Translate this page into:
A Rare Cause of Obstructive Jaundice: Cecal Herniation through the Foramen of Winslow
Address for correspondence: Dr. Ivan Welaratne, Apartment 1, 74 Fitzwilliam Lane, Dublin 2, Ireland. E-mail: welarati@tcd.ie
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Internal abdominal hernias are rarely reported in the literature and have a very low rate of preoperative diagnosis. It is even rarer that they present with jaundice. A 59-year-old Caucasian female presented with a short history of jaundice, dark urine, epigastric pain, vomiting, and obstipation. Her liver biochemistry profile revealed a mixed cholestatic/hepatocellular pattern with significantly elevated bilirubin. She urgently underwent abdominal imaging which provided a preoperative diagnosis of internal herniation of the cecum within the lesser sac through the foramen of Winslow. The dilated bowel was compressing the common bile duct explaining the jaundice. This was repaired intraoperatively by anchoring the mobile cecum. In this case, we highlight the importance of maintaining a high index of suspicion for internal herniation on abdominal imaging with clinical evidence of intestinal obstruction. A foramen of Winslow hernia should be further suspected in the presence of jaundice.
Keywords
Computerized tomography
foramen of Winslow
internal hernia
jaundice

INTRODUCTION
Cases of abdominal internal hernias are rarely reported in the literature. Herniation through the foramen of Winslow is very uncommon and represents only 0.1% of all abdominal hernias.[1] In addition, the rate of preoperative diagnosis has been reported as <10%.[2] Internal hernias most commonly present with signs of acute intestinal obstruction.[3] Delays in diagnosis and treatment can lead to high mortality rates from bowel ischemia. Herniation presenting as acute jaundice has rarely been reported.[345]
Here, we present a case of acute onset obstructive jaundice precipitated by cecal herniation via the foramen of Winslow diagnosed preoperatively on computed tomography (CT).
CASE REPORT
A middle-aged Caucasian female presented to the emergency department with a 1-day history of jaundice and dark urine. This was preceded by 4 days of moderate epigastric pain with nausea, vomiting, and constipation. There was no history of over-consumption of alcohol or indeed any other relevant prior surgical or medical history. On examination, she was visibly jaundiced with abdominal tenderness and guarding in the epigastric area. Her abdomen was mildly distended with reduced bowel sounds.
Initial bloods showed a mixed hepatocellular/cholestatic pattern with markedly elevated bilirubin of 121 μmol/L (normal range: 0–21), aspartate transferase of 189 IU/L (0–40), alanine transferase of 370 IU/L (0–41), gamma-glutamyl transferase of 352 IU/L (10–71), and alkaline phosphatase of 167 IU/L (40–129). Her lactate on venous blood gas sampling doubled within an hour of presentation from 1.64 to 2.89 mmol/L (0.36–1.39).
A plain radiograph of her chest and abdomen [Figure 1a and b] revealed a dilated loop of bowel within the left upper quadrant. This prompted an urgent CT abdomen and pelvis which uncovered a dilated cecum [Figures 1c and 2] within the lesser sac through the foramen of Winslow. Furthermore, there was mass effect on the hepatic hilum with free fluid around the gallbladder as well as evidence of thrombosis at the junction between the splenic vein and superior mesenteric vein. This resulted in a combination of intrahepatic ductal dilatation and edema [Figure 3a and b]. In addition, there was sharp angulation of the cystic duct [Figure 3c].
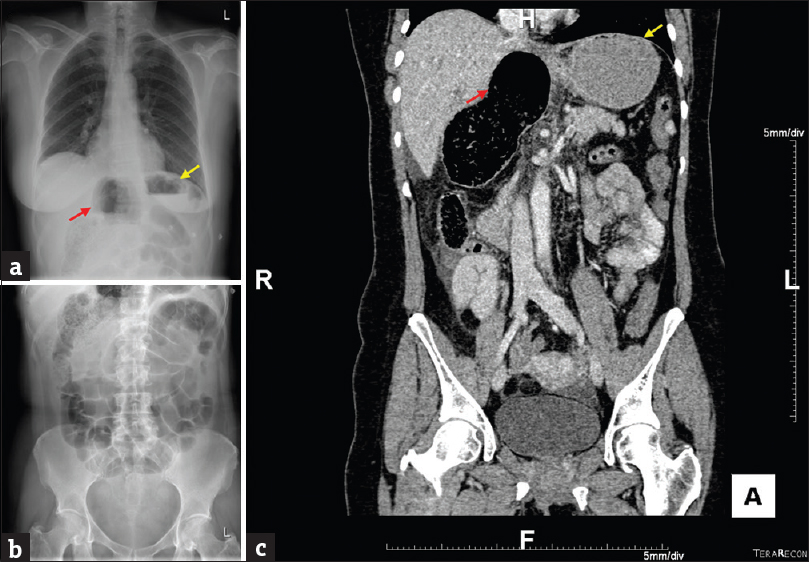
- A 59-year-old Caucasian female presents with epigastric pain, jaundice, vomiting and constipation. (a) Erect chest radiograph reveals dilated hollow viscus (yellow arrow) beside the stomach (red arrow). (b) Abdominal radiograph shows multiple prominent loops of small bowel. (c) Coronal view of computed tomography abdomen and pelvis shows the dilated cecal pole within the lesser sac, corresponding with the radiographic findings.
