Translate this page into:
A Rare Case of Dysembryoplastic Neuroepithelial Tumor
Address for correspondence: Dr. Jun K. Shen, Department of MRI, Second Affiliated Hospital of Soochow University, Sanxiang Lu, Jiangsu Province, 215004, China. E-mail: junkansh@yahoo.com.cn
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We present a rare case of dysembryoplastic neuroepithelial tumor, a rare benign glioneuronal tumor of the central nervous system. It generally occurs in the supratentorial region and the temporal cerebral cortex in children and young adults. The most common presentation is epilepsy. The supratentorial tumor without any signs of mass effect or peritumoral edema is the conventionally accepted diagnostic criteria. In this case of a 19-year-old male with intractable epilepsy, atypical features such as the location of the tumor and the presence of mass effect and peritumoral edema made imaging diagnosis difficult. Diagnosis was confirmed through histopathology. Due to its recent discovery and relatively rare occurrence it is important for radiologists to recognize this disease entity.
Keywords
DNET
dysembryoplastic neuroepithelial tumor
epilepsy
magnetic resonance imaging
INTRODUCTION
This is a case of DNET (dysembryoplastic neuroepithelial tumor) that presented with atypical findings making a radiological diagnosis uncertain. DNET is a rare benign tumor generally seen in children and adolescents with intractable epilepsy. The typical radiological findings of DNET are supratentorial tumor generally affecting the temporal lobes and without any peritumoral edema or mass effect.[1] Given its excellent prognosis this should be considered in any case of supratentorial mass presenting with epilepsy, especially in pediatric and adolescent age groups.[2]
CASE REPORT
A 19-year-old male with a 6-month history of intractable seizures was referred for an MRI examination by the neurologist.
MRI scan conducted on the 1.5T (Philips achieva) machine. The sequences performed were T1weighted imaging (T1W1), T2 weighted imaging (T2W1), Fluid Attenuated Inversion Recovery (FLAIR), diffusion weighted imaging, and a gadolinium (Gd) contrast enhanced scan. The scans showed a large irregular cystic mass lesion in the right temporal-parietal-occipital region with a low signal on T1WI [Figure 1] and a high signal on T2WI [Figure 2] and a hyperintense region around the tumor on FLAIR sequence. Additionally, peritumoral edema and mass effects were seen in the form of a midline shift. The posterior horn of the lateral ventricle and the third ventricle were compressed and deviated anteriorly. The Gd contrast enhanced scan [Figure 3a and b] showed enhancement of the lesion wall. No other parenchymal lesions were detected.
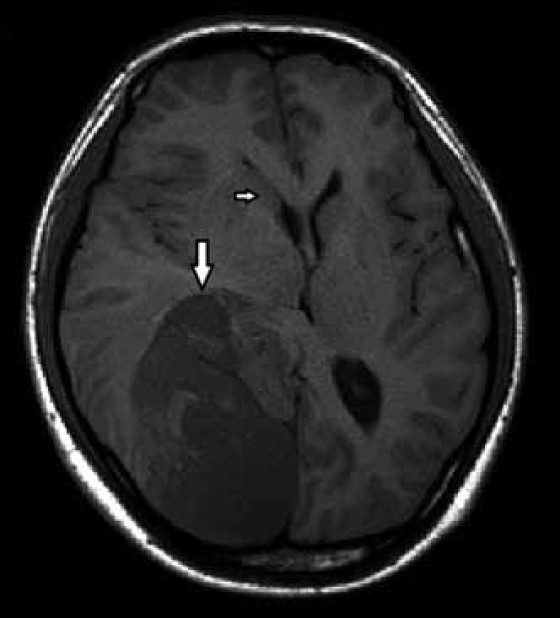
- TI weighted image of the 19-year-old male with dysembryoplastic neuroepithelial tumor involving the right temporo-oocipital lobe (large arrow) and mass effect at the anterior horn of right lateral ventricle (small arrow).
