Adenomatoid Odontogenic Tumor – A Report of Two Cases with Histopathology Correlation
Address for correspondence: Dr. Pavitra Baskaran, Department of Oral Medicine and Radiology, SRM Kattankulathur Dental College, Potheri, Kanchipuram Dist., Tamil Nadu, India. E-mail: pavitra_omed@yahoo.in
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Adenomatoid odontogenic tumor (AOT) is an uncommon, hamartomatous, benign, epithelial lesion of odontogenic origin that was first described by Driebaldt in 1907, as a pseudo-adenoameloblastoma. The current World Health Organisation (WHO) classification of odontogenic tumors defines AOT as being composed of the odontogenic epithelium in a variety of histoarchitectural patterns, embedded in mature connective tissue stroma, and characterized by slow, but progressive growth. The current article reports two cases with different presentations; first in a young female patient and the second in a middle-aged male patient. The importance of biopsy, which is the gold standard for diagnosis, and its use in planning of the treatment is discussed.
Keywords
AOT
odontogenic
pseudo-adenoameloblastoma
INTRODUCTION

Adenomatoid odontogenic tumor (AOT) is a benign tumor of odontogenic origin. It was first described by Dreibaldt in 1907, as a pseudo-adenoameloblastoma and first reported by Harbitz (1915) as a cystic adamantinoma. Philpsen and Birn (1971) proposed the widely accepted and currently used name, adenomatoid odontogenic tumor.[1]
Adenomatoid odontogenic tumor is also called ‘two-thirds tumor,’ because 2/3rd of adenomatoid tumors occur in the maxilla, 2/3rd occur in young females, two-thirds of the cases are associated with un-erupted teeth, and two-thirds of the affected teeth are canines.[2]
AOT constitutes about 2.2 – 7.1% of the odontogenic tumors. The number of reported cases has increased in recent times probably due to the increased incidence of the tumor.[3] This case report highlights the varied clinical and radiological features of AOT.
CASE REPORTS
Case 1
A 15-year-old female patient presented to our Institution with a swelling on her upper left jaw in the region of the front teeth that had persisted for a year. The swelling had gradually increased in size. There was no associated pain.
Extra-oral, physical examination revealed a single diffuse swelling in the left anterior maxillary region measuring about 3 cm × 4 cm in size. On palpation, the swelling was hard and non-tender. On intra-oral examination, a single, well-circumscribed swelling with a smooth surface was present in the buccal and palatal aspect of the left upper anterior maxillary region [Figure 1], resulting in obliteration of the buccal vestibule. Deciduous left maxillary lateral incisor and canine teeth were present. The permanent maxillary left lateral incisor and canine teeth were missing. Bicortical expansion was also present.

- Intraoral view showing the buccal aspect of the swelling.
The intra-oral peri-apical radiograph of the left maxillary anterior region and an orthopantomaograph (OPG) revealed a well-circumscribed unilocular radiolucency in relation to the left maxillary incisor to first premolar region associated with an impacted left maxillary lateral incisor and mesially displaced root of the left maxillary central incisor, in addition, specks of calcification in the radiolucent area were present. An impacted left maxillary canine tooth was seen in the left maxillary first molar region on the OPG [Figures 2 and 3] .
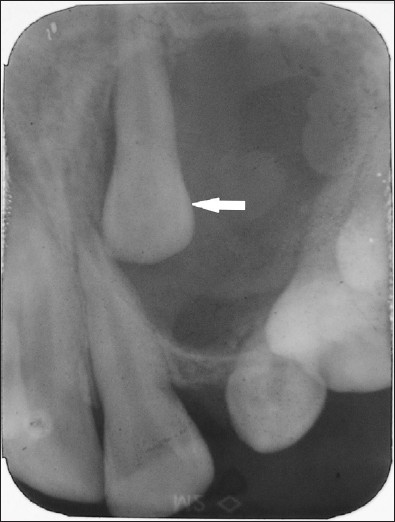
- Intraoral periapical radiograph of maxillary left incisor to canine region reveals unilocular radiolucency with impacted maxillary lateral incisor on the left side (arrow).