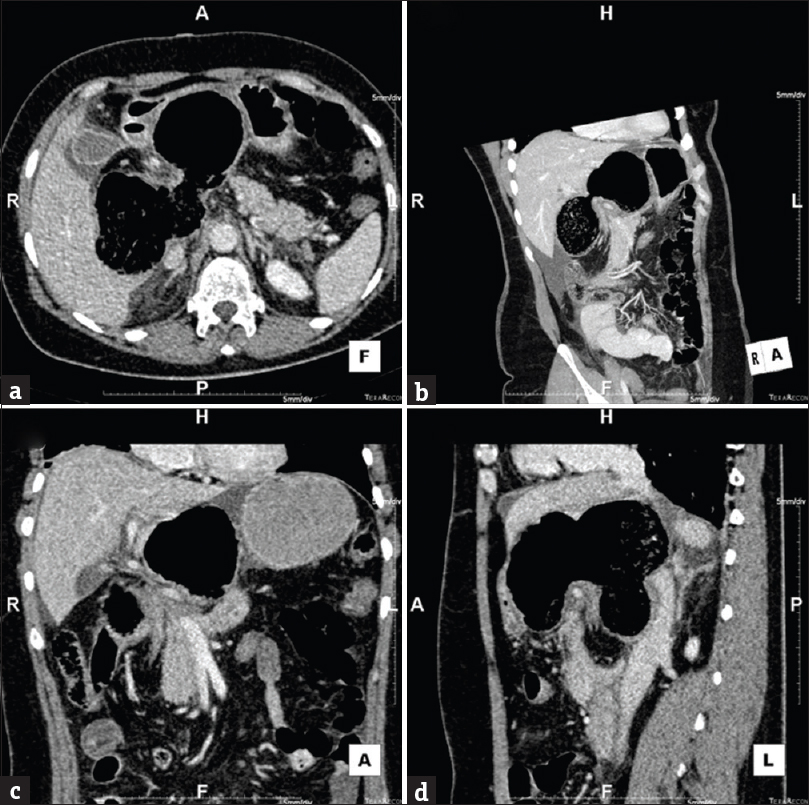
- Multiple planes of computed tomography depicting the twisted, herniated cecum within the lesser sac. Reconstructed images: (a) axial, (b) oblique coronal, (c) coronal, and (d) sagittal views.
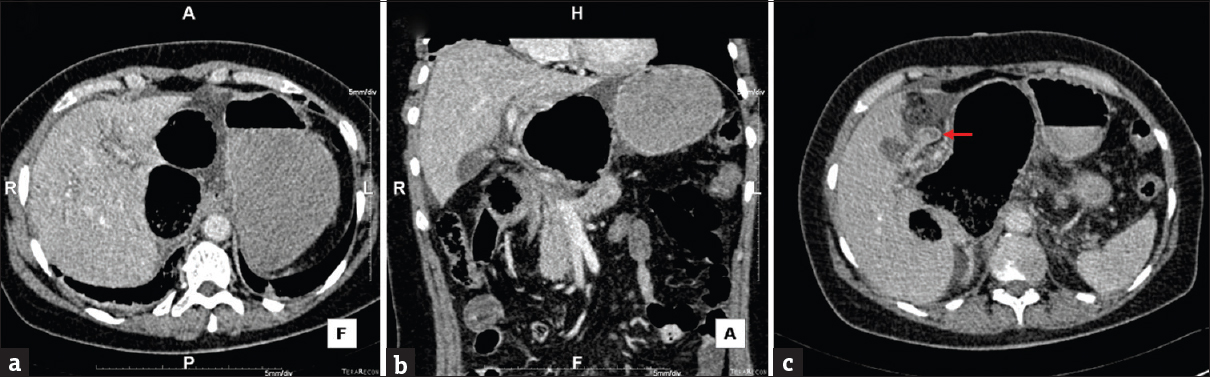
- Computed tomography abdomen showing (a) axial view and (b) coronal view of intrahepatic ductal dilatation resulting from pressure on the biliary tree. Also note surrounding ductal edema and fluid in the gallbladder fossa. (c) Axial view showing sharp angulation of the cystic duct (red arrow).
