Translate this page into:
Computed Tomography Mimics of Acute Appendicitis: Predictors of Appendiceal Disease Confirmed at Pathology
Address for correspondence: Dr. Vikram S. Dogra, Department of Imaging Sciences, University of Rochester Medical Center, 601 Elmwood Ave, Box 648, Rochester, NY 14642, USA. E-mail: vikram_dogra@urmc.rochester.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Purpose:
Imaging and pathology findings are used to analyze the capability of computed tomography (CT) to distinguish between acute appendicitis and radiological mimickers.
Materials and Methods:
A retrospective review of 5861 patients undergoing abdominopelvic CT from 2000 to 2008 for suspicion of acute appendicitis was performed. Appendix diameter, surrounding inflammation, appendicolith, and location were assessed. Only those cases were included where patients underwent surgery for acute appendicitis on CT findings. Pathology specimens were examined and those indicative of acute appendicitis were identified. Statistical analysis was performed to correlate pathology and CT signs.
Results:
A total of 969 of the 5681 patients were included in the study. Acute appendicitis was verified in 870/969 (89%) cases, while 99/969 (11%) demonstrated either chronic findings (i.e., fibrosis [32%], granulomatous disease [16%], lymphoid hyperplasia [11%]) or no abnormality. In regression models, appendiceal diameter >7 mm (odds ratio [OR] = 3.98, P < 0.0001) and mesenteric fat stranding (OR = 6.04, P < 0.0001) were associated with acute appendicitis. Nearly 87% (754/870) of acute appendicitis cases showed both signs on CT, compared with 53% (52/99) of those with other pathologic finding (P < 0.0001). In cases with non-appendicitis findings, 39% (39/99) had only one of these signs compared with 13% (112/870) of those with acute appendicitis (P < 0.0001).
Conclusion:
Diseases of the appendix other than acute appendicitis may manifest with isolated radiological findings and should be considered as part of the differential diagnosis in cases of borderline acute appendicitis.
Keywords
Abdominal radiology
appendicitis
computed tomography
INTRODUCTION

Acute appendicitis accounts for about one-third of patients presenting to the emergency department with acute abdomen. Surgeons perform around 280,000 appendectomies per year in the United States.[1] Historically, in surgical practice, due to the high morbidity and mortality of appendicitis, a false-negative rate in the range of 20% is tolerated to maintain a high sensitivity in the pre-operative workup.[23] The gradual integration of computed tomography (CT) into the diagnostic algorithm has reduced false-negative appendectomy rates to 1.7% overall[4] and 7% in women.[5] Often an alternative explanation for the clinical symptoms have been identified.
Other than appendicitis, there are many rare diseases, which can affect the appendix. In fact, 4% of post-operative specimens are found to represent some alternative disease. Chronic fibrosis, hyperplasia of lymphoid tissue, neoplasm, inflammatory disease, and other etiologies can affect the appendix. Unfortunately, when these diseases present in an acute form, studies have shown that there are no distinguishing features between these conditions and acute appendicitis. Furthermore, 30-50% of appendiceal neoplasms present clinically as acute appendicitis and share radiographic features.[6–9]
The aim of this study was to analyze the role of CT in distinguishing acute appendiceal disease from other diseases affecting the appendix, and to determine the significance of equivocal findings in chronic appendiceal diseases.
MATERIALS AND METHODS
This study was approved by the institutional review board of the University of Rochester Medical Center. A retrospective review of the records of patients at a tertiary care hospital, who were referred for CT because of a clinical suspicion of acute appendicitis during the study period, January 2000 through July 2008, was performed. The initial CT report of 5861 cases was reviewed by a clinical investigator and patients proceeding to surgery with a radiological diagnosis of acute appendicitis were included in the study. Cases were excluded from the study if the initial CT report did not render a diagnosis of acute appendicitis.
Findings from each patient's CT were recorded. The scans were examined by the radiologist for specific radiologic features, such as appendiceal size greater than 7 mm, presence of adjacent mesenteric fat stranding, presence of appendicolith, and location of the appendix, as well as secondary findings such as lymphadenopathy, cecal changes, and presence of phlegmon or abscess. Subsequent operation notes and pathology reports were reviewed. The postoperative and pathology diagnoses were recorded. A case was categorized by the postoperative and pathologic findings as acute appendicitis or not acute appendicitis. Patients were grouped as cases of acute appendicitis (Group 1) and cases of non-appendicitis or other etiology (Group 2).
