Translate this page into:
Morphometric evaluation of the proximal tibiofibular joint among patients with knee joint pain: A pilot study and literature review

*Corresponding author: Jakub Krzysztof Sojat, Department of Anatomy, Faculty of Health Sciences in Katowice, Medical University of Silesia, Katowice, Poland. jakub.sojat.med@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sojat JK, Szlęzak MJ, Zamarlik MI, Bressler K, Zieliński M, Rajca J, et al. Morphometric evaluation of the proximal tibiofibular joint among patients with knee joint pain: A pilot study and literature review. J Clin Imaging Sci. 2024;14:43. doi: 10.25259/JCIS_122_2023
Abstract
Objectives:
The proximal tibiofibular joint (PTFJ) serves as a crucial stabilizing component of the entire knee joint complex. Morphometric analysis of the PTFJ can lead to clinically significant conclusions for orthopedic specialists and physiotherapists. The aim of the study was to assess the values of the inclination angle of the PTFJ in the sagittal and coronal planes using magnetic resonance imaging in patients with knee pain.
Material and Methods:
Measurements of the inclination angle were conducted on 48 patients divided into three groups: Those with damaged medial meniscus (M), those with knee joint cartilage damage (Ca), and the control group (C), in which no deviations from normality were observed in the analyzed imaging study.
Results:
The mean values of the tibiofibular joint inclination angle in the frontal plane were as follows: (C) 16.927° ± 1.778; (Ca) 16.822° ± 2.537; (M) 14.958° ± 1.760. In the sagittal plane, the corresponding values were: (C) 38.155° ± 1.524; (Ca) 39.392° ± 1.927; (M) 37.471° ± 1.165. Although the mean tibiofibular joint inclination angle was lowest in the group with medial meniscus injury when compared to the control group, these differences did not reach statistical significance.
Conclusion:
Measuring and observing the variety of PTFJ inclination angles among patients are conducive to better understanding its influence on knee pain. The differences in the PTFJ inclination angle between groups in our pilot study were not statistically significant. Consequently, the study necessitates replication within a substantial population cohort.
Keywords
Proximal tibiofibular joint
Inclination angle
Magnetic resonance imaging
Morphometry
Gonarthrosis
INTRODUCTION
The morphometry of the proximal tibiofibular joint (PTFJ) is rarely described in the literature.[1-5] This may be attributed to its limited range of motion, infrequent injuries, or fractures of the region around the head and neck of the fibula. However, it is crucial to remember that from both an anatomical and functional standpoint, this joint is closely connected to the knee joint and thereby contributes to its stability. When analyzing the function, stabilization, and biomechanics of the knee joint, attention should not solely be directed at the knee joint itself, but rather at the entire complex encompassing both joints.
When evaluating the structure of the PTFJ, numerous authors highlight its inseparable relationship with injuries within the knee joint, which directly influence the PTFJ.[5-7] Certain anatomical studies point to the tibiofibular joint as a significant supporting element for knee joint stability.[8,9] The anatomy of the PTFJ is well understood; the articular surface of the fibula faces downward, backward, and laterally, enabling dorsal movement of the fibula relative to the tibia due to the activity of the biceps femoris muscle.[6] The fibular muscles are also noteworthy due to their attachments.[6] Consequently, damage to these muscles may result in PTFJ dysfunction. Furthermore, the popliteal bursa directly borders the posterior capsule of the PTFJ. In 20% of cases, this recess will communicate with the tibiofibular joint space, potentially affecting the spread of inflammation in both joints.[6]
In 1974, Ogden[10] described the morphology of the PTFJ based on cadaver dissections, classifying it into two types: Horizontal (fibular angle <20°) and oblique (fibular angle >20°) types. These are the primary typologies used daily by anatomists and orthopedic surgeons.[5,10,11] Researchers define the angle of inclination as the angle between the line of greatest inclination of the PTFJ articular surface and the horizontal plane.[5,10] In clinical practice, the most common injuries encountered are, respectively, medial meniscus injury (50%); anterior cruciate ligament (ACL) injury (30%); and, less frequently, lateral meniscus injury (18%).[11] It is important to emphasize that scientific research frequently points to the occurrence of concurrent damage to multiple structures within the knee joint.[11,12] The existing literature lacks a correlation between the structure of the PTFJ and specific injuries within the knee joint.
The aim of the study was to assess the values of the inclination angle of the PTFJ based on magnetic resonance imaging (MRI) in patients with medial meniscus tear and chondromalacia of the knee joint.
