Translate this page into:
Hypervascular nodular hepatic involvement in multiple myeloma: A case report
*Corresponding author: Mihyun Park, Department of Radiology, Dankook University Hospital, Cheonan, Chungnam, Korea. chino133@dankook.ac.kr
-
Received: ,
Accepted: ,
How to cite this article: Han Y, Park M. Hypervascular nodular hepatic involvement in multiple myeloma: A case report. J Clin Imaging Sci 2023;13:29.
Abstract
Multiple myeloma (MM) presenting as multiple hypervascular nodular hepatic infiltration is rare. We report a case of liver involvement of MM in 62-year-old woman presenting as multiple hepatic nodules with arterial enhancement and delayed washout. As in our case, the inclusion of MM in the differential diagnosis of multiple hypervascular hepatic nodules should be considered despite of its rarity.
Keywords
Multiple myeloma
Liver
Magnetic resonance imaging
INTRODUCTION
Multiple myeloma (MM) is a malignancy of plasma cells which begin with monoclonal gammopathy of unknown significance to overt plasma cell leukemia and extramedullary myeloma.[1] Autopsy series have shown extraosseous manifestation of myeloma in more than 63% of patients and the liver involvement in MM by autopsy series is relatively common, up to 40% of patients.[2] Hepatic involvement of MM is radiologically underestimated compared with the autopsy findings.[3] Herein, we report the imaging features of the case of MM presenting as multiple hypervascular nodular hepatic lesions.
CASE REPORT
A 62-year-old woman was referred to our hospital with multiple hepatic lesions that were incidentally detected during the evaluation of chest pain due to trauma. She had received medical therapy for diabetes mellitus, and her medical history was otherwise unremarkable. Laboratory examination revealed degradation of hemoglobin level (8.0 g/dL). Other laboratory findings, including aspartate transferase, alanine aminotransferase, and hepatitis B surface antigen were within normal limits. Tumor markers, including alpha-fetoprotein, CA-125, CA 19-9, and carcinoembryonic antigen (CEA), were within the normal range.
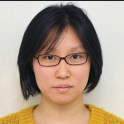
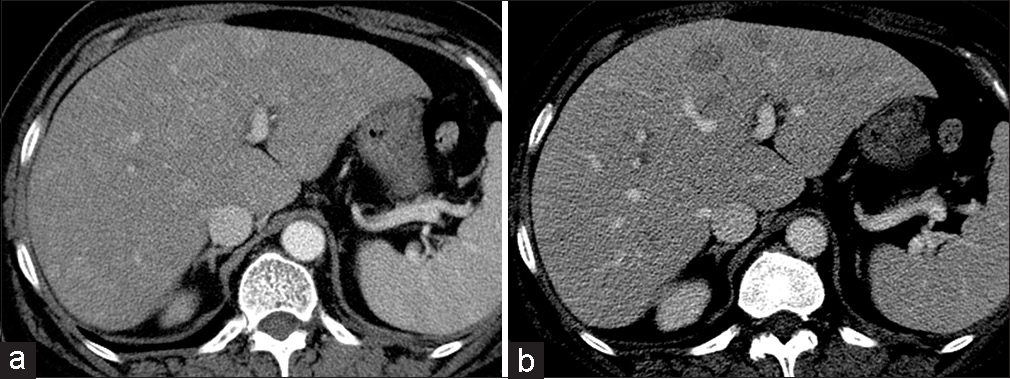
Abdominopelvic computed tomography (CT) revealed multiple nodular arterial enhancing hepatic lesions in the early phase [Figure 1a] with washout enhancement pattern in the delayed phase [Figure 1b]. Magnetic resonance imaging (MRI) of the liver was performed using 3-Tesla MRI scanner (Achieva, Philips Healthcare, Netherlands). A dynamic enhancement study was performed using Gd-EOB-DTPA (Primovist). The innumerable well-defined nodular lesions showed hypointensity relative to the background liver tissue on T1-weighted image [Figure 2a]. The hepatic lesions showed enhancement in the arterial phase [Figure 2b] and a washout enhancement pattern in the portal and delayed phase [Figure 2c and d]. In the hepatobiliary phase, the hepatic lesions showed low-signal intensity [Figure 2e]. On T2-weighted images, the hepatic lesions showed hyperintensity [Figure 2f]. The hepatic lesions showed high-signal intensity on diffusion-weighted image and a low apparent diffusion coefficient value [Figure 2g and h]. The hepatic lesions showed no loss of signal on out-of phase versus in-phase images.
- A 62-year-old woman with incidentally detected multiple hepatic lesions. (a) Abdominopelvic computed tomography was revealed the innumerable nodular arterial enhancing hepatic lesions in early phase (b) with washout enhancement pattern in delayed phase.
