Translate this page into:
Computed Tomographic Features of Congenital Left Ventricular Diverticulum
Address for correspondence: Mr. Amit Nandan Dhar Dwivedi, Assistant Professor, Department of Radiodiagnosis and Imaging, Institute of Medical Sciences, BHU, Varanasi - 221005, Uttar Pradesh, India. E-mail: amitnandan21@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Congenital left ventricular diverticulum is a rare cardiac malformation characterized by a localized out-pouching from the cardiac chamber. They are most often found in the left ventricle (LV) but have been reported to occur in all chambers of the heart. The patient is usually asymptomatic. However, complications like embolism, infective endocarditis, arrhythmia and, rarely, rupture may be the initial presentation. Diagnosis can be established by echocardiography (EKG), computed tomographic (CT) angiography, and magnetic resonance imaging (MRI). We report a case of congenital left ventricular diverticulum in an adult with no valvular abnormality as an incidental finding in an uncommon location.
Keywords
Cantrell
cardiac
congenital
CT coronary angiography
ECG
left ventricular diverticulum
INTRODUCTION

Congenital left ventricular diverticulum (CLVD) is a rare cardiac abnormality consisting of a localized out-pouching from the free wall of the cardiac chamber. A weakness of the myocardial wall during the embryogenesis may cause a focal protrusion of the ventricular wall. They are most commonly diagnosed in early childhood because of their frequent association with other cardiac and midline thoraco-abdominal anomalies. CLVD is rare in adults and its incidence is reported to be about 0.4% in an autopsy series of adult patients with cardiac death.[1] Commonly, CLVD arises from the left ventricular apex; however, non-apical locations also occur.[2] We report a case of CLVD in an elderly patient as an incidental finding in an uncommon location with normal cardiac valves.
CASE REPORT
A 50-year-old male presented to our department with a history of dyspnea at rest without angina. The patient was a non-smoker, non-alcoholic, and non-hypertensive. There was no history suggestive of coronary artery disease or peripheral vascular disease. On 2D-echocardiography, it was reported that there was an out-pouching showing dyskinetic contractile motion arising from left ventricular lateral wall. No evidence of valvular abnormality was reported. Chest radiograph was unremarkable with no evidence of contour abnormality of cardiac silhouette.
On CT aorta angiogram, there was pooling of contrast into a thin-walled lobulated lesion arising from the anterolateral part of proximal portion of ascending aorta [Figure 1]. There was a superior and lateral displacement of left pulmonary artery. Left aortic sinus and left coronary artery [Figure 2] were inferiorly displaced. The origin and root of aorta were normal. Rest of the cardiac chambers and branch vessels were normal in course and caliber. A diagnosis of CLVD was offered. In addition, a large thrombus in the right atrium extending into the superior vena cava [Figure 3] was also observed. Patient was put on anticoagulation therapy with warfarin. No surgical treatment was proposed for the diverticulum. The patient on follow-up examination was found to be well.
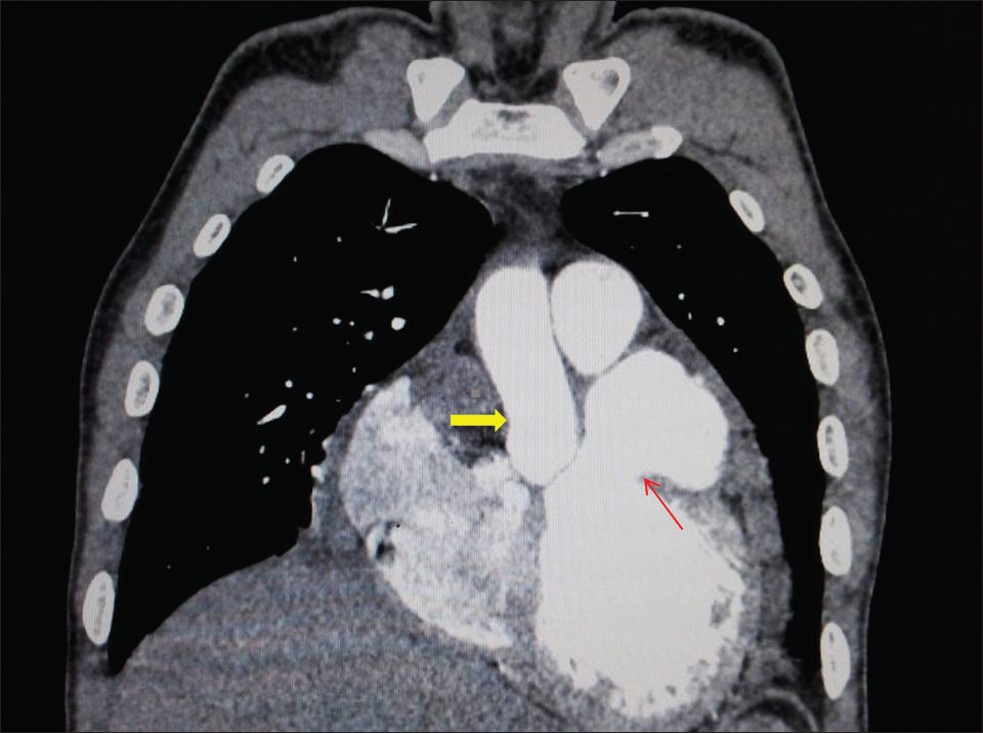
- Coronal image of CT aorta angiogram shows the pooling of contrast into a thin-walled protrusion arising from the anterolateral part of left ventricular wall (thin red arrow) abutting the proximal portion of ascending aorta (solid yellow arrow).