Multinomial logistic regression analysis using SAS (version 9.1, SAS Institute Inc. Cary, NC, USA) was then performed to correlate primary imaging signs with final pathological diagnosis. The significant P value was set at <0.05 to determine the significance of the findings and to estimate the precision of other parameters.
CT signs derived from the regression analysis were grouped into two categories to reflect findings. These categories were “highly suggestive” and “equivocal” for acute appendicitis. Z test was then performed to determine the relative frequency of the categories in the two groups of patients.
RESULTS
In this study, we reviewed 5681 cases (2146 men, 3715 women) with a mean age of 32 years (age range: 6 months-97 years). Of these patients 969 (17%) were diagnosed with acute appendicitis based on their CT findings. The diagnosis of acute appendicitis was verified in 870/969 (89.8%) patients on pathological examination of the specimens obtained during surgery. Of the 969 patients identified as having acute appendicitis on CT, 99 (11%) patients proved to be false positive cases as they were found to be negative in the pathological test. Of these 99 cases, 73 cases showed features of a chronic disease on pathological tests and 26 cases showed no pathologic abnormality.
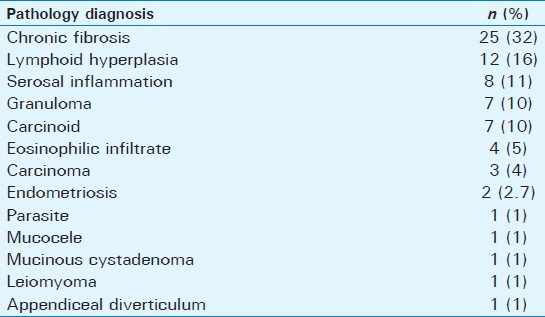
Pathological findings of patients in Group 2 (non-appendicitis cases) showed chronic fibrosis (33%), hyperplasia of lymphoid tissue (16%), focal serosal inflammation (11%), granulomatous disease (10%), carcinoid (11%), as well as signs of other neoplastic, infectious, and inflammatory processes [Table 1].
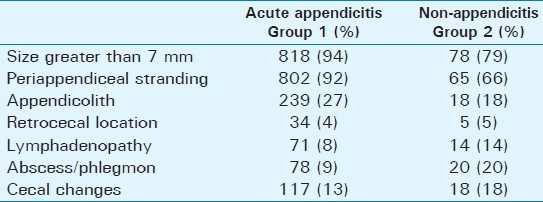
Most of the patients in the acute appendicitis Group 1 category exhibited appendiceal enlargement (94%) and peri-appendiceal infiltrative change (92%). Patients in the non-appendicitis Group 2 showed lower values (appendiceal enlargement 79% and peri-appendiceal infiltrative change 66%). Findings of an appendicolith were slightly more common in the acute appendicitis Group 1 (27%) versus 18% in the non-appendicitis Group 2. Lymphadenopathy in the right lower quadrant was present in 8% of Group 1 cases and 14% of Group 2 cases. Abscess or phlegmon was seen more often in the Group 2 category (20%) versus just 9% in Group 1 cases. Inflammatory changes within the cecum were observed in 13% of acute appendicitis Group 1 cases and 18% of Group 2 cases [Table 2].
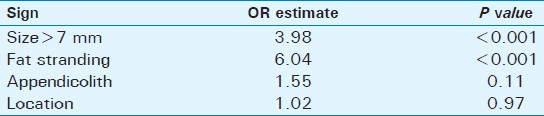
In our regression models, CT signs of appendiceal enlargement and mesenteric fat stranding were associated with acute appendicitis. Appendiceal enlargement greater than 7 mm was associated with an odds ratio (OR) of 3.98 for predicting acute appendicitis (P < 0.001). Infiltration of the peri-appendiceal mesenteric fat represented an OR of 6.04 (P < 0.001). The presence of appendicolith and a retrocecal location were not found to be statistically significant [Table 3].