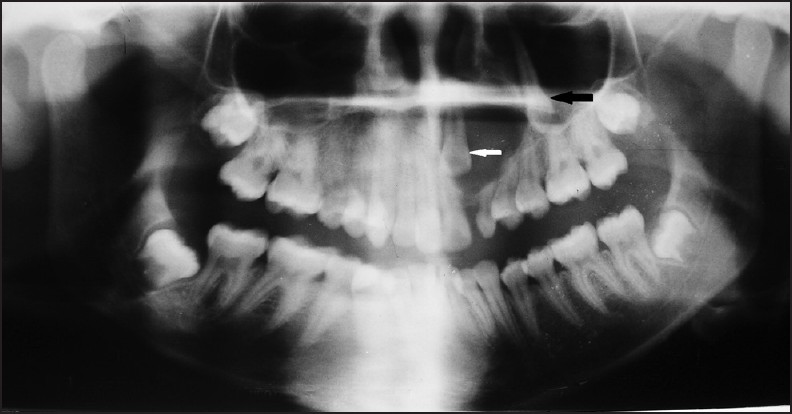
- An orthopantomograph (OPG) reveals unilocular radiolucency with an impacted left maxillary lateral incisor (white arrow) and displaced left maxillary canine (black arrow).
A provisional diagnosis of a benign bony neoplasm of odontogenic or non-odontogenic was made. The patient underwent surgical curettage under general anesthesia.
Microscopy revealed a cystic space lined by focal areas of solid tumor showing whorls, sheets, and duct-like structures [Figures 4 and 5] . The final diagnosis of intraosseous variant of AOT was obtained.
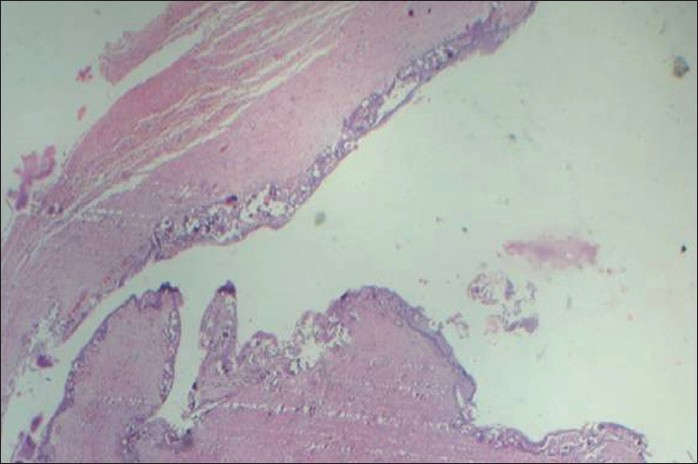
- Hemotoxylin and Eosin (4×) stained tissue exhibits a cyst lining-like epithelium made up of cuboidal epithelial cells showing encapsulation.
- Hemotoxylin and Eosin stained tissue (10)× shows whorls and sheets of cuboidal epithelial cells present in a rosette-like arrangement.
Case 2
A 34-year-old male patient came to the clinic with a swelling in the region of left upper front teeth that had developed over a period of three years. The swelling had gradually increased in size and there was no associated pain.
On physical examination, a single, diffuse swelling was present in the left anterior maxillary region, measuring 3 cm × 2 cm. There was no tenderness on palpation, the swelling was firm in consistency, the surface was smooth, and had well-defined edges.
Intra-oral examination demonstrated a mass in the left anterior maxillary region extending in both labial and palatal directions, with a bicortical expansion, resulting in obliteration of the buccal vestibule [Figure 6] . The maxillary left lateral incisor and canine teeth were slightly displaced.
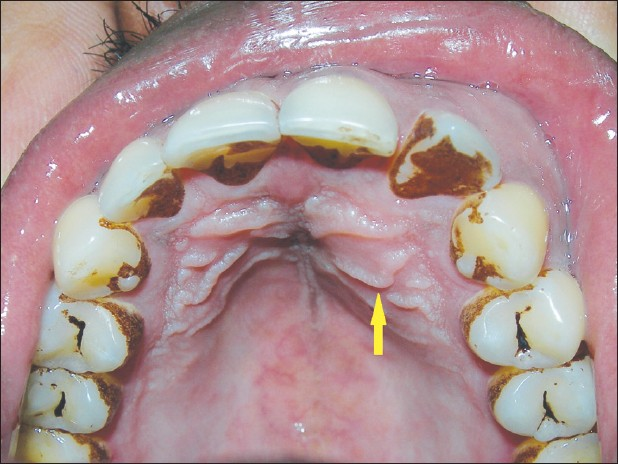
- Intraoral view demonstrates the palatal aspect of the swelling (arrow).