- A 62-year-old woman with incidentally detected multiple hepatic lesions. (a) On the axial fat-suppressed T1-weighted magnetic resonance (MR) images, the innumerable well-defined nodular lesions showed hypointensity relative to the background liver tissue. (b) Dynamic contrast-enhanced MR images, the hepatic lesions showed arterial enhancement (c-d) and had washout enhancement pattern in portal and delayed phase. (e) On the hepatobiliary phase, the hepatic lesions showed low signal intensity. (f) On the axial fat-suppressed T2-weighted MR images hepatic lesions showed hyperintensity. (g) Diffusion weighted image (DWI) at b-value of 800 s/mm2 reveal high signal intensity. (h) And an apparent diffusion coefficient (ADC) map reveal a low ADC value.
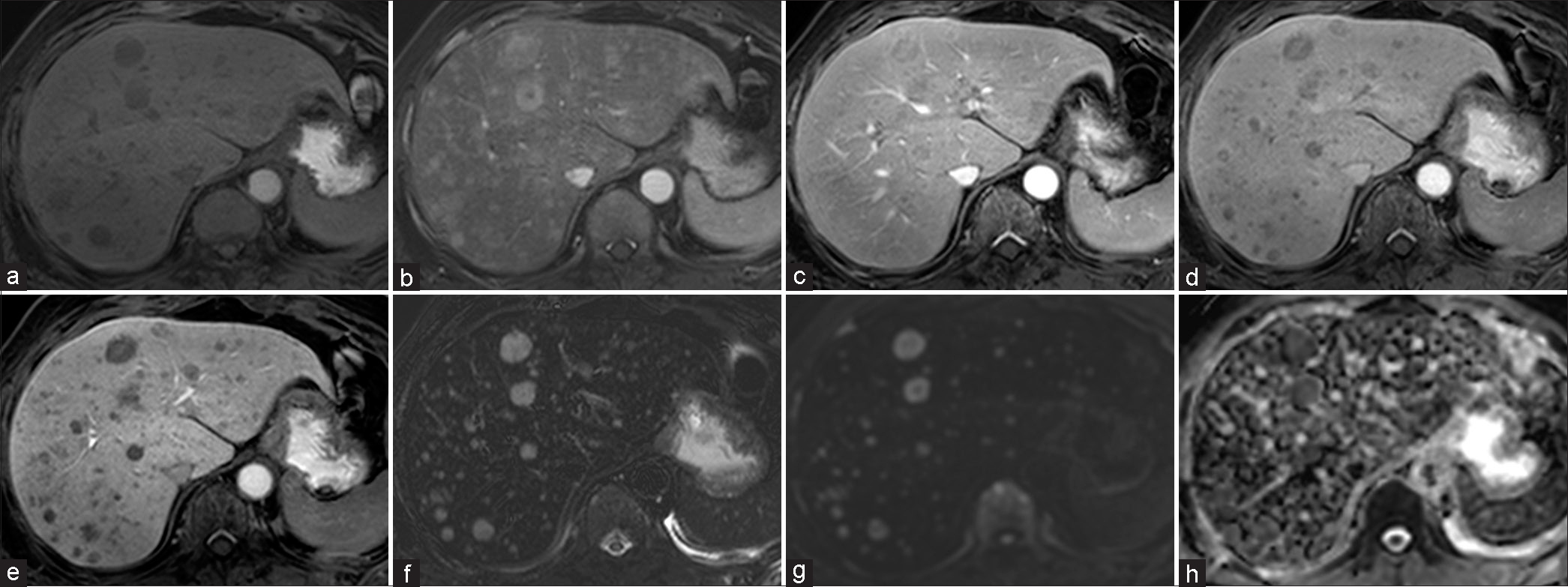
Whole-body positron emission tomography-CT (PET-CT) revealed multiple hypermetabolic lesions (SUV max 8.8) in the liver [Figure 3] and multiple hypermetabolic lesions (SUV max 9.6) along whole skeletal systems. Ultrasound (US) revealed numerous nodular lesions with a target appearance [Figure 4]. A US-guided gun biopsy was performed using an 18-gauge needle, and a pathologic examination revealed a plasma cell neoplasm [Figures 5a-d]. A bone marrow study was performed for precise diagnosis, and plasma cells were counted to be over 30% on the bone marrow smear study, which is compatible with MM. According to the revised International Staging System, additional laboratory examination and DNA analysis were done. Her serum β2-microglobulin level was measured at 11.17 mg/L, exceeding the threshold of 5.5 mg/L and lactate dehydrogenase level was measured at 786 U/L, over the normal range. Despite these elevated levels, the patient’s cytogenetics was categorized as “not high risk,” resulting in a staging classification of 2 for MM. Liver involvement did not impact the staging of MM. Her condition rapidly deteriorated, and she died just 1 month after initial diagnosis.