MATERIAL AND METHODS
A total of 80 patients who underwent an MRI examination of the knee joint due to injury or pain between 2019 and 2021 were initially reviewed. Due to the retrospective nature of the study, the requirement for ethical committee approval is not required. Based on MRI examination and available medical documentation, we identified forty-eight (48) patients who met inclusion and exclusion criteria to ensure the formation of homogeneous groups. The inclusion criteria for the following groups were medial meniscus injury (M group), chondromalacia of the knee joint (Ca group), and the lack of deviations from the norm in the knee joint structures as observed in the MRI (C group). Patients from the control group (C) were also sourced from a retrospective database and underwent diagnostic MRI due to suspected knee injury or pathology. The exclusion criteria from the study were simultaneous damage to the cartilage and medial meniscus, lateral meniscus injury, neoplastic changes within the examined bone structures, degenerative changes at grade III and IV of the knee joint, and damage to the knee joint ligaments including ACL and posterior cruciate ligaments, (respectively) and collateral ligaments (medial collateral ligament and lateral collateral ligament [LCL]). To minimize potential discrepancies arising from variations in resolution, slice thickness, and different imaging protocols, only MRI scans of patients who were examined using the magnetic resonance device available in our clinic (1.5T general electric apparatus) were included for further analysis. The population characteristics of established groups are displayed in Table 1. Due to the retrospective nature of the research, it did not require the approval of a Bioethics Committee. Data confidentiality was respected following the Helsinki Declaration. During the study, full confidentiality of data was ensured and ethical standards of the analyzed patients were observed. All MRI scans were appropriately anonymized to maintain data confidentiality.
| Group | M (n=16) | Ca (n=16) | C (n=16) |
|---|---|---|---|
| Age (years) | 47±14 | 34±11 | 34±11 |
| Knee (left: right) | 11:5 | 9:7 | 8:8 |
Medial meniscus injury (M group), chondromalacia of the knee joint (Ca group), and the lack of deviations from the norm in the knee joint structures as observed in the MRI (C group)
All the MRI studies adhered to the same imaging protocol, with a slice thickness of 3 mm and an interspace gap of 4 mm. All morphometric measurements of the PTFJ were performed on a dedicated diagnostic workstation using OsiriX MD software (version 8.0; Osiris Foundation, Geneva, Switzerland). The images were analyzed in T1-weighted projection. Measurements of the PTFJ in the coronal and sagittal planes were executed by the two independent researchers, and the results were subsequently averaged. The measurement method was based on the protocol established by Chang et al.[3]
The angle of inclination of the fibula bone was measured in the images from the moment of the first appearance of the entire articular surface of the PTFJ, both in the sagittal and coronal planes.[3] In the sagittal plane, the following points were marked: e and f – points connecting the anterior and posterior horns of the lateral meniscus at the height of the tibial plateau, a – the most anterior point on the surface of the fibula, and b – the most posterior point on the surface of the fibula [Figure 1]. In the frontal plane, c – the most lateral point on the articular surface of the fibula; a – the most medial point on the articular surface of the fibula; e – the lateral apex of the tibial plateau; and f – the medial apex of the tibial plateau [Figure 2]. The PTFJ inclination angle was determined by establishing the lines |ef| and |ab| in the sagittal plane as well as the lines |ef| and |ac| in the coronal plane. Therefore, in the sagittal plane, line |ef| must be parallel to the tibial plateau, and line |ao| must be parallel to line |ef|. In the coronal plane, line |ao| must be parallel to |ef|. Subsequently, the PTFJ inclination angle was calculated in the Osirix software between the line parallel to the tibial plateau and the line passing through the articular surface of the PTFJ [Figures 1 and 2].