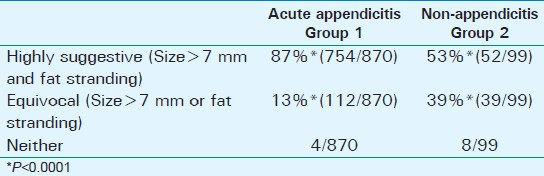
CT findings from the regression analysis for Group 1 and Group 2 were then compared. The presence of the pair of signs (appendiceal enlargement and mesenteric fat stranding) together was categorized as “highly suggestive” of acute appendicitis, while the presence of one of these signs in isolation was categorized as “equivocal”. Signs of appendiceal enlargement and mesenteric fat stranding were identified together on CT in 87% (754/870) of pathology-confirmed acute appendicitis cases compared with 53% (52/99) of cases with alternative diagnoses. Signs of enlargement or fat stranding was present as a single feature in 13% (112/870) of acute appendicitis cases compared with 39% (39/99) of cases in Group 2. The difference between these proportions was statistically significant (P < 0.0001) [Table 4].
DISCUSSION
Acute appendicitis is an extremely common clinical entity and accounts for 28% of patients presenting with acute abdomen.[10] The incidence of appendicitis is 8.6% for males and 6.7% for females.[11] Pre-operative imaging with CT for appendicitis has become standard of care, as one study found an increase from 1% of patients undergoing appendectomy to 97.5% over a 17-year period.[4] CT, using various techniques, has been found to be effective in the diagnosis of acute appendicitis: sensitivity (91-99%), specificity (91-99%), positive predictive value (92-98%), negative predictive value (95-100%), and accuracy (94%98%).[12–15] In this retrospective study, the positive predictive value was found to be 89.8%, slightly lower than the previous estimates.
Other much rarer conditions also affect the appendix, and some present acute symptoms that mimic the suppurative disease for which appendectomy is ordinarily performed.[6–816] In this study, conditions ranged from chronic and sub-acute inflammatory processes to benign proliferative diseases [Figure 1], malignant neoplasms [Figure 2], or infiltrative diseases [Figure 3]. Overall, 74/969 (7.6%) of patients presenting to the emergency department (ED) with findings of acute appendicitis on CT who underwent appendectomy over an 8-year period were found to have other primary disease of the appendix.
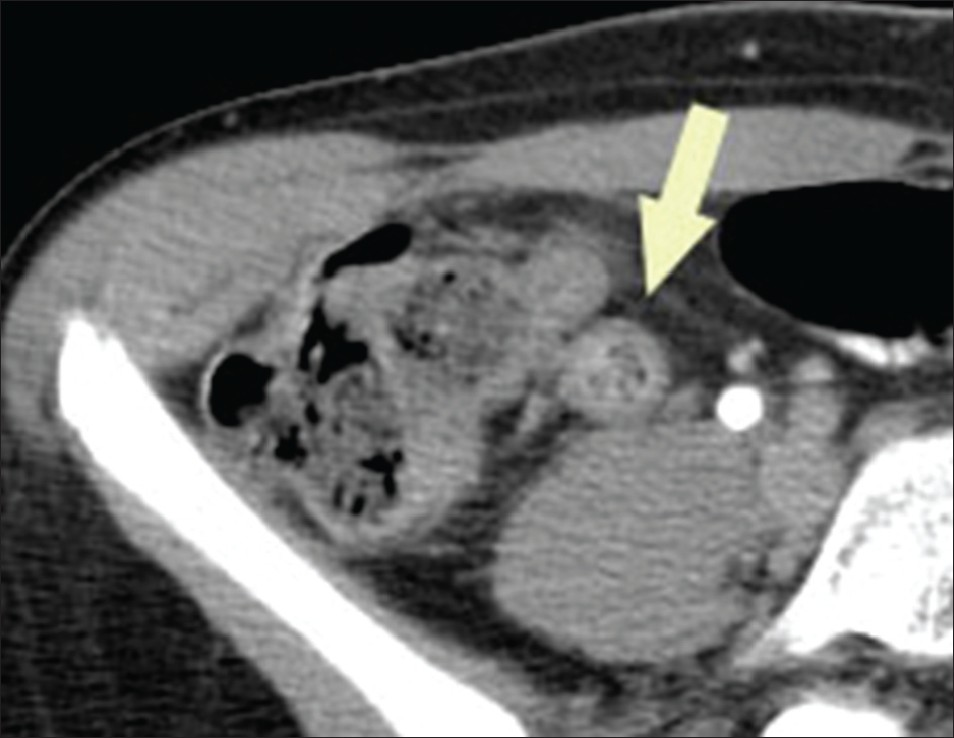
- Mucocele of the appendix. Axial computed tomography image through the pelvis shows an enlarged tubular structure in the right lower quadrant without significant adjacent inflammatory change (arrow). Note the bubbly appearance of the luminal contents.
