI-RADS lexicon as a widely accepted standard.
Due to widely accepted standardization and guidelines, breast MRI reports were a convenient choice for evaluation of report quality. We also considered breast MRI reports a good representative of a situation in which subspecialty imaging has to be somehow tackled with general radiologists. To the best of our knowledge, no study has been performed to assess the degree of adherence to BI-RADS lexicon in countries where its utilization is not a legal requirement.
Limitations
Our study has a few significant limitations, however. We evaluated readers from one single academic center with reporting and communication tradition dissimilar to other centers in the country. We also did not evaluate the reports for diagnostic accuracy, which limits any conclusion on the overall quality of the reports. As far as we know, despite attempts to design quality assurance systems for radiology systems, there is no formal assessment of radiologist accuracy elsewhere either. We thus report on the structure and form of the reports, and not on the general quality.
CONCLUSION
This study underscores the need for further standardization in countries like ours where it is not yet practiced widely. Based on our findings, it might be concluded that in the working environments where it is not feasible to limit privilege of breast MRI reporting to subspecialty-trained radiologists in the near future, having an additional breast imaging background can be an acceptable and practical prerequisite for interpreting breast MRIs. In our study, the readers involved in breast imaging, in general, described the lesion outline, inner enhancement characteristics, mentioned the MR protocol completely, and used the BI-RADS lexicon in their reports significantly more often [Table 2]. There was no significant difference in description of the dynamic enhancement characteristics of lesions between the two groups of radiologists with and without breast imaging background.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Dr. Ravanfar for her kind assistance.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2015/5/1/66/172970
REFERENCES
- Radiology report turnaround: Expectations and solutions. Eur Radiol. 2008;18:1326-8.
- [Google Scholar]
- The clinical impact of the radiology report in wheezing and nonwheezing febrile children: A survey of clinicians. Pediatr Radiol. 2009;39:348-53.
- [Google Scholar]
- Evaluation of the quality of radiology requisitions for intensive care unit patients. Acad Radiol. 2006;13:236-40.
- [Google Scholar]
- A new method of evaluating the quality of radiology reports. Acad Radiol. 2006;13:241-8.
- [Google Scholar]
- The ACR practice guideline for communication of diagnostic imaging findings. (Revised 2010, Resolution 11) Reston, VA: American College of Radiology; 2010. p. :1-6.
- [Google Scholar]
- ACR BI-RADS® Magnetic Resonance Imaging. In: ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System. Reston, VA: American College of Radiology; 2013.
- [Google Scholar]
- Breast imaging reporting and data system standardized mammography lexicon: Observer variability in lesion description. AJR Am J Roentgenol. 1996;166:773-8.
- [Google Scholar]
- Structure and content of radiology reports, a quantitative and qualitative study in eight medical centers. Eur J Radiol. 2009;72:354-8.
- [Google Scholar]
- Improving the quality of radiology reporting: A physician survey to define the target. J Am Coll Radiol. 2004;1:497-505.
- [Google Scholar]
- Quality - A radiology imperative: Interpretation accuracy and pertinence. J Am Coll Radiol. 2007;4:162-5.
- [Google Scholar]