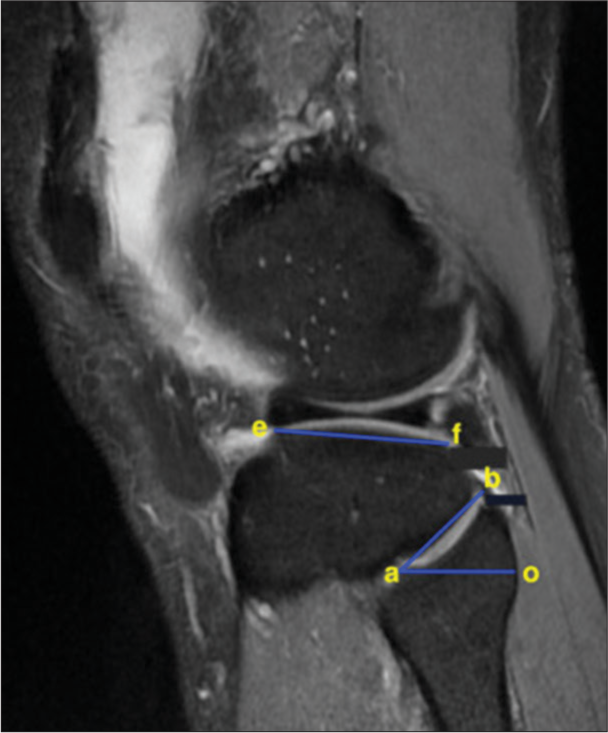
- Methodology of determining the proximal tibiofibular joint inclination angle in the sagittal plane based on T1-weighted magnetic resonance image: e, f – points connecting the anterior and posterior horns of the lateral meniscus at the level of the tibial plateau, a – the most anteriorly positioned point of the tibial surface, and b – the most posteriorly positioned point of the tibial surface. Line |ef| must be parallel to the tibial plateau, and line |ao| must be parallel to line |ef|.
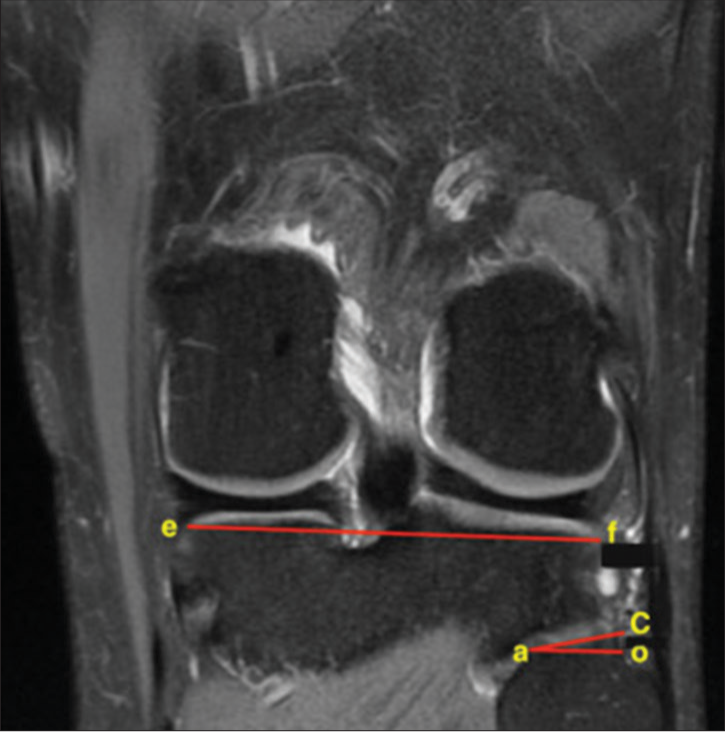
- Methodology of determining the proximal tibiofibular joint inclination angle in the coronal plane based on T1-weighted magnetic resonance image: C – the most laterally located point of the articular surface of the tibiofibular joint on the tibial side; a – the most medially located point of the articular surface of the tibiofibular joint on the tibial side; e – the lateral apex of the tibial plateau; f – the medial apex of the tibial plateau. Line |ao| must be parallel to |ef|.
Statistical analysis
KyPlot 6.0 software was used for statistical analysis. The data were analyzed using Bartlett’s test for homogeneity of variance, the Tukey–Kramer test, and the Dunnett test for comparisons with the control group. Inter-rater reliability was assessed using Pearson’s correlation. A significance level of P ≤ 0.05 was adopted. Quantitative data are presented as mean ± standard deviation.
RESULTS
The analysis revealed that in the coronal plane, the mean value of the PTFJ inclination angle was highest in the C group (16.93°), compared to Ca and M groups (16.82° and 14.96°, respectively). The obtained results did not achieve statistical significance at P ≤ 0.05 level, and no statistically significant differences were noted between the groups with medial meniscus damage (M) and knee chondromalacia (Ca) as well as between those groups and the control group (C) [Table 2].
| Groups | PTFJ (S) (°) | PTFJ (F) (°) | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| C | 38.15 | ±6.10 | 16.93 | ±7.11 |
| Ca | 39.39 | ±7.71 | 16.82 | ±10.15 |
| M | 37.47 | ±6.61 | 14.96 | ±7.04 |
Medial meniscus injury (M group), chondromalacia of the knee joint (Ca group), and the lack of deviations from the norm in the knee joint structures as observed in the MRI (C group). PTFJ: Proximal tibiofibular joint, SD: Standard deviation
Analyzing the mean value of the PTFJ inclination angle in the sagittal plane, the results demonstrated that the highest value occurred in the Ca group (39.4°). In the C and M groups, the mean angle values were lower, 38.2° and 37.5°, respectively. Similar to the coronal plane, the results of intergroup comparisons did not achieve statistical significance [Table 2].