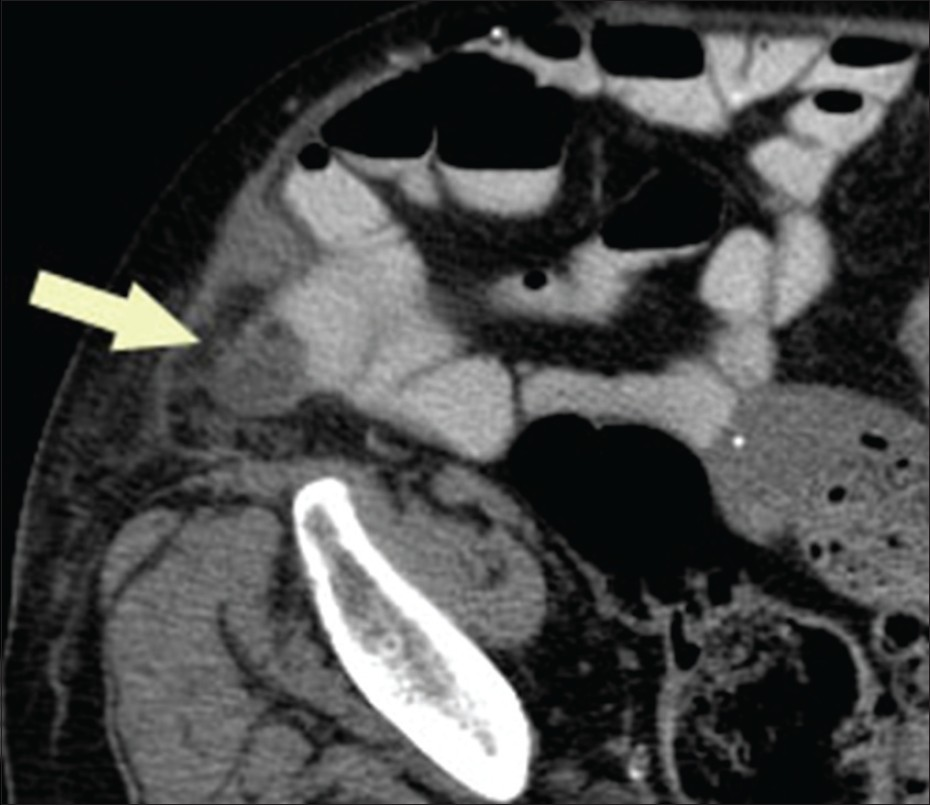
- Carcinoma of the appendix. Axial computed tomography image through the right lower quadrant demonstrates a homogenously thickened appendix with minimal surrounding fat stranding (arrow) exerting mass effect upon adjacent contrast-filled small bowel.
