Translate this page into:
Back to Basics – ‘Must Know’ Classical Signs in Thoracic Radiology
Address for correspondence: Dr. Athiyappan Kumaresh, Department of Radiology, Sri Ramachandra Medical College and Hospital, Chennai, Tamil Nadu, India. E-mail: drkumaresha@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
There are a few signs in radiology which are based on many common objects or patterns that we come across in our routine lives. The objective behind the association between such common objects and the corresponding pathologies is to make the reader understand and remember the disease process. These signs do not necessarily indicate a particular disease, but are usually suggestive of a group of similar pathologies which will facilitate in the narrowing down of the differential diagnosis. These signs can be seen in different imaging modalities like plain radiograph and computed tomography. In this essay, we describe 24 classical radiological signs used in chest imaging, which would be extremely helpful in routine clinical practice not only for radiologists but also for chest physicians and cardiothoracic surgeons.
Keywords
Chest
computed tomography
signs
thoracic radiography
X-ray

INTRODUCTION
Radiological signs are classical and distinctive abnormalities, characteristic of a disease or a group of similar pathologies which can be seen either on a plain radiograph or on a computed tomography (CT) scan. These signs are generally based upon and associated with common objects and patterns that we come across in our routine lives. The objective behind establishing such an association is to help the reader understand and memorize their appearance and characteristics. The familiarity and application of these signs can facilitate in narrowing down the differential diagnosis and timely management of the disease. The knowledge of these signs is helpful to residents and practitioners across various streams like radiology, internal medicine, chest medicine, and cardiothoracic surgery. The aim of this essay is to serve as a ready reference guide in the field of chest imaging.
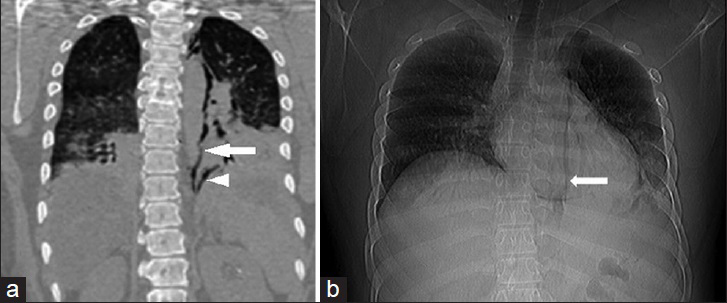
Air crescent sign
Air crescent sign appears as a crescent of air surrounding a soft-tissue mass in a pulmonary cavity and can be seen in both plain X-ray and CT scan [Figure 1]. Though it is characteristic of invasive pulmonary aspergillosis, it can also be seen in cavitating neoplasms, lung abscesses, and infections. This sign is considered a good marker of immune activity as it is seen when the necrotic tissue gets invaded by leukocytes and replaced by air in invasive pulmonary aspergillosis.[1] The other conditions in which air crescent sign can be seen are pulmonary gangrene,[2] pulmonary hematoma,[2] Rasmussen aneurysm in a tuberculous cavity,[2] and lung hydatid.[23] It mimics Monad sign which is seen in patients with aspergilloma in a pulmonary cavity.
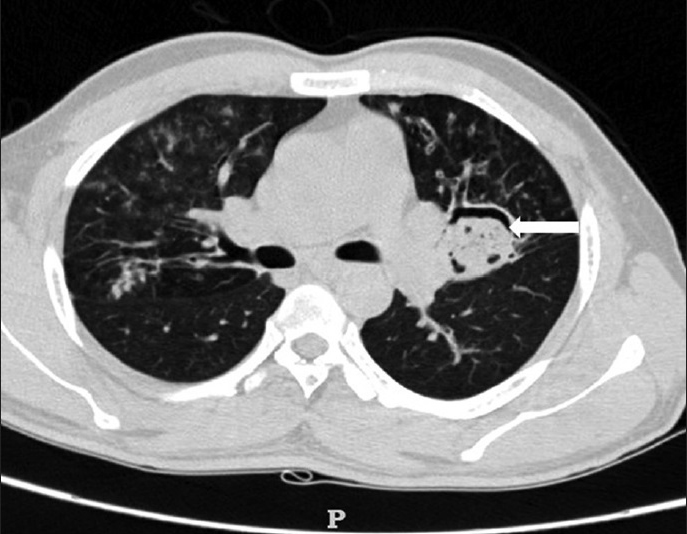
- 29-year-old male presented with 3 weeks history of fever and was diagnosed with invasive aspergillosis. Axial CT image of lung demonstrates a cavity in the left lung with a soft-tissue mass within it and crescent of air (white arrow) around it representing the radiologic sign, air crescent sign.
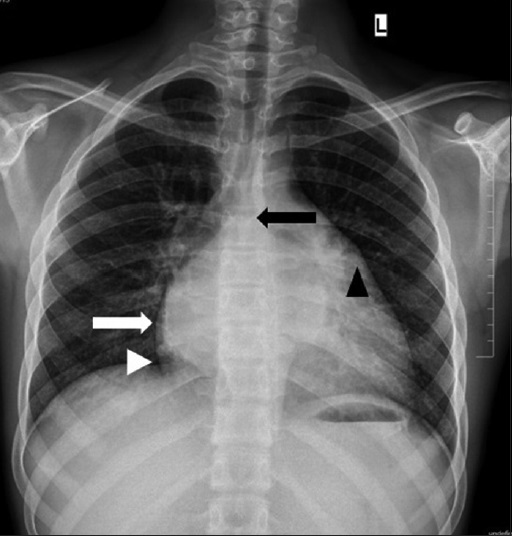
Bulging fissure sign
Bulging fissure sign is seen classically in consolidation caused by Klebsiella pneumoniae infection in the right upper lobe. It occurs due to large exudates produced by the Klebsiella organism which expands the lobe and causes a bulge in the fissure, and can be seen in plain X-ray and CT scan [Figure 2]. Although the main causative organism responsible for this sign is K. pneumoniae, other causes are tuberculosis, pneumococcal pneumonia, Hemophilus influenzae, lung abscesses, and tumors like bronchoalveolar carcinoma.[45]
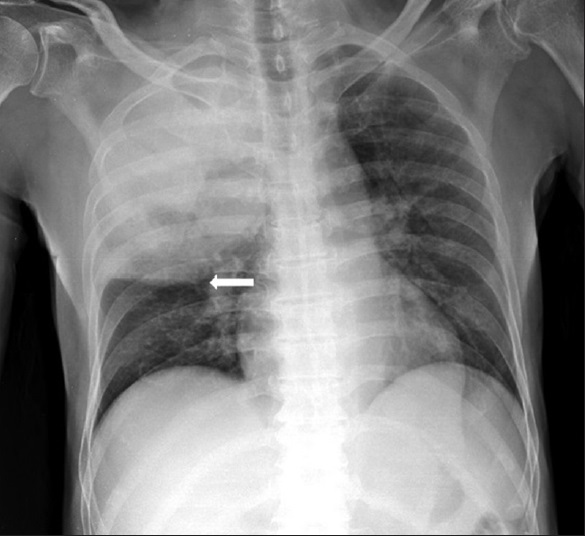
- 35-year-old male presented with 2 weeks history of dyspnea and fever and was diagnosed with pneumonia. Frontal chest radiograph reveals opacified right upper lobe with bulge in the minor fissure (white arrow) representing the radiologic sign, bulging fissure sign.