An intraoral periapical radiograph [Figure 7] of the left anterior maxillary region, maxillary occlusal [Figure 8] radiograph, and a panoramic radiograph [Figure 9] showed a well-defined, unilocular radiolucency, with a thin sclerotic border in the maxillary left anterior region, with displacement of maxillary left lateral incisor and canine teeth. There was an impacted supernumerary tooth in the periapical region of the maxillary central incisor that was not associated with well-defined radiolucency. There was root resorption associated with the maxillary left canine and first premolar teeth.
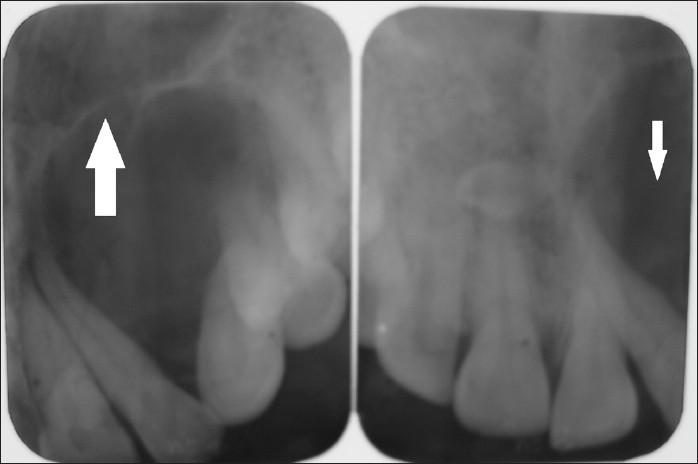
- Intraoral periapical radiograph of the region from maxillary left incisor to the canine region unilocular radiolucency with sclerotic border (white arrow).
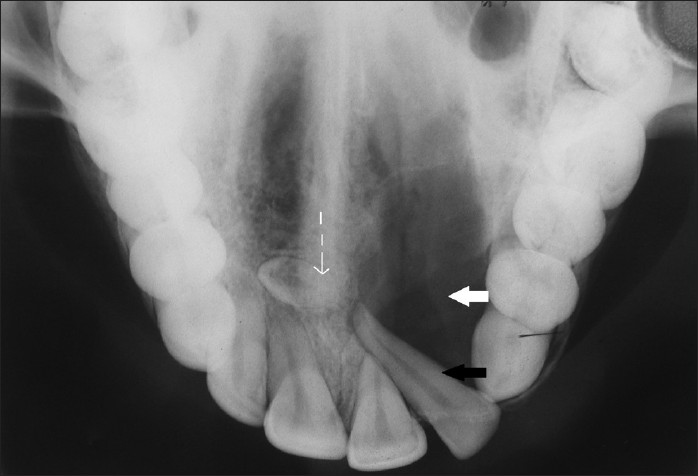
- Maxillary occlusal view reveals unilocular radiolucency with a sclerotic border in relation to the maxillary left central incisor to canine (teeth 21-23) region (white arrow), displaced maxillary left lateral incisor (tooth 22, black arrow), and presence of impacted supernumerary teeth in the midline (dashed arrow).
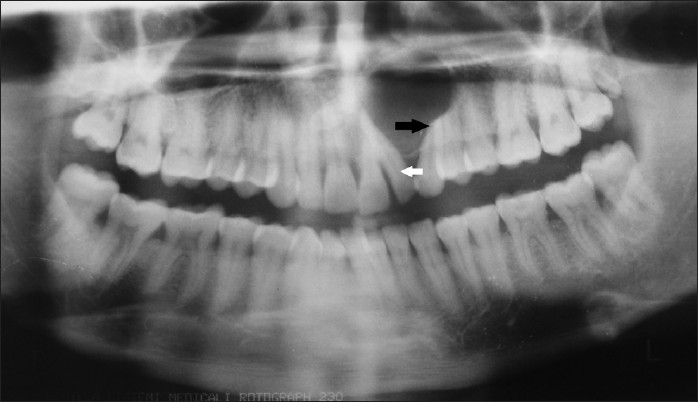
- Orthopantomograph (OPG) reveals unilocular radiolucency with an impacted supernumerary tooth in the midline, with displaced maxillary left lateral incisor (white arrow) and root resorption in the maxillary left canine and premolar (black arrow).
