Translate this page into:
Endovascular Management of Fusiform Superior Cerebellar Artery Aneurysms: A Series of Three Cases with Review of Literature
Address for correspondence: Dr. Anand Alurkar, Chief, Department of Neurointervetion, King Edward Memorial Hospital, Pune - 411011, Maharashtra, India. E-mail: anandalurkar@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Distal superior cerebellar artery (SCA) aneurysms are rare. Fusiform aneurysms of SCA are rarer and more challenging to treat. Parent artery occlusion by endovascular coiling is the treatment option for these cases. Presence of good collateral circulation and paucity of perforators from S1 and S2 segments makes this a feasible option. From 2007 to 2010, we treated three patients (two men and one woman between the ages of 42 to 64 years) with distal fusiform SCA aneurysms using endovascular coiling. All the patients presented with symptoms of rupture and were treated in the acute phase. Informed and written high-risk consent was given by all patients prior to the procedure. Successful angiographic and clinical outcome was achieved in all three patients. Endovascular treatment of fusiform SCA aneurysms with coils is a safe and feasible option in the management of this rare entity.
Keywords
Coiling
fusiform aneurysm
superior cerebellar artery
INTRODUCTION

Superior cerebellar aneurysms (SCA) are rare and account for 1.7% of all treated intracranial aneurysms. Distal SCA aneurysms (that exclude the basilar-SCA junction aneurysms) are even rarer and constitute less than 0.2% of all intracranial aneurysms. In the present report, we describe three cases of Fusiform SCA aneurysms treated successfully with endovascular coiling.
CASE REPORTS
Case 1
A 42-year-old man with no past significant medical illness presented with headache. CT scan done showed subarachnoid hemorrhage (SAH) predominantly in the perimesencephalic cisterns [Figure 1a]. Magnetic resonance imaging T1 gradient sequence also showed the hypointense signal suggestive of blood products in the perimesencephalic cisterns [Figure 1b]. Fetal posterior cerebral arteries are seen on both the sides arising from the internal carotid artery [Figures 1c and d]. DSA (digital subtraction angiogram) done subsequently revealed fusiform bulbous dilation involving both the cisternal and cortical segments of the left SCA [Figure 1e]. Endovascular treatment in the form of parent artery occlusion was done under general anesthesia, with complete exclusion of the aneurysm from the circulation as seen on post-coiling angiogram [Figure 1f]. Standard heparin protocol was followed and activated clotting time greater than 250 s was maintained during the procedure. Six-French (6F) Envoy (cordis) guiding catheter was placed in the distal vertebral artery. A combination of echelon-10 microcatheter (ev3) and transcend 0.014 microwire (Stryker) were used to access the aneurysms. Multiple Axium (ev3) coils were used to occlude the aneurysm. There were no intra- and periprocedural complications and patient was discharged on the 5th day after operation. The post-operative course was uneventful. The patient's neurological examination after 1 month was completely normal. Control angiogram done after 1 year showed stable occlusion of the aneurysm with endovascular coil in place [Figure 1g].