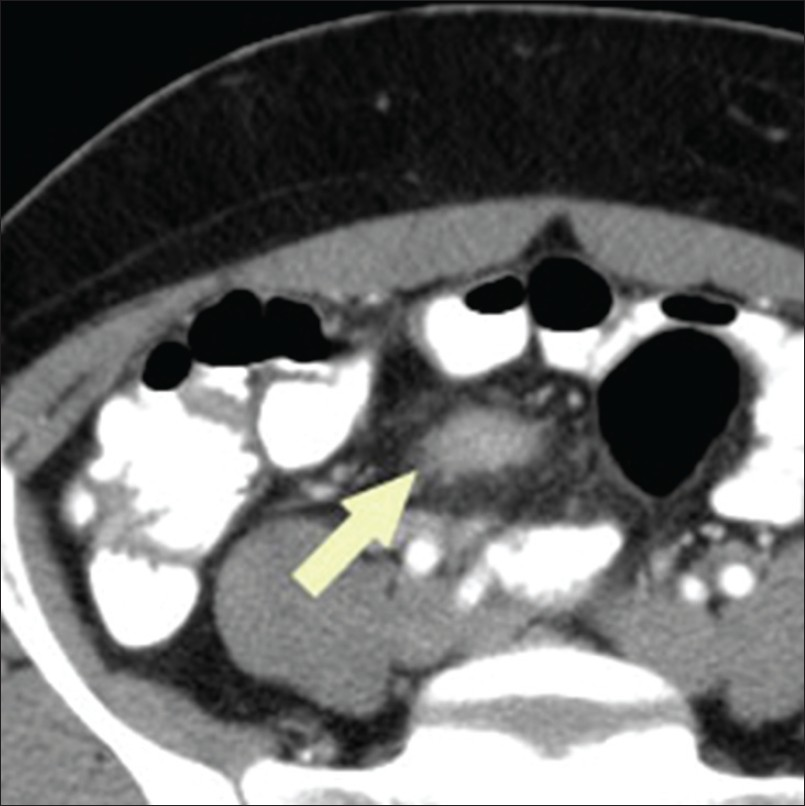
- Endometriosis involving the appendix. Axial computed tomography image through the upper pelvis shows a thickened appendix with hazy borders (arrow) and surrounding mild infiltrative changes in the mesenteric fat.
The sequence of pathophysiologic events in acute appendicitis is well known and each stage in the process correlates with findings on CT. Initially, the appendiceal lumen may become obstructed by inspissated fecal material or an appendicolith, classically described as a plain film finding. The clinical use of this finding is questionable, and in our study, it was a weak, non-significant predictor for acute appendicitis. In the past, appendicolith was found to have 100% specificity in some studies.[16]
Physiological secretion of mucus into the lumen may accumulate, distending the lumen and enlarging the appendix, a sign, which on its own, has been found to have sensitivity and specificity as high as 93% and 100%, respectively.[17] The use of appendiceal size on CT has been approached in several ways. Although one study concluded that 10 mm is the upper limit of normal, with a mean of 6.6 mm, based on surgical-pathologic correlation,[18] others have advocated a diagnostic algorithm that optimizes sensitivity and specificity based on size.[1419] In this study, appendiceal enlargement over 7 mm was found to have an OR of 4 for acute appendicitis.
As the lumen expands with fluid, vascular compression and ischemia results, and it is thought that leaky vessels allow bacterial translocation, leading to subsequent inflammation around the appendix. The CT finding of fat stranding can be an important sign of acute appendicitis and may support the clinical diagnosis, when the appendix is not clearly visualized.[9] Stranding has been shown to have a sensitivity ranging from 87% to 100%, and as long as it is centered around the appendix, its specificity is between 74% and 80%.[1720] Our findings echo those of previous reports, as the presence of peri-appendiceal inflammation was a strong, highly significant predictor of acute appendicitis, with an OR near 6.
Perforation and abscess formation may complicate late acute appendicitis and is helpful as confirmatory evidence in the presence of other signs.[141720] In this study, an abscess was present on CT in 9% of patients with proven acute appendicitis in Group 1, but was seen in twice as many patients with alternative pathology in Group 2. In 32% of Group 2 cases the pathology diagnosis was chronic fibrosis, suggesting the possibility in these patients of delayed clinical presentation or prior conservative management of perforated appendicitis. However, the finding is nonspecific, as CT evidence of abscess was also found in two-third of the cases of appendiceal carcinoma and four of seven cases of granulomatous disease.
When acute appendicitis is encountered, several of the above signs are commonly seen at once, as one study found at least three signs in all of its 100 patients.[17] Much less clear is the significance of intermediate, so-called “equivocal” findings, in which as few as one isolated primary sign is present. Studies, which have examined this scenario, have found that half of cases with only appendiceal enlargement, and 30-50% of cases with isolated periappendiceal mesenteric infiltration, may represent acute disease.[9] The present study was designed to address the association of these isolated signs with other pathologic entities affecting the appendix.