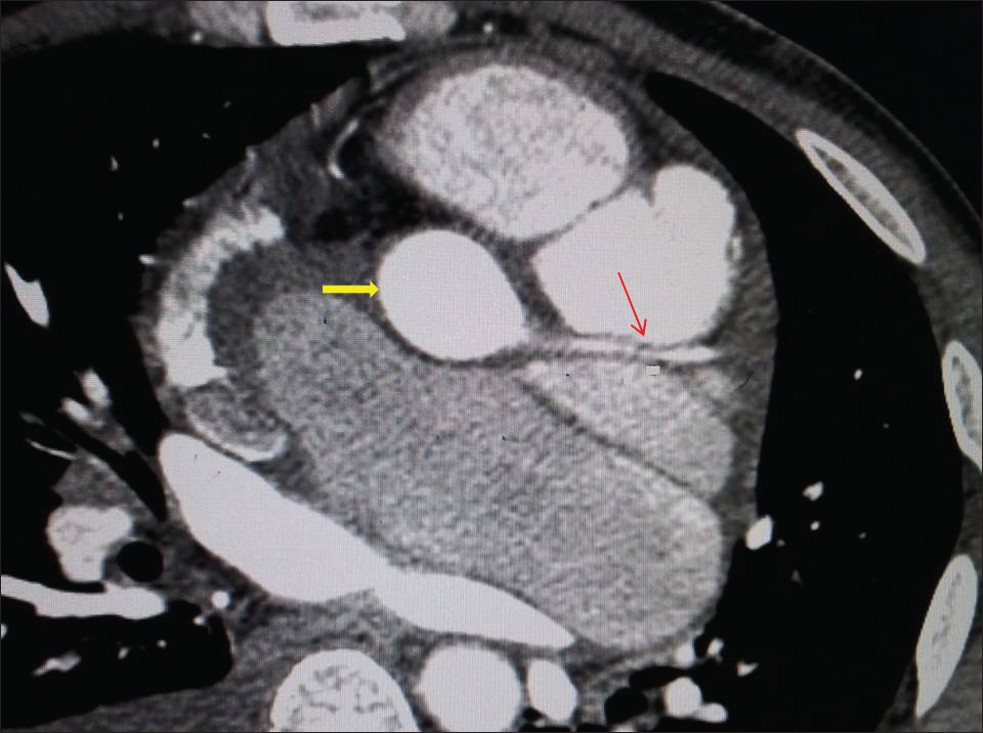
- Contrast-enhanced axial CT shows the displacement of left aortic sinus (bold yellow arrow) and left coronary artery (thin red arrow).