On the basis of the above findings, a provisional diagnosis of benign neoplasm of odontogenic or non-odontogenic origin was made.
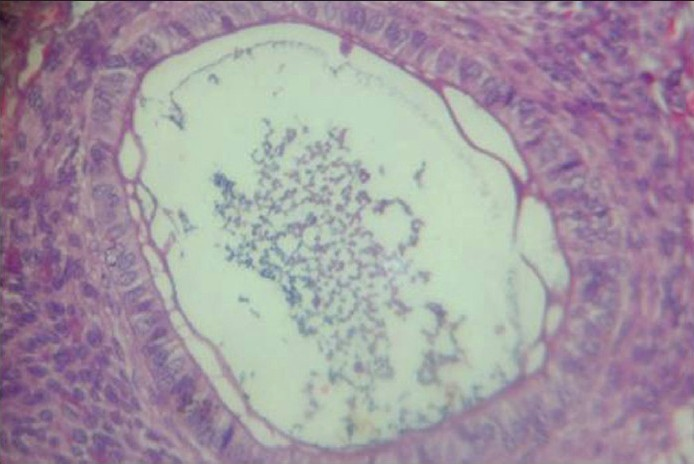
An excisional biopsy was performed under general anesthesia and the histopathology revealed whorls and sheets of cuboidal epithelial cells, which were well-encapsulated. There was evidence of duct-like structures lined by columnar cells, with the nucleus polarized away from the lumen [Figure 10] . At the periphery of the lesion, narrow anastomosing cords of epithelial cells were seen in an eosinophilic, loosely arranged matrix. There was evidence of calcifications and moderate vascularity. The above features were suggestive of adenomatoid odontogenic tumor.
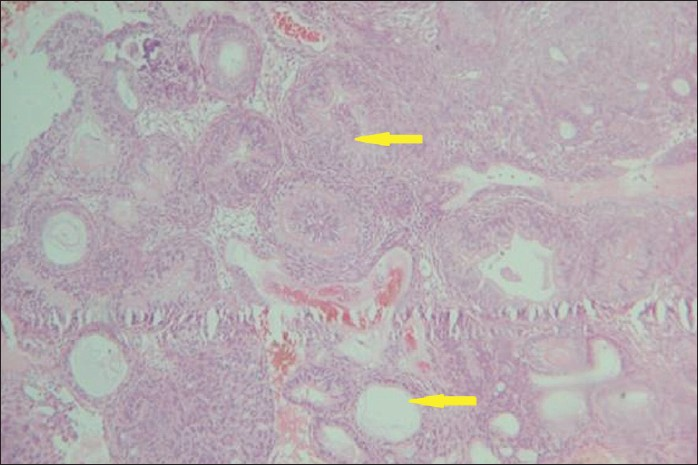
- Hematoxylin and Eosin stained tissue (10×) shows odontogenic epithelial lining arranged in a rosette, ductal, and whorling pattern (arrows).
DISCUSSION
The adenomatoid odontogenic tumor is a slow growing lesion, constituting about 3% of all odontogenic tumors followed by odontoma, periapical cemental dysplasia (Cementoma), myxoma, and ameloblastoma.[4] In a series of publications, the mean ages of all cases reported were between eight and twenty-five years, and one case reported by Baby John was 39-years old.[1] However, in our case, the age of the patient in Case 1 was 15 years, which was in concordance with all other reports, and the age in Case 2 was 34 years, which is more along the lines of Baby John's report.
Most of the cases reported in the literature were in the maxilla affecting the anterior segment and were associated with the canine tooth.[1] The cases we report here were also similar, except that in one of our cases, the tumor was associated with an impacted lateral incisor.
The origin of AOT is believed to be from an odontogenic source; the cytologic features are similar to those of the enamel organ, dental lamina, reduced enamel epithelium, and / or their remnants.[2]
AOT shows centrifugal expansion (uniform expansion in all directions). It has been hypothesized that at an early stage AOT may expand the cortical plates, which within the cancellous bone spread linearly and then later may affect the cortical plates by expansion / resorption.[5] Bicortical expansion was seen in both our patients.