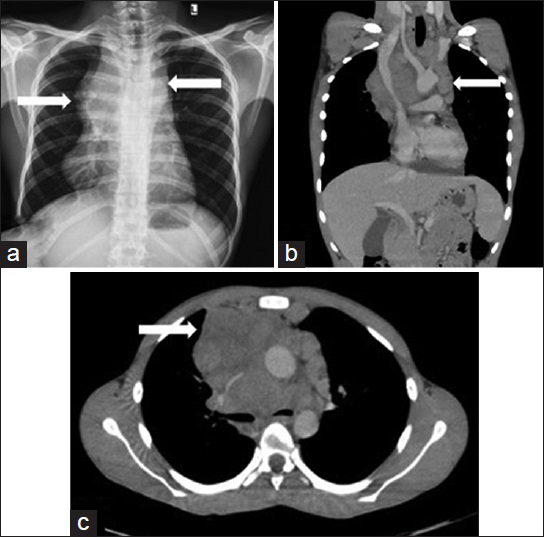
Cervicothoracic sign
This sign was described by Benjamin Felson and based on the Silhouette sign.[6] This sign is seen on plain X-ray and is used to differentiate between an anterior and posterior mass in the superior mediastinum. At the level of the thoracic inlet, the posterior part of the lung extends superiorly to the clavicle compared to the anterior part; hence, any mass when situated in the posterior mediastinum, is completely surrounded by the lung tissue from all sides. This leads to a well-defined cephalic border seen well above the clavicle.[7] In contrast to this, anterior mediastinal masses have ill-defined cephalic margins due to their anatomical contact with the soft tissues of the neck, either at or below the clavicle[8] [Figure 3a–d], indicating a cervicothoracic lesion.
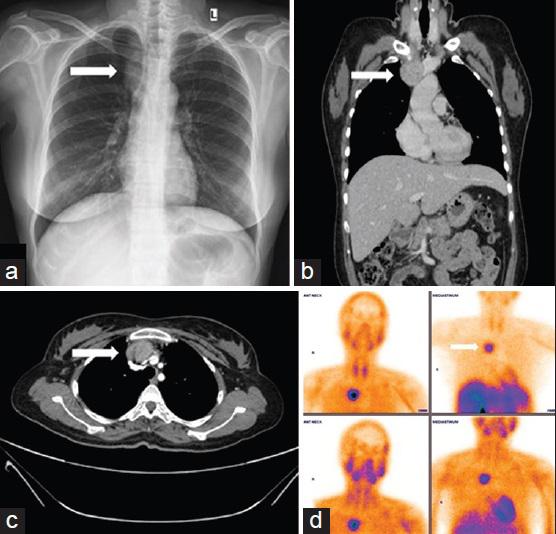
- 32-year-old female presented with recurrent pancreatitis due to ectopic parathyroid adenoma. (a) Frontal radiograph of chest shows opacity in the right paratracheal region extending up to the clavicle with ill-defined upper margins (white arrow) representing anterior mediastinal mass according to the radiologic sign, cervicothoracic sign. (b) Contrast-enhanced coronal image of CT chest confirming the opacity in chest radiograph as an enhancing lesion in the anterior mediastinum in the prevascular compartment (white arrow). (c) Contrast-enhanced axial image of CT chest shows an enhancing lesion in the anterior mediastinum (white arrow). (d) Anterior views of 99mTc MIBI scan show intense uptake in the enhancing lesion (white arrow).