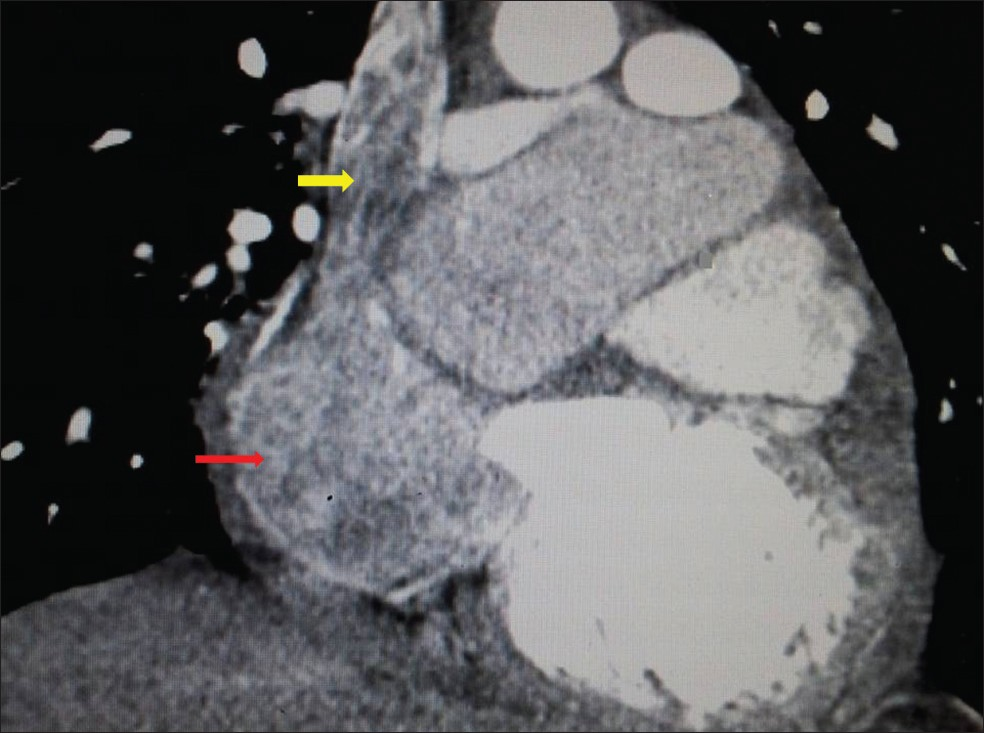
- Coronal-reformatted CT angiogram image demonstrates a large thrombus in the right atrium (bold red arrow) extending into the superior vena cava (bold yellow arrow).
DISCUSSION
A diverticulum is defined as a pouch or sac branching out from a hollow organ or structure. The first case of congenital left ventricular aneurysm was reported in 1838 and surgical resection of these malformations date back to 1912.[3] The incidence of congenital ventricular aneurysm/diverticula was previously reported to be as high as 0.4% in an autopsy series of patients who had died as a result of cardiac disease, but the incidence was only 0.26% in a population of patients referred for cardiac catheterization.[1] In a large retrospective echocardiographic study, researchers found a prevalence of only 0.04%.[4]
CLVD is most commonly diagnosed in early childhood because of their frequent association with other cardiac and midline thoraco-abdominal anomalies such as ventricular septal defect, tricuspid atresia, and tetralogy of fallot. Depending on the amount of myocardial fibers involved, diverticula may be primarily muscular or fibrous in nature. In children ventricular diverticulum has been commonly observed as the muscular type,[5] while the majority of ventricular diverticulum in adults has been classified as the fibrous type.[6] Table 1 compares the different features of the fibrous and muscular type of diverticula.
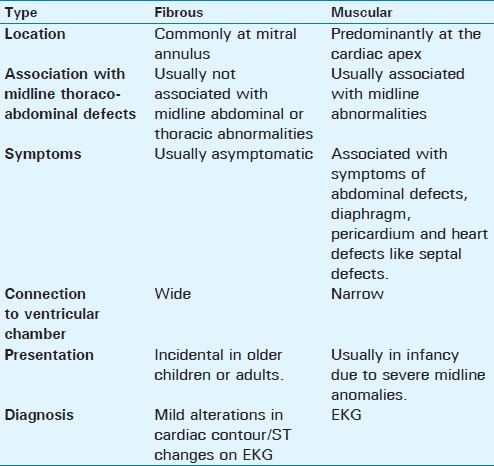
Fibrous ventricular diverticulum
Fibrous diverticulum consists mainly of fibrous tissues with few or no muscle fibers. Histologically, fibrous diverticula have connective tissues composed of reticulin fibers.
It is commonly located at the apex or base of left ventricle and its connection with the ventricular cavity is wide. Patient with fibrous diverticulum may be asymptomatic. It is usually diagnosed as an incidental finding in older children or adults by the mild alteration of cardiac silhouette or ST changes (ST segment on the electrocardiogram represents the period when the ventricles are depolarized) on EKG. The fibrous type is localized either in the apical or sub-valvular area and often leads to mitral and aortic regurgitation. The fibrous type is not accompanied by congenital midline thoracic or abdominal abnormalities and occurs more frequently in the Negroid race.