DISCUSSION
In our study, we investigated the PTFJ morphology by measuring the fibular inclination angle using MRI on the coronal and sagittal cross-sections to determine the associations between PTFJ inclination angle and the occurrence of various knee disorders. In our preliminary investigation, even though statistical significance between groups was not evident, a noticeable trend emerged wherein the M group exhibits comparatively lower mean inclination angles in both coronal and sagittal cross-sections. A more robust trend might be expected to manifest when considering a larger MRI-based population. The relatively small part of the population in our preliminary study can be linked to its single-site nature and strict exclusion criteria, factors that limited patient enrollment within the respective groups. This is important to note that MRI is an accurate, non-invasive, cost-effective technique for examination of the soft tissue and osseous structures of the knee.[13] Therefore, we believe that this type of diagnostic imaging is the most effective method for evaluating PTFJ morphometry. Upon reviewing the literature, we did not find studies describing alterations in the PTFJ inclination angle within certain knee joint disorders, such as medial meniscus damage and knee chondromalacia.
Several researchers propose that assessing the PTFJ inclination angle could potentially aid in the early identification of degenerative alterations in patients.[2-4] Numerous anatomical investigations have elucidated the typical structure and pathomorphology of the PTFJ.[1,3,5,10,14-16] These studies have provided insights into the PTFJ inclination angle by performing measurements on human cadavers or radiographic images. In 1974, Ogden[10] defined and classified PTFJ inclination angles by extensively examining 84 fibular bone specimens and analyzing 200 radiographs. It is noteworthy that certain morphometric investigations of this joint were carried out also on cadavers.[10,13-15] Both, radiological and cadaver studies, exhibit differences in measurement techniques and outcomes when compared to our research. Measurements taken from cadavers might be inherently less precise due to the influence of cadaver preservation agents such as formalin, which can cause contractions in sectional materials. Consequently, the advantage of conducting measurements using MRI images lies in their ability to retain tissue appearance and structural integrity. Furthermore, it is worth noting that numerous researchers emphasize the strong correlation between the PTFJ and the knee joint. Based on observations, several authors pointed out that after contrast agent injection, this interrelation is more pronounced in MRI investigations compared to anatomical examinations on cadavers.[2,9,14,15] This may account for the potential accuracy of delineating disparities in anatomical structures through MRI scans rather than cadaveric studies. Consequently, the assessment of area dimensions or angles may reveal variations between groups within cadaveric investigations, while such differences might remain elusive in studies employing alternate methodologies, such as MRI scans. The absence of statistically significant intergroup disparities in our study could plausibly be attributed to its MRI-based foundation. The relatively broader age span encompassed within our study cohort as opposed to other studies might also contribute to the attenuated level of significance.
In the available literature, only a few studies describe the PTFJ inclination angle variations in knee joint structures, particularly in the presence of lateral meniscus abnormalities, employing MRI images.[3,5] Shahrezaee et al.[5] measured the PTFJ inclination angle in patients with lateral meniscus abnormalities, demonstrating that patients with such abnormalities exhibit a significantly smaller PTFJ inclination angle compared to a control group, with mean values of 15.2° and 22.4°, respectively. The authors chose to exclude individuals below 20 and above 40 years of age, citing potential variabilities and degenerative progression of the knee joint disease. Our study encompassed a wider age range, which may have influenced the obtained results. The methodology for angle calculation is also of significance. The approach to computing the PTFJ inclination angle differs significantly from the methodology we employed. The authors draw a line through the articular surface of the PTFJ, followed by two perpendicular lines, calculating the PTFJ inclination angle accordingly. Furthermore, it is noteworthy that the authors reported lower PTFJ inclination angles in patients with conditions such as lateral meniscus damage or discoid meniscus, aligning well with our findings.[5] Moreover, upon comparing groups with discoid meniscus and lateral meniscus damage, the mean PTFJ inclination angle significantly decreases in the group with lateral meniscus damage.[5] Therefore, it can be hypothesized that a reduced PTFJ inclination angle might be linked to lateral or medial meniscus injuries or chondromalacia of the knee joint. Although the research methodology differs from ours, a similar trend in the results can be observed, indicating a level of consistency. However, it is important to note the differences in methodology. Chang et al.