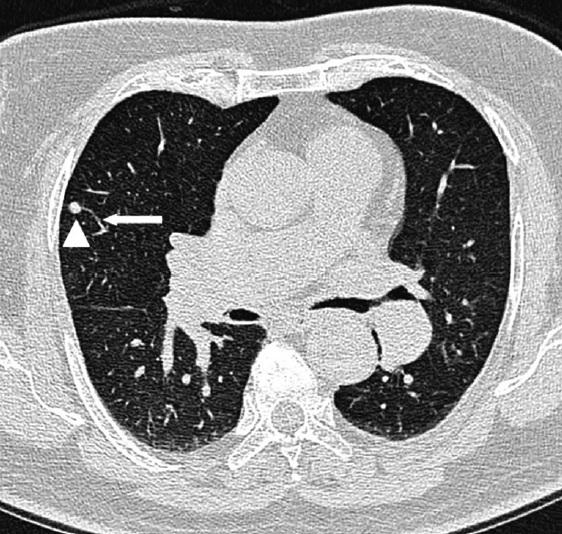
Comet tail sign
In comet tail sign, a subpleural mass produces distortion of the adjacent bronchovascular bundles and appears as a curvilinear opacity extending from the subpleural mass toward the ipsilateral hilum as seen on CT scan, thus resembling a comet tail [Figure 4]. This round atelectasis is associated with pleural effusion or pleural thickening and is seen in approximately 70% of asbestos-related pleural disease.[9] The other uncommon causes are chronic pleural infections like tuberculosis, congestive heart failure, or pulmonary infarct.[10] Round atelectasis is mostly seen in lower lobes, but can rarely involve other lobes as well. Fine needle aspiration biopsy and/or excision biopsy may be required in equivocal cases to exclude the possibility of neoplasm.[11]
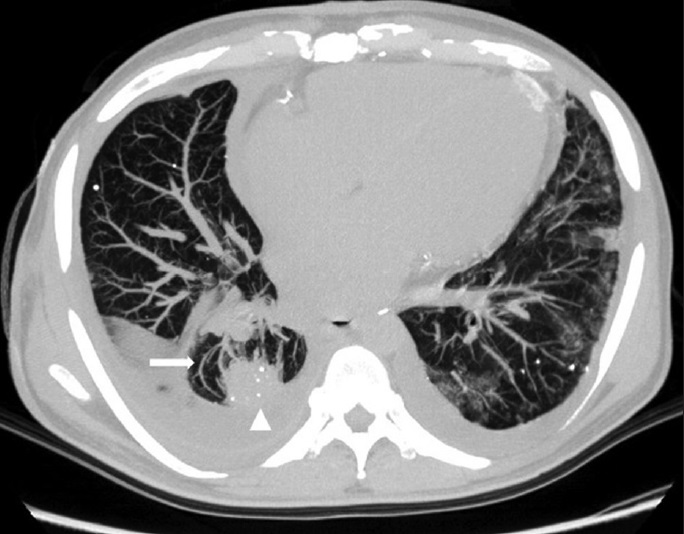
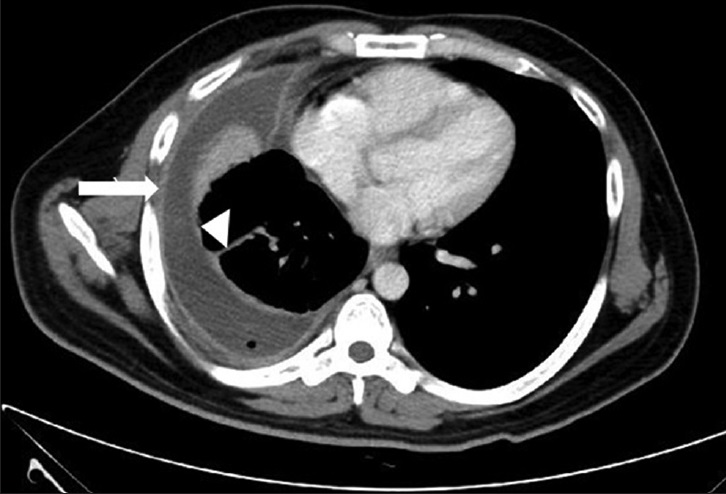
- 57-year-old male presented with shortness of breath was diagnosed with asbestos-related pleural disease. Transaxial CT scan of chest shows a pleural-based mass (white arrowhead) with few curvilinear vessels (white arrow) around it, appearing as the tail of a comet and thus producing the radiologic sign, comet tail sign.
Continuous diaphragm sign
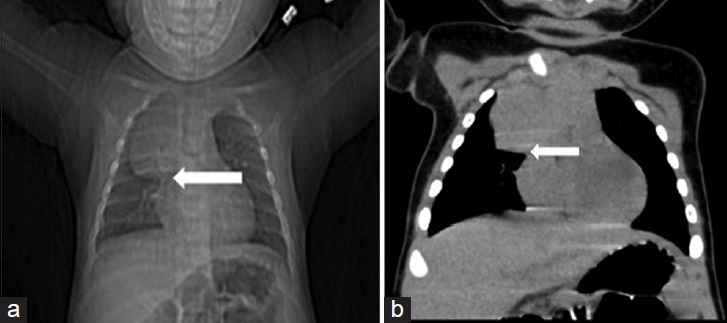
This sign is seen in pneumomediastinum in which air accumulates between the lower border of the heart and the superior part of the diaphragm, which results in complete visualization of the diaphragm in chest X-ray [Figure 5a and b], hence named continuous diaphragm sign.[12] Normally, the central part of the diaphragm is obscured by the heart, and hence is not seen on chest radiographs. Though this sign is commonly seen in pneumomediastinum, it can occasionally be also seen in pneumopericardium.[13] This sign when seen, is a differential tool between pneumomediastinum and pneumothorax.[1214]

- 46-year-old male who met with a road traffic accident (RTA) was diagnosed with pneumomediastinum. (a) Portable chest radiograph shows luceny below the heart border (black arrow) producing the radiologic sign, continuous diaphragm sign. (b) Coronal CT image of chest confirming air below the heart border (black arrow).
Crazy paving sign
Crazy paving sign is seen with a combination of thickened interlobular septa and areas of ground glass opacities (GGO) on high-resolution computed tomography (HRCT) lung [Figure 6],[45] resembling irregular paving stones. Originally noted in pulmonary alveolar proteinosis, the common causes are adult respiratory distress syndrome, infectious causes like Pneumocystis carinii pneumonia, bacterial pneumonia, etc. The rare causes include nonspecific interstitial pneumonia, sarcoidosis, and respiratory bronchiolitis superimposed on interstitial lung disease.[12] Histologically, the thick interlobular septa represent inflammation, while the ground glass opacities are due to intra-alveolar protein-rich fluid in pulmonary alveolar proteinosis.

- 39-year-old male with persistent dry cough for 6 months diagnosed with pulmonary alveolar proteinosis. HRCT lung shows diffuse ground glass opacities with thick interlobular septa in both lungs representing the radiologic sign, crazy paving sign.
CT halo sign
Halo sign is a circular mass or a consolidation surrounded by ground glass opacities [Figure 7]. It was first reported by Kuhlman et al., in 1985 in a case of pulmonary aspergillosis indicating hemorrhagic nodules. Various diseases produce different histological features leading to the formation of a halo. For example, in cases of invasive aspergillosis, halo represents hemorrhage,[15] whereas in cases of carcinoma, the same represents lepidic spread of tumor. The appearance of halo sign on CT has been mostly assessed to be an indication of pulmonary hemorrhage, but it is also seen in various infections and inflammatory and neoplastic conditions. It is associated with fungal infections like invasive aspergillosis, Pneumocystis jiroveci pneumonia, and candidiasis, bacterial infections like TB, Nocardia, and Legionella, viral infections like cytomegalovirus and herpes, inflammatory conditions like Wegener's granulomatosis, vascular causes like infarct, and neoplastic conditions like metastatic tumor, Kaposi sarcoma, bronchioloalveolar carcinoma, and adenocarcinoma. Although nonspecific, the presence of the halo requires detailed history, thorough clinical evaluation, and correlation with laboratory and radiological investigations to narrow down the differential diagnosis.