- A 62-year-old woman with incidentally detected multiple hepatic lesions. Whole-body positron emission tomography-computed tomography revealed multiple hypermetabolic lesions (SUV max 8.8) in liver.
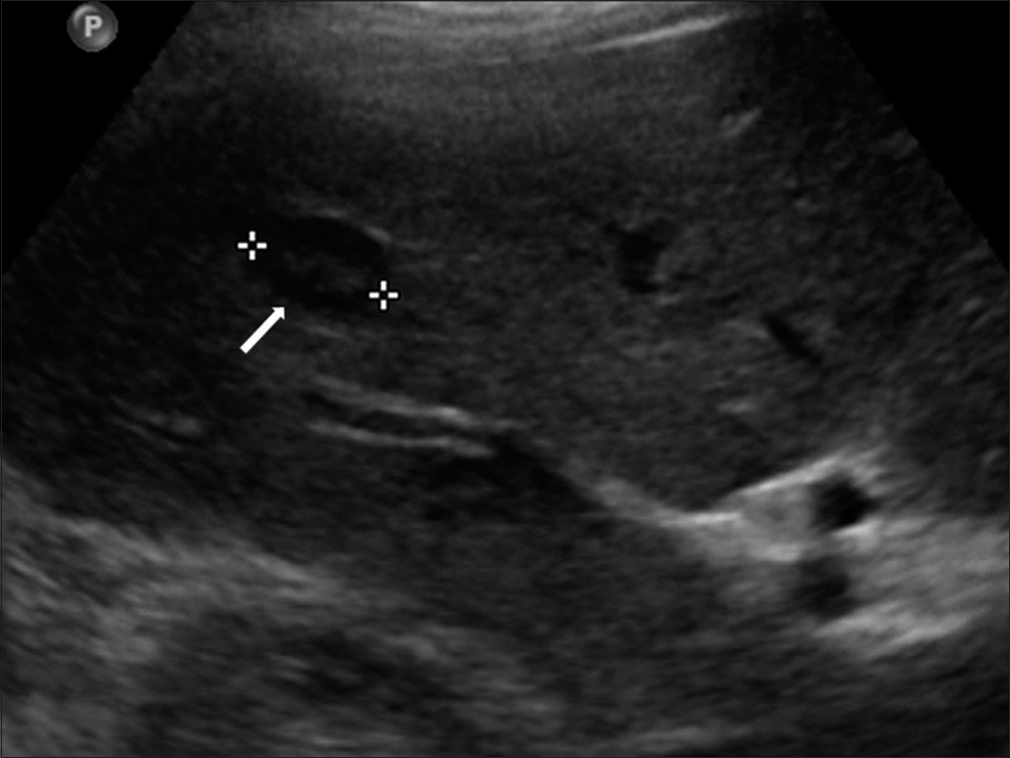
- A 62-year-old woman with incidentally detected multiple hepatic lesions. On the ultrasonography, the hepatic lesion (arrow and stars) was seen target appearance.
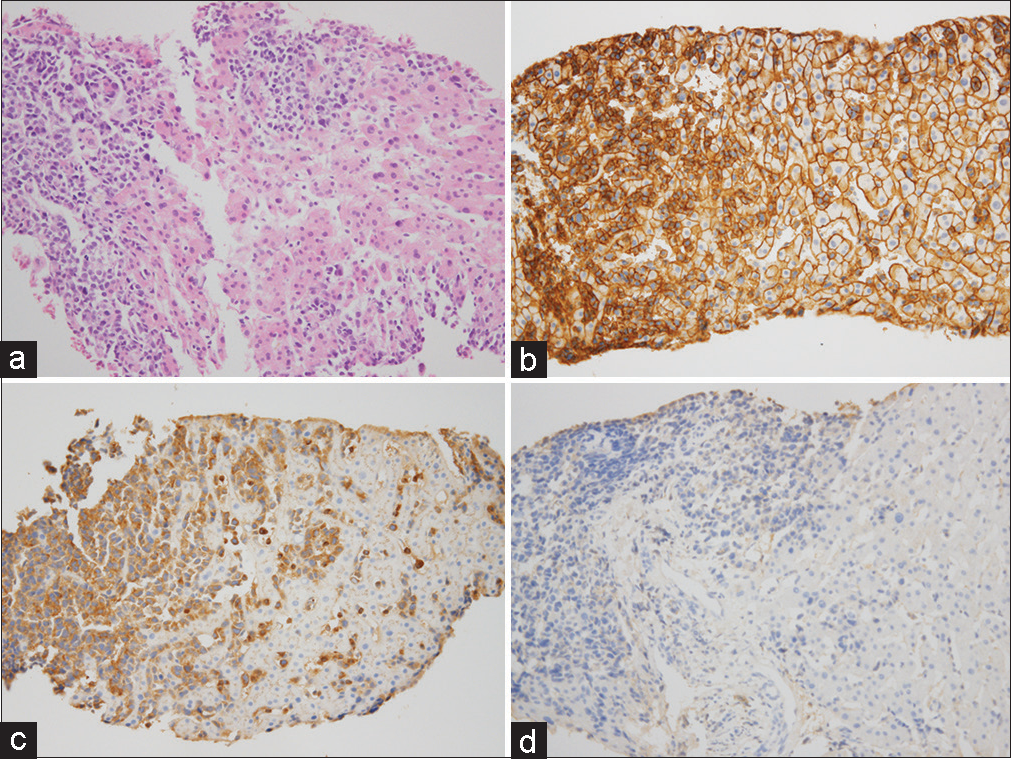
- A 62-year-old woman with incidentally detected multiple hepatic lesions. (a) A core biopsy of hepatic nodule shows infiltration by atypical plasmacytoid cells (Hematoxylin-Eosin stain) (b) and immunohistochemical staining for CD138 confirms plasma cell infiltration. (c) Plasma cells demonstrate kappa light chain restriction by immunohistochemistry for immunoglobulin kappa (d) and lambda light chains.