[3] examined PTFJ morphometrics in patients with advanced knee osteoarthritis scheduled for total knee arthroplasty. The study was based on MRI scans of 408 patients (average age 63.2 years). The authors demonstrated that the fibular area of the PTFJ is smaller in patients with advanced knee osteoarthritis as measured by the PTFJ inclination angle.[3] It is important to note that the authors employed the same measurement method as utilized in our study. Furthermore, the study was conducted on Australian populations, with the groups being gender-homogeneous. It is worth emphasizing that the authors meticulously selected patients to create the most homogeneous groups possible. Patients with rheumatoid diseases, numerous MRI artifacts, and neoplastic changes were excluded. In this context, it is feasible to claim that our study’s exclusion criteria are quite similar in their rigorousness. The careful selection of uniform groups is pivotal to minimizing the impact of variables on PTFJ morphometrics. In conclusion, the work by Chang et al.[3] suggests that a smaller PTFJ surface area could predispose to knee osteoarthritis. These findings are remarkably consistent with our own, particularly concerning the mean PTFJ inclination angle examined in the sagittal plane within the group with chondromalacia of the knee joint. It is worth emphasizing that the methodology is identical, with strict inclusion and exclusion criteria. The only difference is the size of the groups. However, it should be noted that our research is a pilot study involving participants characterized by knee joint pain.
Eichenblat and Nathan[14] investigated the PTFJ inclination angle using knee joint specimens. The authors demonstrated a statistically significant correlation between PTFJ degeneration and knee osteoarthritis, particularly in the medial compartment. The study encompassed a total of 489 fibular bones and 50 knee joint specimens. The fibulas were sourced from different historical periods, yet the specimens belonged to the Israeli population. The research methodology was founded on a customized goniometer model, which facilitated the calculation of the inclination angle by inserting the fibular bone or applying the goniometer to the PTFJ articular surface.[14] It is worth noting that the methodology significantly diverged from the approach employed in our study, thereby precluding direct result comparison. Considerable morphological variability was noted, accompanied by frequent degenerative changes. The range of inclination spanned from 5° to 80°. In summary, reducing the PTFJ inclination angle and decreasing the articular surface of the PTFJ in patients with medial meniscus damage are likely to lead to the development of knee osteoarthritis, particularly in the medial compartment of the knee joint.[14,15] The authors explain the reduction in the angle to the potential distortion of varus knee alignment, leading to increased strain on the LCL and biceps femoris tendon.[14,15] Consequently, due to the proximity of these structures to the fibular bone head, heightened pressure within the PTFJ might result, subsequently fostering greater PTFJ degeneration.[15] Comparing with our results, it is worth emphasizing that in the sagittal plane, the value of the PTFJ inclination angle in group M was the smallest, which may be consistent with the context of the above studies. A lower value of the PTFJ inclination angle, especially in the case of damage to the medial meniscus, may be a predictor of degenerative changes in the knee joint. However, due to different research methodologies, these studies cannot be compared directly.
Huang et al.[4] investigated PTFJ morphometrics in a group of 40 patients, focusing particularly on the PTFJ inclination angle. The study involved an equal allocation of participants to both the study and control groups (1:1 ratio), with 50% of women and 50% of men assigned to each group. The research was conducted on a Chinese population, with the participants’ ages being equal to or below 50 years. The authors established that a lower value of the fibular inclination angle correlates with an increased risk of knee osteoarthritis in the medial compartment.[4] From a clinical perspective, early prevention of knee osteoarthritis in middle-aged and older individuals in correlation with alterations in the PTFJ inclination angle should be contemplated. However, it is essential to emphasize that the authors analyzed the PTFJ inclination angle based on radiographs and utilized a slightly different methodology than ours.[4] Moreover, PTFJ morphometrics might slightly differ when analyzing a European population or individuals with knee osteoarthritis after the age of 50. In conclusion, while these studies may align with our findings, the research diverges significantly due to the examination methodology, group allocation, and the specific population on which the studies were conducted. It is important to underscore that, owing to the rigorous inclusion and exclusion criteria applied in our study, we intend to expand our research to encompass a larger cohort of patients in the future. The number of MRI studies should be augmented, divided into finer subgroups, and meticulously correlated with the clinical data of the patients.