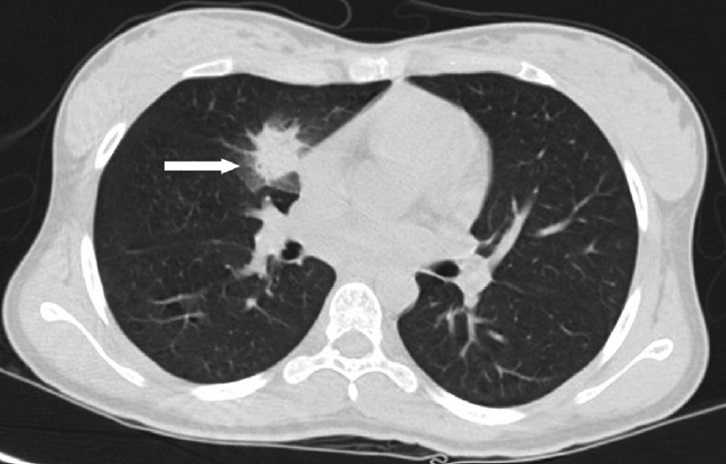
- 40-year-old male with 1 month history of dry cough and diagnosed with invasive aspergillosis. Axial non-contrast CT scan of chest shows a spiculated nodule in the right middle lobe with surrounding ground glass opacities seen as halo (white arrow) resulting in the radiologic sign, CT halo sign.
Deep sulcus sign
This sign is seen in supine chest radiographs of pneumothorax in which air accumulates in the lateral costophrenic angle, which appears lucent and deep when compared to the other costophrenic angle [Figure 8]. This sign is visualized in supine position when air accumulates in the nondependent parts of the pleura, i.e. anterior and basal parts, in contrast to the upright position in which air accumulates in the apex of the pleura. Once visualized, one should always look for other signs of pneumothorax in cases of major trauma, neonates, and ICU patients to avoid errors.[16] False deep sulcus sign can be seen in chronic obstructive pulmonary disease.[17]

- 52-year-old female with sudden-onset chest pain and diagnosed with right pneumothorax. Frontal radiograph of chest shows right pneumothorax causing mild depression of the right costophrenic angle (white arrow) producing the radiologic sign, deep sulcus sign.
Double density sign
Left atrial enlargement appears as a curvilinear soft-tissue density in the right retrocardiac region in chest radiographs. This curvilinear density along with the right atrium opacity represents the double density sign [Figure 9]. In severe cases, this curvilinear density of the left atrium may even project beyond the right atrium border which is called the atrial escape.[1819] Once visualized, one should also look for other signs of left atrial enlargement like carinal widening, elevation of the left main bronchus, and enlargement of the left atrial appendage.
- 23-year-old female with difficulty in breathing and diagnosed with mitral valve disease. PA chest radiograph shows double density behind the right heart with two separate borders due to right atrium (white arrowhead) and left atrium (white arrow) producing the radiologic sign, double density sign.
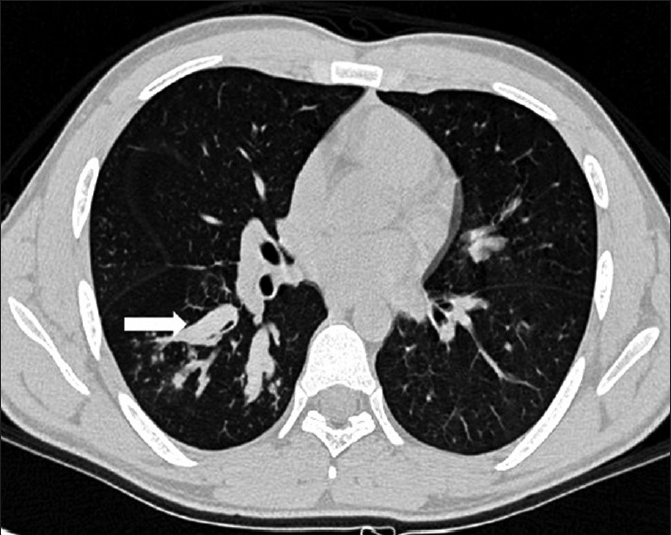
Feeding vessel sign
This sign consists of a pulmonary artery leading to the center of the nodule signifying the hematogenous origin of the nodule [Figure 10]. It is seen in CT scan of the chest, and is a strong indication of septic embolism and is seen in approximately 67–100% of septic embolus cases.[20] This can also be seen in secondaries to the lung, hemorrhagic nodules, pulmonary vasculitis, pulmonary infarct, and pulmonary arteriovenous malformation.[2122] The feeding vessel may even rotate around the nodule instead of entering the center of the nodule, which is seen clearly on multiplanar images or may even represent a pulmonary vein.[23]
- 42-year-old female with neck swelling and diagnosed with carcinoma of thyroid. HRCT lung shows a small nodule (white arrowhead) in the right middle lobe with a feeding vessel (white arrow) to it producing the radiologic sign, feeding vessel sign.
Finger-in-glove sign
This sign which can be seen in plain X-ray and CT scans of the chest appears as a tubular soft-tissue density opacity radiating from the hilum to the lung periphery and, thus, mimicking fingers-in-a glove [Figure 11]. It occurs due to impaction of mucus in the bronchi, which results in bronchiectasis surrounded by aerated lung. This sign was first described in 1978 by Mintzer et al., in a case of allergic bronchopulmonary aspergillosis (ABPA).[24] It occurs due to two main pathologies – obstructive and non-obstructive. Obstructive pathologies comprise benign tumors like hamartoma, lipoma, etc., and malignant neoplasms like bronchogenic carcinoma or metastases, while congenital causes include bronchial atresia, etc. The non-obstructive pathologies are ABPA and cystic fibrosis. ABPA is more common in asthmatic patients with Aspergillus infection. Mucoid impaction in cystic fibrosis occurs due to thick mucus secretions and mucociliary dysfunction.
- 44-year-old female presented with acute exacerbation of asthma and was diagnosed with allergic bronchopulmonary aspergillosis. HRCT lung shows dilated and mucus-filled bronchi in the right lung appearing as finger in glove (white arrow) producing the radiologic sign, finger-in-glove sign.