She underwent an emergency laparotomy during which the internal hernia was reduced manually without complication. Intraoperatively, it was noted that the ascending colon and cecum were not fixed within the retroperitoneum and had their own mesentery resulting in a mobile cecum. This was the precipitating factor for her internal herniation. This was repaired with colo-/cecopexy.
She recovered well postoperatively with normalization of liver biochemistry within several days. There was no recurrence of symptoms at 6 weeks’ postoperation.
DISCUSSION
Internal herniation is a rare occurrence, and there are even fewer cases presenting with jaundice.[36] One mechanism described involves herniation of the gallbladder through the foramen of Winslow.[7] A case presenting with obstructive jaundice and pancreatitis has also been reported in the literature, however the diagnosis was made intraoperatively, with imaging being inconclusive.[4]
In the imaging for our case, the plain radiographs show prominent loops of small bowel. On CT, there is no evidence of small bowel obstruction [Figure 4]. As the patient was vomiting for 4 days before presentation, this could have led to some decompression, hence the caliber of bowel in this study being at the upper limit of normal. Furthermore, the cecum was ascended and twisted within the lesser sac causing effacement of the proximal ascending colon and terminal ileum. Of note, there was compression of the second part of the duodenum as it passed from the gastroduodenal junction, which would explain the early onset of vomiting. Another interesting concurrent finding was the presence of thrombosis at the confluence of the splenic and superior mesenteric veins [Figure 5a], further confirmed by mesenteric vessel congestion [Figure 5b]. The hepatic portal vein (HPV) was not positively visualized more distally [Figure 5c]. However, there was evidence of contrast within the right and left branches of the portal vein within the liver [Figure 5d and e]. It is, therefore, more likely that the HPV itself was compressed by the dilated cecum rather than thrombosed.
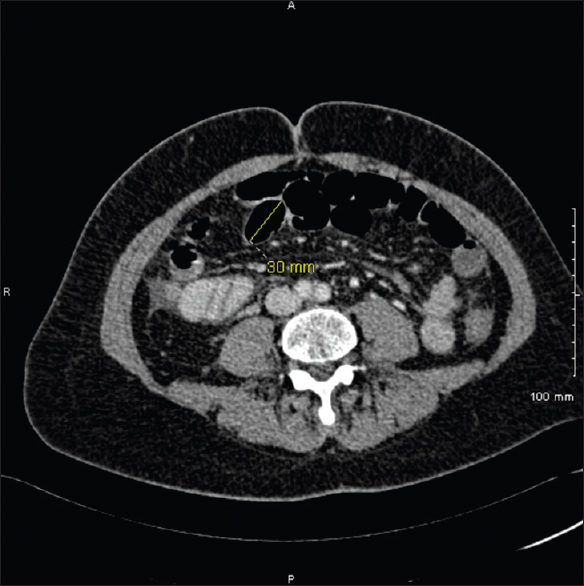
- Axial computed tomography of the mid abdomen showing small bowel calibre at the upper limit of normal.