Limitations of study
The pilot study was conducted with a group of 48 patients, adhering to very strict inclusion and exclusion criteria. In the future, it would be worthwhile to divide the study groups into age categories and assess the effect of the PTFJ angle according to age and gender. Given the pilot nature of this study, we did not divide the participants into smaller subgroups, as the small sample size would have precluded meaningful statistical analysis.
CONCLUSION
Several authors have observed a relationship between a smaller PTFJ inclination angle or reduced joint surface area and a predisposition to knee joint degenerative changes. As repeatedly indicated, discrepancies between our results and those of other authors mainly stem from differences in measurement methodologies, variations in research material (MRI images of patients vs. measurements on cadavers), and differences in the populations on which the measurements were conducted. Clinically, it is important to consider the value of the PTFJ inclination angle due to its potential relation to predisposition for knee joint degenerative changes. Our study results indicate the need to delve into factors that may contribute to reduced PTFJ inclination angles. Exploring causal relationships in PTFJ and knee joint morphometry can enable early preventive measures against knee joint degeneration in middle-aged and older individuals. In addition, considering other structural damages within the knee joint, such as cruciate ligament injuries, could lead to subgroup analyses to establish correlations between PTFJ morphometry and occurrences of damage or injuries within the knee joint. An in-depth analysis of the PTFJ inclination angle and an understanding of its pathobiomechanics can contribute to more comprehensive diagnostics for patients with structural damage within the knee joint.
Ethical approval
As per letter dated 08.10.2024, issued by the Bioethics Committee, Medical University of Silesia in Katowice, the IRB approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The forgotten joint: Quantifying the anatomy of the proximal tibiofibular joint. Knee Surg Sports Traumatol Arthrosc. 2018;26:1096-103.
- [CrossRef] [Google Scholar]
- Associations between the morphological parameters of proximal tibiofibular joint (PTFJ) and changes in tibiofemoral joint structures in patients with knee osteoarthritis. Arthritis Res Ther. 2018;24:34.
- [CrossRef] [Google Scholar]
- A novel method for assessing proximal tibiofibular joint on MR images in patients with knee osteoarthritis. Osteoarthritis Cartilage. 2018;26:1675-82.
- [CrossRef] [Google Scholar]
- Association between the inclination angle of the proximal tibiofibular joint surface and medial compartment knee osteoarthritis. Ann Palliat Med. 2021;10:8753-61.
- [CrossRef] [Google Scholar]
- Proximal tibiofibular joint inclination angle and associated meniscal tear in patients with discoid lateral meniscus. Maedica (Bucur). 2019;14:116-20.
- [CrossRef] [Google Scholar]
- Anatomy of the proximal tibiofibular joint and interosseous membrane, and their contributions to joint kinematics in below-knee amputations. J Anat. 2015;226:143-49.
- [CrossRef] [Google Scholar]
- Is stability of the proximal tibiofibular joint important in the multiligament-injured knee. Clin Orthop Relat Res. 2014;472:2691-7.
- [CrossRef] [Google Scholar]
- Role of the proximal tibiofibular joint on the biomechanics of the knee joint: A three-dimensional finite element analysis. Injury. 2022;53:2446-53.
- [CrossRef] [Google Scholar]
- Kinematics of the proximal tibiofibular joint is influenced by ligament integrity, knee and ankle mobility: An exploratory cadaver study. Knee Surg Sports Traumatol Arthrosc. 2019;27:405-11.
- [CrossRef] [Google Scholar]
- The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res. 1974;101:186-91.
- [Google Scholar]
- Cruciate ligament and meniscus injuries of the knee joint in magnetic resonance imaging. In New diagnostic and therapeutic methods. :128-37. (In Polish)
- [Google Scholar]
- Imaging of athletic injuries of knee ligaments and menisci. Sports imaging series. Radiology. 2006;281:23-40.
- [CrossRef] [Google Scholar]
- Arthroscopic and low-field MRI (0.25 T) evaluation of meniscus and ligaments of painful knee. J Clin Imaging Sci. 2012;2:24.
- [CrossRef] [Google Scholar]
- The proximal tibio fibular joint. An anatomical study with clinical and pathological considerations. Int Orthop. 1983;7:31-9.
- [CrossRef] [Google Scholar]
- Anatomy of the proximal tibiofibular joint. Knee Surg Sports Traumatol Arthrosc. 2006;14:241-9.
- [CrossRef] [Google Scholar]
- Proximal tibiofibular joint: An often-forgotten cause of lateral knee pain. AJR Am J Roentgenol. 2007;188:W359-66.
- [CrossRef] [Google Scholar]