Fleishner sign
This sign was first described by Felix Fleishner and it represents dilatation of the proximal pulmonary arteries due to pulmonary embolism [Figure 12].[25] It is seen on both plain X-ray and CT scan of chest. This could be either due to large embolus enlarging the pulmonary artery or increased pressure in pulmonary arterial circulation.[26]
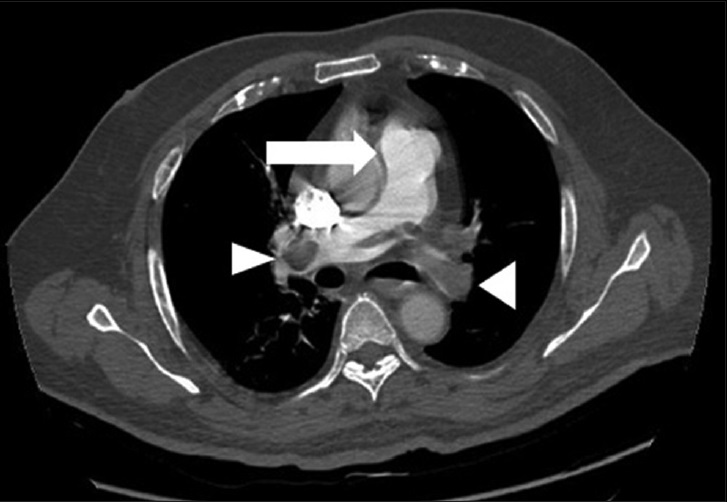
- 54-year-old male presented with acute chest pain and was diagnosed with pulmonary thromboembolism. Axial contrast-enhanced CT scan of chest shows dilated central pulmonary artery (white arrow) producing the radiologic sign, Fleishner sign, secondary to distal emboli (white arrowheads).
Hampton's hump
It was first described by Aubrey Otis Hampton in 1940[27] and was even named after him. It is also known as the melting sign owing to its resolution resembling a melting ice cube.[28] This sign is a classical radiographic feature of pulmonary embolism, which represents wedge-shaped area of pulmonary infarction secondary to embolus as seen on plain X-ray or CT scan [Figure 13]. The accurate and timely diagnosis of this disease, which carries a mortality rate of 26–30% in untreated patients[29] and a rate of 2–8% even in treated patients,[30] is extremely important.
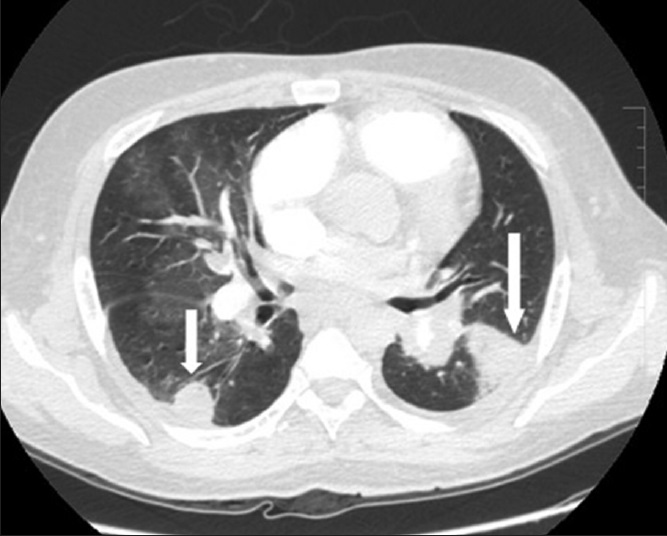
- 54-year-old male with chronic pulmonary thromboembolism. Contrast-enhanced CT chest shows wedge-shaped areas of opacities in the right and left lower lobes representing infarcts (white arrows) due to pulmonary embolism produce the radiologic sign, Hampton's Hump.
Hilum overlay sign
This sign was also described by Benjamin Felson[31] and it helps to determine whether an opacity seen on chest X-ray is within the hilum or anterior or posterior to it. It is based on the Silhouette sign. If opacity is situated within the hilum, there will not be any air between the margins of the hilar structures, which will in turn lead to obscuration of the opacities from the proximal pulmonary artery. This will appear as opacity inseparable from hilar structures, confirming its location to be within the hilum [Figure 14a–c]. On the other hand, if a mass produces opacity through which hilar vessels are clearly seen, then the mass can be said to be located anterior or posterior to the hilum [Figure 15a and b].
- 50-year-old asymptomatic male came for routine health check-up and was subsequently diagnosed with Hodgkin's lymphoma of nodular sclerosing type. (a) PA radiograph of chest shows lobulated margins (white arrows) of the mediastinum with obscuration of the hilar vessels producing the radiologic sign, hilum overlay sign. (b) Coronal and (c) axial images of contrast-enhanced CT scan of the chest show large nodal masses in the mediastinum (white arrows) obscuring the hilar vessels.
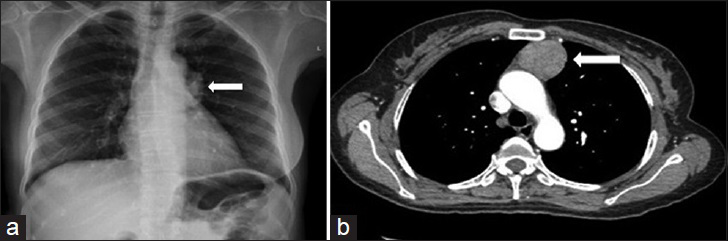
- 46-year-old female presented with history of cough for 2 months and was diagnosed with thymoma. (a) PA chest radiograph shows a round opacity (white arrow) projecting over the left hilum through which the hilar structures can be seen clearly, implying the opacity lies either anterior or posterior to the hilum and showing the radiologic sign, hilum overlay sign. (b) Contrast-enhanced axial image of CT scan of the chest confirms the anterior location of the mass (white arrow).