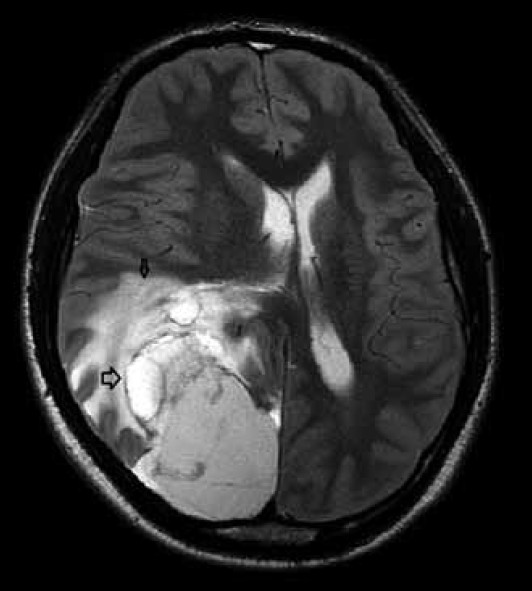
- T2 weighted axial image at the level of head of caudate nucleus shows the peritumoral edema (small arrow) multinodular lesion in the temporooccipital lobe (large arrow).
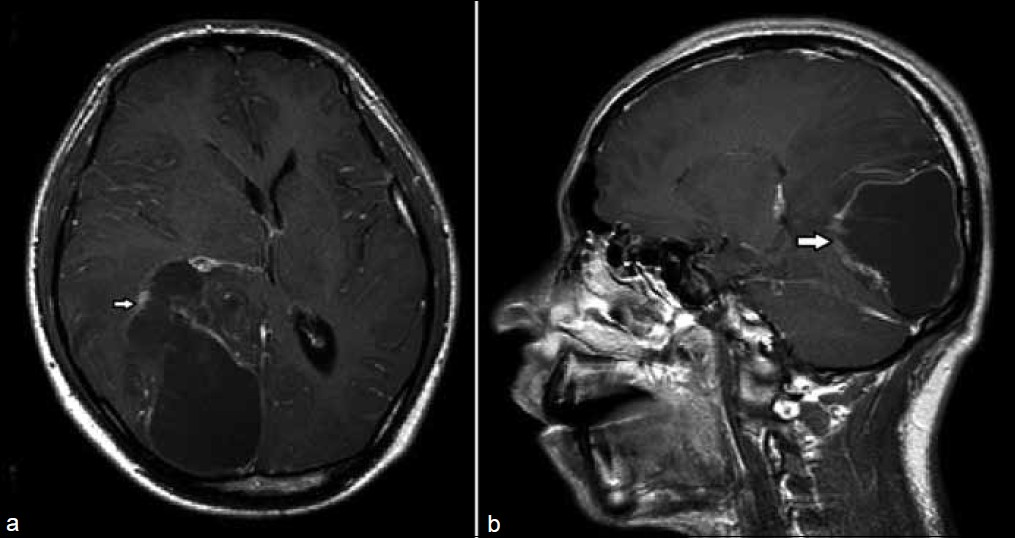
- (a) Gd contrast enhanced T1 weighted axial image at the level of caudate nucleus shows the lesion wall enhancement (arrow). (b) Corresponding sagittal plane lesion involving temporo-occipital lobe reconfirms the axial plane features
Additionally, but unrelated to the presenting symptoms a maxillary sinus cyst was also seen.
Given the age, history, and MRI findings of the lesion size and content we considered the diagnosis of a right temporal parietal occipital cystic mass -probably a glioma (ependymoma or large astrocytoma) and the patient was referred for surgery, following which a sample was sent for histopathology analysis.
Pathology combined with immunohistochemistry [Figure 4] findings was diagnostic of dysembryoplastic neuroepithelial tumor (WHO Grade 1).
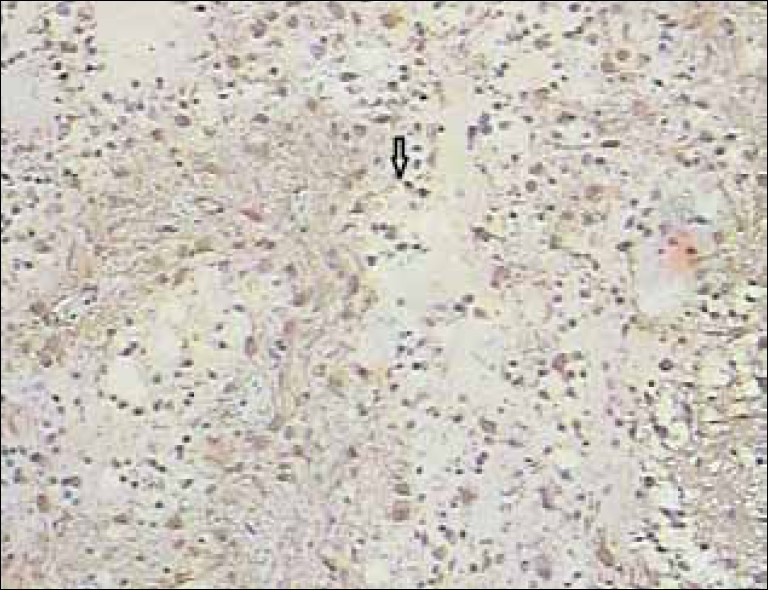
- Glial Fibrillary Acidic Protein (GFAP) stained histopatholgy slide shows the specific glioneuronal elements (arrow). Immunohistochemistry for glial fibrillary acidic protein (GFAP), S-100 protein, establish the presence of astrocytic and neuronal components, while GFAP reactivity is negative for an oligodendrocytic component
The patient was successfully treated and follow-up examinations were done as required without any findings of consequence.