DISCUSSION
The incidence of MM accounts for 0.9% of all cancers, and autopsy studies have shown extramedullary involvement in approximately 70% of cases.[1] Liver involvement in MM by autopsy series is relatively common in up to 40% of patients and it is most commonly involved with extraosseous myeloma in the abdomen. In the case of liver involvement in MM, the clinical manifestations were not specific. The most common clinical manifestations are hepatomegaly, splenomegaly, jaundice, and ascites. There are two reported different image features of liver involvement of MM in literature: Diffuse and nodular form. The diffuse form presents as hepatomegaly without intrahepatic focal lesion. Moreover, the nodular form presents as single or multiple hepatic nodules.[2]
Nodular form liver involvement of MM is not common. Moreover, imaging findings of the nodular form of liver involvement are non-specific. The nodular form presents a well-defined hypoechoic nodule with or without target appearance in US. These hepatic nodular lesions are hypodense on CT. On MRI, the hepatic nodular lesions are hypointense or hyperintense on T1-weighted images and hyperintense on T2-weighted images. This hepatic nodular lesion is enhanced or not enhanced on CT and MRI. In several cases, these hepatic nodular lesions showed arterial enhancement and delayed washout as in our case.[3-6]
In these cases, differential diagnoses include hepatocellular carcinoma, hepatic adenoma, and hypervascular metastases such as melanoma, neuroendocrine tumor, renal cell carcinoma, and thyroid carcinoma. The hepatic nodular lesion shows little or FDG uptake at PET.[3-8] Therefore, differential diagnosis based on imaging findings alone is difficult. However, it is important to recognize that hepatic manifestation of MM can present as hypervascular nodules. In conjunction with the patient’s clinical presentation, including anemia, renal dysfunction, and altered albumin-globulin ratio, the possibility of MM should be considered.
CONCLUSION
We present that a case of hepatic manifestation of MM presents as multiple hypervascular nodules with arterial enhancement and delayed washout. This case suggests the inclusion of MM in the differential diagnosis of multiple hypervascular hepatic nodules.
Declaration of patient consent
The Institutional Review Board (IRB) permission obtained for the study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Multiple myeloma epidemiology and survival: A unique malignancy. Semin Oncol. 2016;43:676-81.
- [CrossRef] [PubMed] [Google Scholar]
- Liver involvement in multiple myeloma. Clin Lymphoma Myeloma. 2007;7:538-40.
- [CrossRef] [PubMed] [Google Scholar]
- Liver involvement by multiple myeloma presenting as hypervascular focal lesions in a patient with chronic hepatitis B infection. BJR Case Rep. 2016;2:20150013.
- [CrossRef] [PubMed] [Google Scholar]
- Extraosseous myeloma of liver mimicking multifocal hepatocellular carcinoma where a distinction has to be made: Two case reports. Hong Kong Med J. 2023;29:66-9.
- [CrossRef] [PubMed] [Google Scholar]
- A pictorial review on extraosseous manifestations of multiple myelomas. J Korean Soc Radiol. 2011;64:567-75.
- [CrossRef] [Google Scholar]
- Nodular extramedullary multiple myeloma: hepatic involvement presenting as hypervascular lesions on CT. Ann Acad Med Singap. 2011;40:329-31.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging features of multiple myeloma extramedullary lesions in the liver with 18F-FDG PET/CT, contrast-enhanced CT and MRI. Diagnostics. 2019;9:179.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple liver nodules mimicking metastatic disease as initial presentation of multiple myeloma. Case Rep Hematol. 2018;2018:7954816.
- [CrossRef] [PubMed] [Google Scholar]