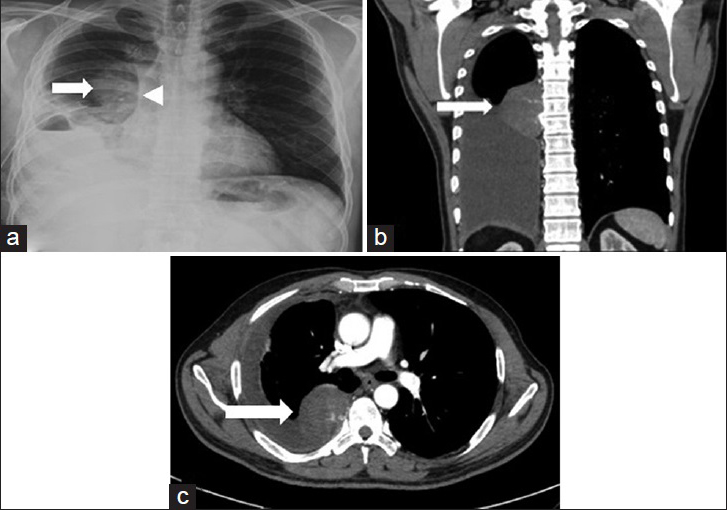
Juxtaphrenic sign
This sign was first described by Katten et al., in 1980, and hence, it is also known as the Katten's sign.[32] It is seen on chest radiograph and appears as a peak arising from the medial part of the diaphragm [Figure 16]. This peak is caused most commonly by traction from the inferior accessory fissure,[33] but can also be caused by major fissure or inferior pulmonary ligament. It is seen in upper lobe collapse, middle lobe collapse, and in cases of post upper lobectomy.[34]

- 63-year-old male presented with chronic cough and old history of pulmonary tuberculosis. PA chest radiograph shows fibrosis in the right upper lobe (white arrowhead) with a small peak (white arrow) arising from the right hemidiaphragm producing the radiologic sign, juxtaphrenic sign.
Knuckle sign
It appears as abrupt tapering of a pulmonary artery (white arrow) secondary to embolus [Figure 17]. It is seen on a CT scan. Once detected, one should look for other signs of pulmonary thromboembolism like Fleishner sign, Westermark sign, etc., and determine the extent and severity of pulmonary thromboembolism.

- 67-year-old female presented with chest pain and was diagnosed with pulmonary thromboembolism. Contrast-enhanced CT scan of chest shows abrupt tapering of a pulmonary artery (white arrow) secondary to embolus and thus producing the radiologic sign, knuckle sign.
Naclerio's v sign
This sign is a common presentation in pneumomediastinum in which there occurs a lucency in the shape of “V” which is caused by air outlining the medial part of the left hemidiaphragm and lower mediastinal border [Figure 18a and b], and can be seen both on X-ray and CT scan. Although this sign was first described by Naclerio in cases of spontaneous esophageal rupture,[35] this sign is not specific for esophageal rupture.[36]
- 46-year-old male presented with severe chest pain after an episode of vomiting and was diagnosed with esophageal tear resulting in pneumomediastinum. (a) Coronal image of CT chest shows air outlining the left hemidiaphragm (white arrowhead) and left lateral wall of aorta (white arrow) appearing as V and thus producing the radiologic sign, Naclerio's V sign. (b) Scanogram shows air outlining the left lateral wall of the aorta (white arrow).
Polo mint sign
This sign is seen in a blood vessel in a contrast-enhanced CT scan in which the central filling defects represent the thrombus while the peripheral rim appears as a hyperattenuating area due to contrast which mimics the polo mint [Figure 19a]. This could be seen in any vessel with thrombus, such as pulmonary artery, superior vena cava [Figure 19b], or portal vein.[37]
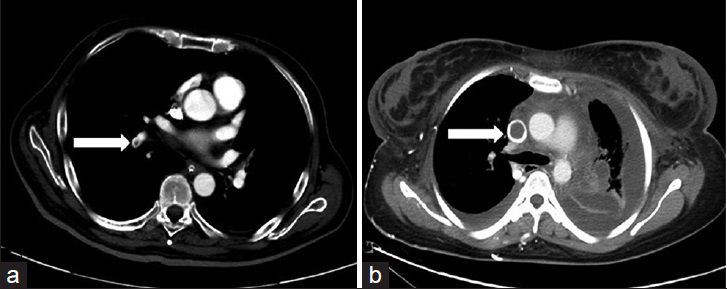
- (a) 62-year-old male presented with chest pain and was diagnosed with pulmonary thromboembolism. Contrast-enhanced axial image of CT chest shows central embolus with peripheral contrast in a right pulmonary artery branch (white arrow) producing the radiologic sign, polo mint sign. (b) 38-year-old female with chronic renal failure presented with swelling of whole body and was diagnosed with superior vena cava obstruction due to thrombus. Contrast-enhanced CT scan of chest shows central embolus with peripheral contrast in the superior vena cava (white arrow) producing the radiologic sign, polo mint sign.
Signet ring sign
This sign appears as a round area of soft-tissue attenuation abutting a circle of lucent air in HRCT of lungs [Figure 20] and, thus, mimicking a ring. This soft-tissue attenuation represents a pulmonary artery lying adjacent to the dilated bronchi and is seen in cases of bronchiectasis.[38] Bronchiectasis is defined as an irreversible and abnormal dilatation of the bronchus[38] and can be classified as cylindrical, varicose, and cystic types on the basis of morphology. Bronchiectasis is diagnosed when the dilated bronchus measures more than 50% of the associated pulmonary artery, along with other findings like bronchial wall thickening, visualization of bronchi within 1 cm of the pleura, and non-tapering bronchi.[38] False-positive increase in the bronchoarterial ratio can be seen with increased altitude on HRCT.[39]

- 54-year-old male presented with difficulty in breathing and was diagnosed with asthma. HRCT of lung shows dilated bronchi (white arrows) lying adjacent to the pulmonary artery (white arrowhead) producing the radiologic sign, signet ring sign.
