Translate this page into:
A Very Rapid Visual Recovery of Posterior Reversible Encephalopathy Syndrome
Address for correspondence: Dr. Harpreet Walia, Department of Ophthalmology, 3445 Stratford Road Box 1106, Atlanta, GA 30326, USA. E-mail: hwalia@emory.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.

Dear Editor,
Patients with Posterior Reversible Encephalopathy Syndrome (PRES) usually present with visual disturbances along with neurotoxic manifestations. Typically, radiographic and clinical manifestations of PRES resolve within several weeks after the inciting factor has been addressed. We report a classic case of PRES in a pre-eclamptic patient with the unique feature of rapid visual recovery and typical radiographic features.
CASE PRESENTATION
A 27-year-old Afro-American woman with significant history of severe pre-eclampsia necessitating Caesarean section was referred to our ophthalmology department on the third postoperative day with complaints of blurred vision in both eyes along with a right-sided headache. First ophthalmology examination demonstrated her visual acuity limited to fingers counting in both eyes. No relative afferent pupillary defect was present. Neurologic examination was unremarkable.
A Computed Tomography (CT) scan was performed, which revealed a hypointensity within the bilateral cortical white matter involving the occipital lobes [Figure 1]. A Magnetic Resonance Imaging (MRI) of the brain revealed an abnormal T2 hyperintensity within both occipital lobes, with sparing of the calcarine and paramedian parts of the occipital lobes and the posterior aspect of the left parietal lobe [Figure 2]. The classic features of neuroimages, combined with clinical presentation of decreased vision and headache with a history of pre-eclampsia, confirmed the diagnosis of PRES.
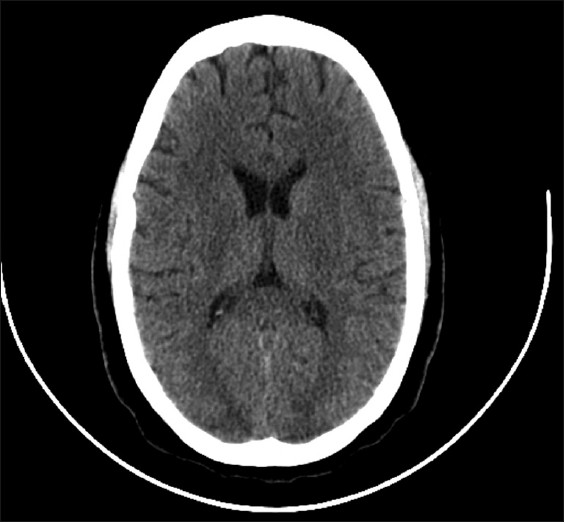
- Non- contrast axial computed tomography of the head demonstrates bilateral cortical hypointensities involving the occipital lobes.
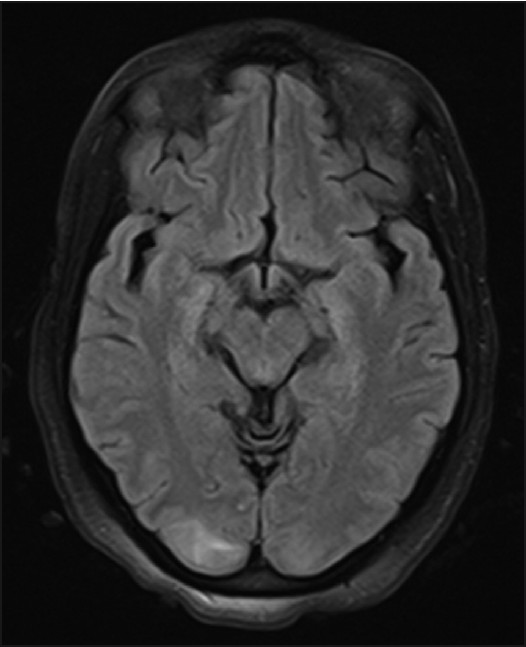
- Axial magnetic resonance image of the brain with Fluid Attenuated Inversion Recovery (FLAIR) sequence demonstrates hyperperintensity within the posterior aspects of both occipital lobes and paramedial aspect of left parietal lobe.