We analyzed the frequency of the most highly predictive signs of appendicitis in the acute and alternative pathology categories, and found that isolated findings are significantly more common in chronic and sub-acute disease of the appendix than in acute appendicitis. Highly suggestive findings of inflammatory change and appendiceal enlargement were present together in 89% of acute cases compared with 53% in the other group. Previous reports describe a similar proportion of cases (93%) with this pair of signs in acute appendicitis.[9] In contrast, 39% of alternative cases exhibited equivocal findings compared with 13% in the acute appendicitis category. There have been reviews that have examined the CT findings of other appendiceal diseases.[7] Studies on small group of patients suggest that there is no difference between the findings of acute and chronic appendiceal disease cases.[68] However, there has been no attempt to study a large sample size to subject these claims to statistical analysis, until now.
Looking at how the pathophysiology of acute appendicitis relates to findings on CT provides a possible explanation for our results. Although these individual conditions range from idiopathic inflammation to chronic fibrosis, the diseases tend to result primarily in either appendiceal enlargement or inflammation. For instance, hyperplasia of lymphoid tissue and fibrosis may increase the amount of soft tissue comprising the appendix, increasing its diameter without necessarily causing inflammatory changes. Similarly, granulomatous diseases like Crohn's or idiopathic inflammation of the serosa may result in inflammatory changes visible on CT without appreciable enlargement.
However, any of these processes could produce both enlargement and inflammation as long as acute luminal obstruction occurs. Indeed, more than 50% of the non-acute appendicitis cases had findings that were highly suggestive of acute disease.
How can the results of this study apply to everyday practice? The focus of this study was to examine diseases which are radiologic mimics of acute appendicitis, many of which are rare. Indeed, only 1.3% of patients who presented to the ED during the 8 year review period who underwent CT for suspicion of acute appendicitis turned out to have such a mimic when pathology was reviewed. On the other hand because the CT diagnosis was incorrect 10.2% of the time in this study, these other diseases should be considered in the differential diagnosis when radiologic signs are equivocal.
Given that it has been traditional surgical practice to have a low clinical threshold for surgical management, the prospect of further lowering the negative appendectomy rate should not be ignored. The ramifications of decreasing false positive diagnoses are not limited to the reduction of unnecessary surgery but also impact the judicious use of healthcare resources.[21] Appendiceal tumors can mimic acute appendicitis clinically and radiologically.[7] In cases of malignancy, surgical management is usually hemicolectomy rather than appendectomy.[16] Clearly, making an alternative diagnosis or simply indicating to the clinician that the findings are equivocal and may represent some other primary appendiceal disease may lead to conservative management or optimization of surgical approach.
This study is limited in a large part by its retrospective design, and the lack of follow-up in the nearly 4400 patients excluded for lack of findings suggesting acute appendicitis. Retrospective review neglects the clinical judgment employed by the interpreting radiologists in calling some appendices normal, as there is significant overlap of normal and abnormal parameters in borderline cases. These cases would probably further demonstrate findings we have targeted in this study and presumably would reveal more information about the CT appearance of such conditions.
To achieve statistical significance for such rare diseases, it was necessary to use a large sample size. Some of these conditions only occurred in one case out of several thousand patients visiting the emergency department. In our study design, these conditions were grouped together, not only to gather enough cases to allow a comparison with acute disease, but also to permit a clinical decision, that is, acute appendicitis versus other disease entities that may not require emergent surgery. Normal appendices encountered in the pathology results were included in the non-acute appendicitis group, rather than discarded, for this reason. Therefore, the results of this study should not be taken to describe the value of CT for any single disease because these diseases are so rare compared with acute appendicitis, especially in the acute presentation.
Unfortunately, the number of cases in this study, which is among the largest retrospective studies of acute appendicitis, made independent retrospective review of each examination impractical. Futhermore, over-reading examinations which were already acted upon in clinical real-time may have invalidated the results, as the decision to operate may have been contingent on the wording of any given report. The study is also limited by the CT technique used that was less advanced in technology and did not use the newer modified protocol regarding administration of oral and intravenous contrast. This difference in diagnostic quality may have affected the clinical decision made nearly a decade ago.