Silhouette sign
This sign is present when an intra-thoracic lesion touches the border of the heart, aorta, or diaphragm and that border is obliterated on the X-ray [Figure 21a–c].[31] Conversely, an object which is not neighboring these structures will not obliterate their border [Figure 22a–c].[831] This absence or presence of silhouette helps in localizing the lesion anatomically. This is based on the fact that variation in the densities between nearby structures results in different radiological shadows.[8]
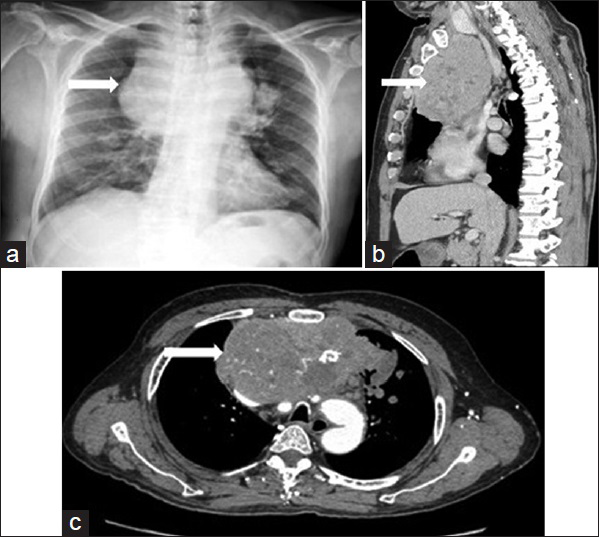
- 44-year-old male presented with swelling of face and neck since 2 months and was diagnosed with spindle cell thymoma. (a) Frontal chest radiograph shows a large mass in the mediastinum (white arrow) silhouetting the right upper mediastinal border, suggesting anterior location of the mass in the mediastinum and hence positive silhouette sign. (b) Sagittal and (c) axial contrast-enhanced CT shows a large heterogeneous mass (white arrow) in the anterior mediastinum causing posterior displacement of the superior vena cava, aortic arch and its branches. Foci of calcification and areas of hypervascularity are seen within the mass. Kinking of the aortic arch is seen.
- 43-year-old male presented with heaviness in chest since 3 months and was diagnosed with solitary fibrous tumor of pleura. (a) Frontal chest radiograph shows right pleural effusion with a homogenous opacity (white arrow) in the right hilar region. There is no loss of silhouette of cardiac border (white arrowhead) suggesting posterior location of the lesion. (b) Coronal and (c) axial contrast-enhanced CT shows a homogenous pleural-based mass (white arrow) in the right paravertebral region with right pleural effusion confirming the findings made in chest radiograph.
The lesions in the right middle lobe and lingula usually obliterate the right and left borders of the heart, respectively. Similarly, the lower lobe lesion obliterates the diaphragm and descending aorta. Lesions in the anterior segment of the right upper lobe obliterate the right paratracheal stripe, whereas lesions in the apicoposterior segment of the left upper lobe obliterate the aortic knuckle.
This term was first described by Dr. Benjamin Felson in 1950.[31] It is also known as the loss of outline sign or loss of silhouette sign.[40]
Split pleura sign
Split pleura sign is seen in CT scan in cases of empyema which most commonly occurs due to bacterial pneumonia. There occurs fluid accumulation in the pleural space, which causes fibrin coating of the inner visceral and outer parietal layers of pleura. This results in separation, thickening, and increased enhancement of pleural layers, producing split pleura sign [Figure 23]. Empyema causes extrapleural fat stranding and thickening of extrapleural soft tissues.[41] Even though these pleural changes are commonly seen in empyema, similar changes can also be visualized in conditions like mesothelioma, hemothorax, and post lobectomy.[4243]
- 47-year-old male presented with high-grade fever and cough since 2 months. Contrast-enhanced axial section CT scan of chest shows thick and enhancing outer parietal (white arrow) and inner visceral right pleural layer (white arrowhead) representing the radiologic sign, split pleura sign.
Thymic notch sign
This sign is seen in newborn chest radiographs in which the inferior border of the thymus forms a notch with the heart border [Figure 24a and b].[10] Other signs seen in the thymus are the wave sign, which is the gentle undulations seen on the right border of thymus due to costochondral junction impressions, and the sail sign, which is a triangular-shaped inferior margin of the thymus mostly seen on the right side.[10]
- 5-month-old kid presented with cough and fever since 1 month. (a) AP chest radiograph shows notch between right inferior border of thymus and right border of heart, indicating the radiologic sign, thymic notch sign. (b) Coronal CT study of chest confirms the findings made on chest radiograph.
Visceral pleural white line
This is seen in pneumothorax in which there occurs separation of the visceral and parietal layers of the pleura by air, leading to visualization of a white line of visceral pleura in a plain X-ray [Figure 25]. Hence, it is called the visceral pleural white line. A skin fold might mimic visceral pleural white line; however, when traced, it tracks outside the lung field.
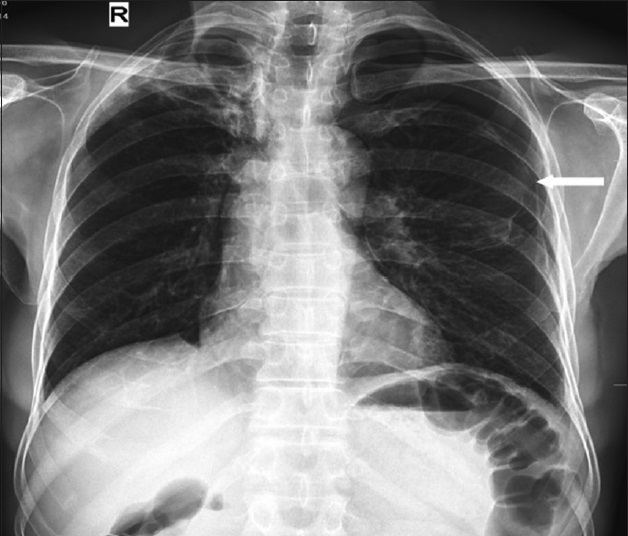
- 38-year-old male presented with chest pain and was diagnosed with pneumothorax. PA chest radiograph shows white line of visceral pleura sign (white arrow) in left hemithorax representing the radiologic sign, visceral pleural white line sign.
Westermark sign
Westermark sign is defined as a focal area of oligemia distal to an occluded pulmonary artery [Figure 26]. This area appears hypoattenuated compared to the normal lung and can be seen on both X-ray and CT scan. This sign was first described by Neil Westermark in the year 1938.[44] This sign is quite rare and seen in 2% of patients with pulmonary thromboembolism.[45] It occurs due to a combination of obstruction of pulmonary artery by embolus and vasoconstriction occurring in the hypoxic lung.[28]
![67-year-old female presented with chest pain and was diagnosed with pulmonary thromboembolism. Contrast-enhanced CT scan of chest in the lung window shows lucency (white arrow) indicating oligemia distal to the occluded pulmonary artery [Figure 17, white arrow], and thus represents the radiologic sign, Westermark sign.](/content/12/2015/5/1/img/JCIS-5-43-g027.png)
- 67-year-old female presented with chest pain and was diagnosed with pulmonary thromboembolism. Contrast-enhanced CT scan of chest in the lung window shows lucency (white arrow) indicating oligemia distal to the occluded pulmonary artery [Figure 17, white arrow], and thus represents the radiologic sign, Westermark sign.