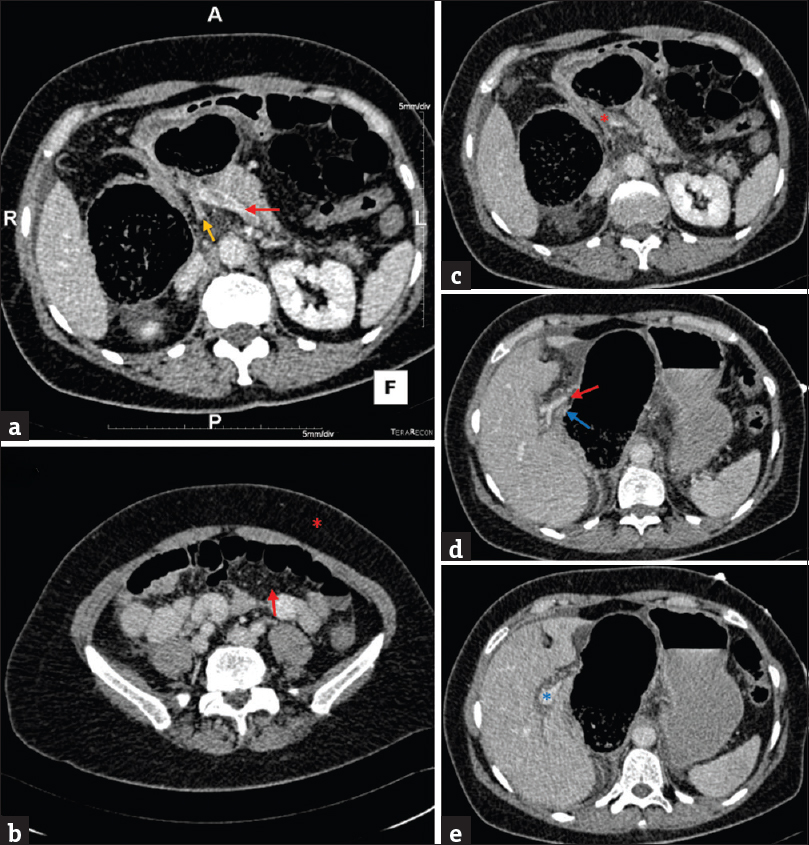
- Multiple axial views of the abdomen on computed tomography. (a) Evidence of thrombosis at the confluence of the splenic vein (red) and the superior mesenteric vein (orange). (b) Misty mesenteric fat (arrow) as compared to normal peripheral fat (asterisk), confirming a degree of thrombosis within the portal venous system. (c) Disappearance of the confluence (asterisk) at the proximal portion of the hepatic portal vein. (d) Depiction of the hepatic hilum showing the hepatic arteries (red) and the re-emergence of the hepatic portal vein (blue). (e) Complete re-emergence of the hepatic portal vein beyond the hepatic hilum (asterisk).
For internal herniation through the epiploic foramen, plain radiographs of the abdomen can identify dilated, gas-containing loops of bowel high in the abdomen.[8] However, CT with multiplanar reconstruction is considered the modality of choice. It aids in identifying classical signs such as: (1) presence of mesentery between the inferior vena cava and the portal vein, (2) an air-fluid collection in the lesser sac with a beak directed toward the foramen of Winslow, (3) absence of the ascending colon in the right gutter, and (4) two or more bowel loops within the high subhepatic spaces.[9]
Multiple risk factors have been reported to increase the risk of herniation through the foramen of Winslow including an enlarged foramen of Winslow, the persistence of an ascending mesocolon with associated increased mobility of the cecum/ascending colon and an abnormally long small bowel mesentery.[8] In this particular case, the cecum and ascending colon had their own mesentery which required surgical fixing to prevent recurrence of internal herniation.
CONCLUSION
This case highlights the importance of maintaining a high index of suspicion for internal hernias when reporting on CT imaging presenting with clinical evidence of intestinal obstruction. A foramen of Winslow hernia should be further suspected in the presence of accompanying jaundice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/24/234666.
REFERENCES
- Foramen of Winslow hernia: A minimally invasive approach. Surg Endosc. 2015;29:2385-8.
- [Google Scholar]
- Intestinal obstruction caused by a foramen of Winslow hernia. Am J Surg. 2008;196:242-4.
- [Google Scholar]
- Internal hernias: Anatomical basis and clinical relevance. Surg Radiol Anat. 2007;29:333-7.
- [Google Scholar]
- Internal hernia presenting as obstructive jaundice and acute pancreatitis. Scand J Gastroenterol. 2002;37:983-6.
- [Google Scholar]
- Obstructive jaundice due to foramen of Winslow hernia: A case report. Aust N Z J Surg. 1991;61:467-9.
- [Google Scholar]
- Herniation through the foramen of Winslow presenting as obstructive jaundice. Pediatr Surg Int. 2005;21:560-2.
- [Google Scholar]
- Review of internal hernias: Radiographic and clinical findings. AJR Am J Roentgenol. 2006;186:703-17.
- [Google Scholar]