SUMMARY
In this large study, the positive predictive value of CT in defining acute appendicitis was found to be slightly lower than previously reported. While the diseases of the appendix other than acute appendicitis considered in the study are rare by themselves, as a group, they represent 7.6% of CT scans interpreted as positive for acute appendicitis. When individual CT findings were analyzed and compared between pathology-proven acute appendicitis patient group and other appendiceal disease patient group, a higher, statistically significant, proportion of these patients with alternative diseases showed a correlation with isolated signs. In summary, diseases of the appendix other than acute appendicitis manifest with different radiological pattern and should be considered as part of the differential diagnosis in borderline acute cases of appendicitis.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/73/104306
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Disconnect between incidence of nonperforated and perforated appendicitis: Implications for pathophysiology and Management. Ann Surg. 2007;245:886-92.
- [Google Scholar]
- Suspected acute appendicitis: nonenhanced helical CT in 300 consecutive patients. Radiology. 1999;213:341-6.
- [Google Scholar]
- Appendiceal CT in 140 cases: Diagnostic criteria for acute and necrotizing appendicitis. Clin Imaging. 1998;22:252-71.
- [Google Scholar]
- Negative appendectomy in the era of CT: An 18 year perspective. Radiology. 2010;256:460-5.
- [Google Scholar]
- Imaging for suspected appendicitis: Negative appendectomy and perforation rates. Radiology. 2002;225:131-6.
- [Google Scholar]
- The computed tomography appearance of recurrent and chronic appendicitis. Am J Emerg Med. 1998;16:26-33.
- [Google Scholar]
- Primary neoplasms of the appendix manifesting as acute appendicitis: CT findings with pathologic comparison. Radiology. 2002;224:775-81.
- [Google Scholar]
- Chronic inflammatory appendiceal conditions that mimic acute appendicitis on helical CT. AJR Am J Roentgenol. 2002;179:731-4.
- [Google Scholar]
- Incidence of acute appendicitis in patients with equivocal CT findings. AJR Am J Roentgenol. 2005;184:1813-20.
- [Google Scholar]
- Surgical validation of unenhanced helical computed tomography in acute appendicitis. Br J Surg. 2004;91:1641-5.
- [Google Scholar]
- The influence of age and gender on the utility of computed tomography to diagnose acute appendicitis. Am Surg. 2004;70:850-3.
- [Google Scholar]
- Accuracy of nonfocused helical CT for the diagnosis of acute appendicitis: A 5-year review. AJR Am J Roentgenol. 2002;178:1319-25.
- [Google Scholar]
- Why we miss the diagnosis of appendicitis on abdominal CT: Evaluation of imaging features of appendicitis incorrectly diagnosed on CT. AJR Am J Roentgenol. 2005;184:855-9.
- [Google Scholar]
- CT evaluation of appendicitis and its complications: Imaging techniques and key diagnostic findings. AJR Am J Roentgenol. 2005;185:406-17.
- [Google Scholar]
- Suspected acute appendicitis: Nonenhanced helical CT in 300 consecutive patients. Radiology. 1999;213:341-6.
- [Google Scholar]
- Appendiceal tumors: Retrospective clinicopathologic analysis of appendiceal tumors from 7,970 appendectomies. Dis Colon Rectum. 1998;41:75-80.
- [Google Scholar]
- Sensitivity and specificity of the individual CT signs of appendicitis: Experience with 200 helical appendiceal CT examinations. J Comput Assist Tomogr. 1997;21:686-92.
- [Google Scholar]
- Frequency of visualization and thickness of normal appendix at nonenhanced helical CT. Radiology. 2002;225:400-6.
- [Google Scholar]
- Independent predictors of acute appendicitis on CT with pathologic correlation. Acad Radiol. 2008;15:996-1003.
- [Google Scholar]
- The most useful findings for diagnosing acute appendicitis on contrast-enhanced helical CT. Acta Radiol. 2003;44:574-82.
- [Google Scholar]
- Effect of computed tomography of the appendix on treatment of patients and use of hospital resources. N Engl J Med. 1998;338:141-6.
- [Google Scholar]