CONCLUSION
These signs are compiled with an intention to provide a comprehensive review of the scientific basis behind these signs and their importance in thoracic imaging. With a thorough understanding of these signs in conjunction with the relevant medical history, we can have a systematic approach to the problems in thoracic imaging, which can assist in a proper patient management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2015/5/1/43/161977
REFERENCES
- The air crescent sign caused by Staphylococcus aureus lung infection in a neutropenic patient with leukemia. Ann Intern Med. 1992;116:910-1.
- [Google Scholar]
- Bulging (sagging) fissure sign in Hemophilus influenzae lobar pneumonia. South Med J. 1978;71:1452-3.
- [Google Scholar]
- High-resolution CT of bronchioloalveolar carcinoma. AJR Am J Roentgenol. 1992;159:275-7.
- [Google Scholar]
- More chest roentgen signs and how to teach them. Annual Oration in memory of L. Henry Garland, M.D., 1903-1966. Radiology. 1968;90:429-41.
- [Google Scholar]
- Approach to the chest radiograph. In: The core curriculum: Cardiopulmonary Imaging. Philadelphia, PA: Lippincott Williams and Wilkins; 2004. p. :66.
- [Google Scholar]
- Localization of intrathoracic lesions. In: Chest Roentgenology. Philadelphia, PA: WB Saunders Company; 1973. p. :22-38.
- [Google Scholar]
- The continuous diaphragm sign: A newly-recognized sign of pneumomediastinum. Clin Radiol. 1973;24:337-8.
- [Google Scholar]
- The chest wall, pleura and diaphragm. In: Grainger RG, Allison DJ, Adam A, Dixon AK, eds. Grainger and Allison's Diagnostic Radiology: A Textbook of Medical Imaging (4th ed). New York: Churchill Livingstone; 2001. p. :333-7.
- [Google Scholar]
- Left atrial dimension on the frontal thoracic radiograph: A method for assessing left atrial enlargement. AJR Am J Roentgenol. 1978;130:251-5.
- [Google Scholar]
- Radiography of acquired heart disease. In: Webb WR, Higgins CB, eds. Thoracic Imaging: Pulmonary and Cardiovascular Radiology (2nd ed). Philadelphia, PA: Lippincott Williams and Wilkins; 2011. p. :722-3.
- [Google Scholar]
- Nonneoplastic paranchymal lung disease. In: CT and MRI of the Whole Body (5th ed). Philadelphia, PA: Mosby, Elseiver; 2009. p. :863-926.
- [Google Scholar]
- Computed Tomography and Magnetic Resonance of the Thorax. (4th ed). Philadelphia, PA: Lippincott Williams and Wilkins; 2007. p. :583-5.
- [Google Scholar]
- High-resolution MDCT of pulmonary septic embolism: Evaluation of the feeding vessel sign. AJR Am J Roentgenol. 2006;187:623-9.
- [Google Scholar]
- The Fleischner Society: A 30th anniversary retrospective. Radiology. 2000;214:631-2.
- [Google Scholar]
- Pulmonary embolism: Roentgenographic and angiographic considerations. AJR Am J Roentgenol Radium Ther Nucl Med. 1963;89:333-42.
- [Google Scholar]
- Correlation of postmortem chest teleroentgenograms with autopsy findings with special reference to pulmonary embolism and infarction. AJR Am J Roentgenol. 1940;43:305-26.
- [Google Scholar]
- Pulmonary thromboembolic disease. In: Thoracic Imaging: Pulmonary and Cardiovascular Radiology (2nd ed). Philadelphia, PA: Lippincott Williams and Wilkins; 2011. p. :656-7.
- [Google Scholar]
- The mortality of untreated pulmonary embolism in emergency department patients. Ann Emerg Med. 2005;45:302-10.
- [Google Scholar]
- Venous thromboembolism and hypercoagulable states. In: Griffin BP, ed. Manual of Cardiovascular Medicine (4th ed). Philadelphia, PA: Lippincott Williams and Wilkins; 2013. p. :446-58.
- [Google Scholar]
- Localization of intrathoracic lesions by means of the postero-anterior roentgenogram; The silhouette sign. Radiology. 1950;55:363-74.
- [Google Scholar]
- Juxtaphrenic peak in upper and middle lobe volume loss: Assessment with CT. Radiology. 1996;198:143-9.
- [Google Scholar]
- Prevalence of the juxtaphrenic peak after upper lobectomy. AJR Am J Roentgenol. 2001;177:869-73.
- [Google Scholar]
- The V sign in the diagnosis of spontaneous rupture of the esophagus (an early roentgen clue) Am J Surg. 1957;93:291-8.
- [Google Scholar]
- Transport of air along sheaths of pulmonic blood vessels from alveoli to mediastinum: Clinical implications. Arch Intern Med. 1939;64:913-26.
- [Google Scholar]
- CT angiography of pulmonary embolism: Diagnostic criteria and causes of misdiagnosis. Radiographics. 2004;24:1219-38.
- [Google Scholar]
- Bronchiectasis: Comparison of preoperative thin-section CT and pathologic findings in resected specimens. Radiology. 1995;195:649-54.
- [Google Scholar]
- Bronchoarterial ratio on thin-section CT: Comparison between high altitude and sea level. J Comput Assist Tomogr. 1997;21:306-11.
- [Google Scholar]
- Lung consolidation, ground glass shadowing, obstructive emphysema, collateral air-drift, mucocoeles, patterns of collapse, lung torsion and herniation. In: Wright FW, ed. Radiology of the Chest and Related Conditions (1st ed). New York: Taylor and Francis; 2002. p. :225-26.
- [Google Scholar]
- Pleural exudates and transudates: Diagnosis with contrast-enhanced CT. Radiology. 1994;192:803-8.
- [Google Scholar]
- Chest radiographic findings in patients with acute pulmonary embolism: Observations from the PIOPED Study. Radiology. 1993;189:133-6.
- [Google Scholar]