AOT can occur both intraosseously and extraosseously.[2] Both the cases reported by us were of the intraosseous type. Intraosseous AOTs are characterised by a well-defined unilocular radiolucency surrounding the crown, which is often part of the root of the unerupted tooth, and follows a follicular pattern. Intraosseous type accounts for about 73% of all AOTs. The extrafollicular variant accounts for about 24% of all AOTs and presents as a unilocular radiolucency found between, above, or superimposed on the roots of erupted teeth.[4] Both our cases were of the intraosseous type, of which the first case represents the follicular variant and the second case, the extrafollicular variant.
However, radiological findings of AOT simulate many other odontogenic lesions such as dentigerous cysts, calcifying odontogenic cysts or tumor, ameloblastoma, keratocystic odontogenic tumor or periapical disease.[6] The above-mentioned lesions along with the nasiolabial cyst, nasopalatine duct cyst, and odontogenic keratocyst can be considered in the differential diagnosis of lesions occurring in the anterior maxilla. Our first case resembled a dentigerous cyst and the second one, an odontogenic keratocyst.
Minute radiopacities (califications) around the retained tooth are seen and considered characteristic, but not pathognomonic.[6] The first case in our report demonstrates radiopacities in accordance with the published reports.
The histological features of AOT show a tumor of the odontogenic epithelium, with duct-like structures, and with varying degrees of inductive changes in the connective tissue.[7] The most striking pattern is that of various sizes of solid nodules of columnar or cuboidal epithelial cells forming nests or rosette-like structures, with minimal stromal connective tissue.[8] The tumor may contain pools of amyloid-like material and globular masses of calcified material.[7] Our case is consistent with the common histological features that are reported in the literature.
The origin of the follicular variant can occur before or after cystic expansion (Cystic expansion in the jaw bone refers to the nature of expansion of the cyst through the buccal and lingual/palatal cortical plates) . If it occurred after cystic expansion, then it effectively meant that the origin was from a dentigerous cyst and several such cases have been reported.[19] If it occurred before cystic expansion, then the tumor tissue would fill the follicular space and the AOT would present as a solid tumor.[9] In case 1, the cystic lining was present, with deeper areas showing tumor islands, suggesting that the tumor could have occurred after cystic expansion.
AOT is a benign neoplasm with a low recurrence rate and can be treated successfully with enucleation and simple curettage.[1]
CONCLUSION
The cases discussed emphasize the importance of recognizing neoplasms arising in the odontogenic tissues. AOT has unique clinical, radiographic, and histopathological features. However, the clinical and radiographic features may often present similarity to those of an odontogenic cyst. Persistence of deciduous teeth for a longer duration and unerupted succeeding permanent teeth, when associated with a swelling, always need to be investigated for odontogenic lesions. For diagnosis of odontogenic lesions, conventional radiographs still play a major role in this era of advanced imaging.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/64/92186.
REFERENCES
- Mural adenoamtoid odontogenic tumor in the mandible- A rare case. Int J Oral Maxillofac Pathol. 2011;2:35-9.
- [Google Scholar]
- Adenomatoid odontogenic tumor-hamartoma or True neoplasms: A case report. J Oral Sci. 2009;51:155-9.
- [Google Scholar]
- Adenomatoid odontogenic tumor mimicking an odontogenic cyst: A case report. JIADS. 2010;1:59-64.
- [Google Scholar]
- An unusual site of adenomatoid odontogenic tumor presenting as a Periapical cyst: A rare case report. JIAOMR. 2010;22:39-41.
- [Google Scholar]
- Adenomatoid odontogenic tumor (AOT) of maxillary sinus: Case report with respect to immunohistochemical findings. In Vivo. 2009;23:111-6.
- [Google Scholar]
- Intraosseous follicular adenomatoid odontogenic tumor- A case report. Int J Dent. 2009;2009:597483.
- [Google Scholar]
- Adenomatoid odontogenic tumor (AOT) originating in a unicystic ameloblastoma: A case report. Head and Neck Pathol. 2007;1:146-9. Epub 2007 Nov 29
- [Google Scholar]