Muscular ventricular diverticulum
Muscular diverticulum is characterized by a muscular appendix emerging from the left ventricular apex. The diverticular musculature has a mechanical activity synchronous with the activity of the ventricles. Histologically, muscular diverticula contain all layers of the ventricular myocardium (with the myocardial architecture preserved) and minimal fibrous tissues. Its connection with the ventricular chamber is usually narrow. It is usually associated with symptoms of abdominal, diaphragm, pericardium, and heart defects like ventricular septal defects. Because of the association with midline defects muscular diverticulum is detected in infancy mostly by echocardiography. Muscular diverticula are most often localized at the apex part of the inferior or anterior walls of the left ventricle and frequently associated with thoraco-abdominal defects and also with Cantrell syndrome.
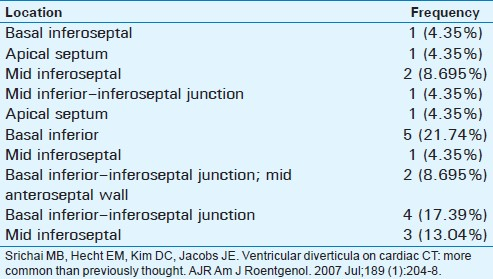
Table 2 summarizes the location of muscular ventricular diverticulum and its frequency of occurrence. The sizes of ventricular diverticula described in the literature range from as small as 0.5 cm in diameter to as large as 8–9 cm.[3]
Congenital ventricular diverticula are often asymptomatic and are usually found incidentally during diagnostic imaging procedures performed for other reasons.
Accompanying cardiac malformations can be evaluated on echocardiography. Doppler sonography can provide additional information about the contractility and myocardial perfusion of the diverticulum.
Congenital ventricular diverticula should be differentiated from other causes of acquired ventricular aneurysms such as those that occur after myocardial infarction, myocardial inflammatory disease such as sarcoidosis or myocarditis, infectious endocarditis or trauma.
Differentiating a ventricular aneurysm from a diverticulum is of importance in adult patients. A narrow mouth and synchronous contractility characterize a diverticulum. On the other hand, aneurysms show akinesia or paradoxic contractility of the out-pouching, which is asynchronous with the rest of the heart.[7]
Isolated ventricular non-compaction is another entity that needs to be considered in the differential diagnosis. Although ventricular non-compaction can appear similar to ventricular diverticula, diagnosis of ventricular non-compaction usually requires the presence of more than 3 deep inter-trabecular recesses.
CONCLUSION
The high spatial resolution and high temporal resolution offered by EKG-gated cardiac multi-detector computed tomographic angiography (MDCTA) provide a unique opportunity to evaluate the ventricular myocardium in a manner not previously afforded by non-gated CT or by alternative imaging techniques such as echocardiography. As the number of patients referred to cardiac MDCTA for evaluation of coronary artery disease increases, there is an opportunity to evaluate a population of patients who may have a higher incidence of ventricular diverticula in uncommon locations as in our case.
Source of Support: No financial disclosures
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/48/99182
REFERENCES
- Isolated congenital left ventricular diverticulum in an adult. A case report. Angiology. 1994;45:743-7.
- [Google Scholar]
- Case series: Congenital left ventricular diverticulum. Indian J Radiol Imaging. 2010;20:211-4.
- [Google Scholar]
- Congenital left ventricular aneurysms and diverticula: Definition, pathophysiology, clinical relevance and treatment. Cardiology. 2006;106:63-72.
- [Google Scholar]
- Congenital left ventricular aneurysms and diverticula: Clinical findings, diagnosis and course [in German] Schweiz Med Wochenschr. 1999;129:1249-56.
- [Google Scholar]
- Cantrell's syndrome.Left ventricular diverticulum in an adult patient. Circulation. 2000;101:109-10.
- [Google Scholar]
- Contrast harmonic power Doppler imaging of congenital ventricular diverticulum. A case report. Angiology. 2001;52:357-9.
- [Google Scholar]
- Cantrell's pentalogy: Report of four cases and their management. Pediatr Surg Int. 1997;12:428-31.
- [Google Scholar]