A repeat ophthalmology examination performed the same day after 4 hours demonstrated her visual acuity to be 20/25 OD and 20/30 OS. Color vision and Amsler grid testing showed normal results for both eyes. Pupils were equal, round, and reactive without any relative afferent pupillary defect. Confrontational visual field revealed a small superonasal deficit in the right eye and no deficit in the left. Goldmann visual fields were normal in both eyes. Funduscopic examination revealed tortuous vessels without any optic disc edema or intraretinal hemorrhage.
Typically, symptoms improve over several weeks and such rapid recovery is highly atypical. Our case is unique because of resolution of the visual disturbances of our patient within the same day.
DISCUSSION
PRES is a syndrome characterized by neurotoxic manifestations such as headache, visual disturbances, aphasia, facial numbness, seizure, and ataxia. These are thought to result from cerebral edema.[1] The edema is presumed to be vasogenic cerebral edema indicating an underlying disruption of the blood brain barrier, ultimately considered a failure of cerebral perfusion autoregulation.[23] The edema is typically in the parieto-occipital lobes. It can also be present in the frontal lobes, brainstem, cerebellum, and spinal cord. A diffusion-weighted MRI demonstrates restricted water movement confirming this to be vasogenic in nature.[3]
Various conditions can predispose to PRES. The most common conditions include toxemia of pregnancy (eclampsia and pre-eclampsia), immunosuppression with cyclosporine or tacrolimus, systemic inflammatory response syndrome, multiorgan dysfunction syndrome, and autoimmune conditions such as systemic lupus erythematosus, scleroderma, Wegener's granulomatosis, and polyarteritis nodosa. PRES can also occur after chemotherapy, usually in high doses, with cytarabine, cisplatin, gemcitabine, tiazofurin, bevacizumab, and kinase inhibitor BAY 34-9006.[134] Additionally, there are case reports of PRES occurring in the setting of hypomagnesemia, hypercalcemia, hypocholesterolemia, intravenous immunoglobulin treatment for Guillain-Barre syndrome, ephedra overdose, and tumor lysis syndrome.[1]
The definitive treatment of PRES aims at precipitating factors. It is beyond the scope of our case to discuss treatment for each inciting factor; however, general management of PRES in the presence of toxemia of pregnancy requires a multidisciplinary approach and control of hypertension.
The role of the ophthalmologist is vital as neurotoxic symptoms often present as loss of vision, blurred vision, scotoma, and visual hallucination. The ophthalmologist should perform a thorough examination to evaluate other potential causes of visual abnormalities that can manifest in the peripartum period such as central serous chorioretinopathy, serous retinal detachment, idiopathic intracranial hypertension, Purtscher-like retinopathy, and post-partum pituitary apoplexy.[5]
CONCLUSION
It is important for a practicing radiologist to be familiar with the characteristic imaging features of this reversible disease process for proper management and to avoid unnecessary work-ups.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/36/82341
REFERENCES
- Posterior Reversible Encephalopathic Syndrome. Curr Opin Ophthalmol. 2008;19:479-84.
- [Google Scholar]
- Posterior Reversible Encephalopathy Syndrome, Part 1: Fundamental Imaging and Clinical Features. AJNR Am J Neuroradiol. 2008;29:1036-42.
- [Google Scholar]
- Posterior Reversible Encephalopathy Syndrome, Part 2: Controversies Surrounding Pathophysiology of Vasogenic Edema. AJNR Am J Neuroradiol. 2008;29:1043-9.
- [Google Scholar]
- Posterior Reversible Encephalopathy Syndrome: Is there a difference between Pregnant and Non-Pregnant Patients? Eur Neurol. 2009;62:142-9.
- [Google Scholar]