DISCUSSION
Dysembryoplastic neuroepithelial tumors are a relatively recent discovery having been identified barely 2 decades ago.[3] The name given to this type of tumor is controversial as its dysembryogenetic origins are subject to debate. Presently, DNETs are classified by WHO as Grade 1 neuronal and mixed glial tumors.[4] Generally DNET is a benign tumor but there have been cases of malignant transformation.[5] This tumor generally affects children and young adults and presents with a history of intractable seizures. It is a supratentorial tumor most commonly located in the temporal lobe.[1] The hallmarks for diagnosis are an intracortical supratentorial tumor in the temporal lobe with multinodular structure and no peritumoral edema or signs of mass effect in young patients who present with intractable seizures.[1]
In our case the large size of tumor with occipital involvement and the absence of characteristic multinodular appearance[6] and the presence of mass effect and edema made the diagnosis difficult. Diagnosis was possible only through histopathological analysis. Microscopically, all DNETs exhibit multiple intracortical nodules of varying sizes. Pathologically, DNET is a benign, predominantly intracortical lesion composed mainly of a population of heterogeneous cellular components, such as oligodendrocyte-like cells with admixtures of mature neurons and astrocytes.[3] The principal differential diagnoses of DNETs are oligodendrogliomas and gangliogliomas. In our case, the diagnosis was established based on the histopathological findings (confirmed on review) and clinical data. Typically, the diagnosis is established by pathology.[7] In some cases oligodendroglioma with cystic changes and entrapped neurons may resemble DNET on imaging.[8] Thus, the diagnosis of DNET cannot rely just upon imaging features but needs a multidisciplinary contribution from the clinical and diagnostic department involving the clinician, radiologist as well as the pathologist to reach a definite and conclusive diagnosis.[9] In this case the neuroimaging features were not typical of DNET.[10] The variations in morphological and pathological appearances of DNET are still being documented due to the low incidence of this disease.
The best course of treatment for DNET is a surgical resection. However, with increasing availability of modern histological and imaging facilities the incidence of diagnosed cases is increasing. Considering the fact that this tumor is benign and slowly growing with excellent prognosis and surgical outcome without any lasting neurological deficit,[2] the radiologist should consider this entity during differential diagnosis of a young adult or child with relevant clinical history of late onset of intractable epilepsy even in the absence of the typical radiological markers.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/60/102057
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Dysembryoplastic neuroepithelial tumors.Analysis of 16 cases. Neurochirurgie. 1999;45:180-9.
- [Google Scholar]
- Revised WHO classification and new developments in diagnosis of central nervous system tumors. Pathologe. 1995;16:245-55.
- [Google Scholar]
- Clinicopathologic features of recurrent dysembryoplastic neuroepithelial tumor and rare malignant transformation: A report of 5 cases and review of the literature. J Neurooncol. 2009;94:283-92.
- [Google Scholar]
- Dysembryoplastic neuroepithelial tumors: MR and CT evaluation. AJNR Am J Neuroradiol. 1996;17:419-30.
- [Google Scholar]
- Dysembryoplastic neuroeptihelial tumor (DNT): An immunohistochemical and ultrastructural study. J Neuropathol Exp Neurol. 1994;53:184-95.
- [Google Scholar]
- Dysembryoplastic neuroepithelial tumor.A tumor with small neuronal cells resembling oligodendroglioma. Am J Surg Pathol. 1994;18:604-14.
- [Google Scholar]
- The usefulness of MR imaging in the diagnosis of dysembryoplastic neuroepithelial tumor in children: A study of 14 cases. AJNR Am J Neuroradiol. 2003;24:829-34.
- [Google Scholar]
- Dysembryoplastic neuroepithelial tumors: CT, MR findings and imaging follow-up: A study of 53 cases. J Neuroradiol. 2001;28:230-40.
- [Google Scholar]