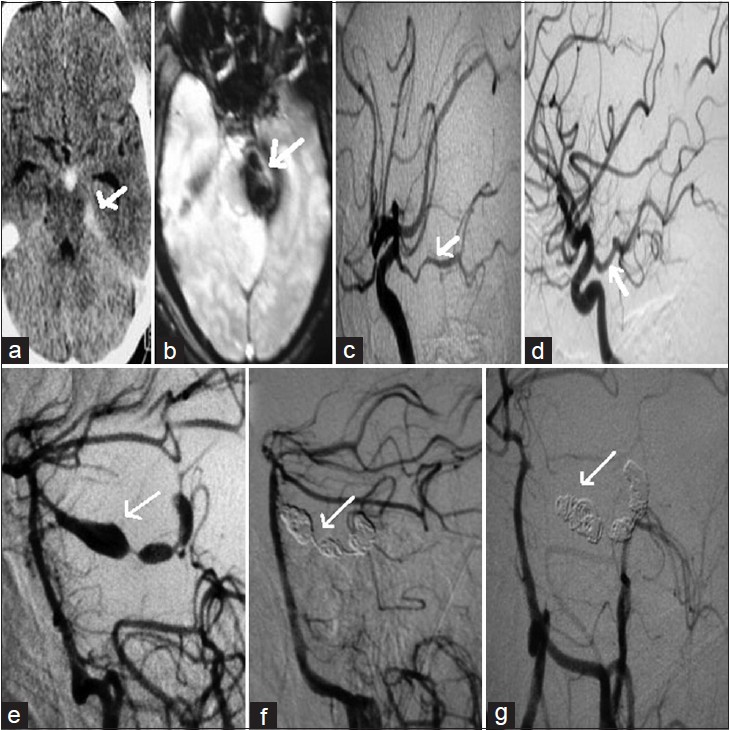
- (a) Computer tomography scan and (b) MRI gradient sequence shows subarachnoid hemorrhage (arrows) in the perimesencephalic cisterns (c, d) Right and left internal carotid artery (ICA) angiograms show the fetal posterior cerebral artery PCA (arrows) (e) Pre-procedure vertebral angiogram on lateral view shows the fusiform aneurysm (arrow) of left SCA (f) Post-procedure vertebral angiogram on lateral view shows aneurysm was occluded completely (arrow) with endovascular coil embolization. (g) Control angiogram shows stable occlusion (arrow) of the aneurysm.
Case 2
A 50-year-old lady, who had a history of hypertension, presented with severe headache and ataxia. CT scan done at admission showed acute right cerebellar hematoma [Figure 2a]. DSA done subsequently revealed fusiform aneurysm of the cisternal segment of the SCA [Figure 2b]. Endovascular treatment was done under general anesthesia with inside out coiling of the aneurysm with platinum coils [Figure 2c]. Standard heparin protocol was followed and an activated clotting time greater than 250 s was maintained during the procedure. 5F Envoy (cordis) guiding catheter was placed in the distal vertebral artery. A combination of echelon-10 micro-catheter (ev3) and transcend 0.014 micro-wire (Stryker) were used to access the aneurysms and multiple axiom (ev3) coils were used to occlude the aneurysm. Post-coiling angiogram showed complete exclusion of the aneurysm from the circulation. The post-operative period was uneventful. The patient's neurological examination done after 1 month was completely normal. Control angiogram done at the end of 1 year showed stable occlusion with no re-canalization of the aneurysm [Figure 1d].
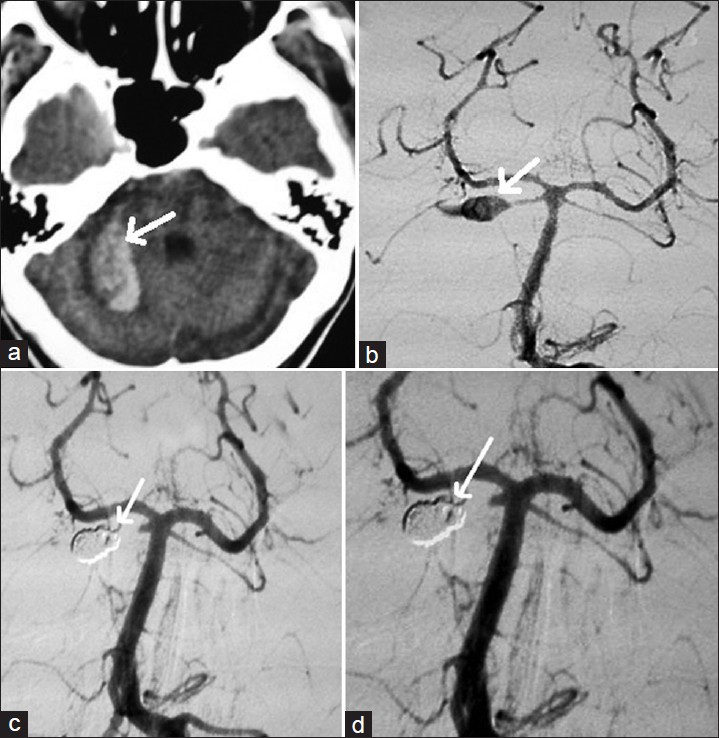
- (a) Computer tomography scan shows the right cerebellar hemorrhage (arrow) and (b) digital subtraction angiogram (DSA) shows the fusiform aneurysm (arrow) of the right superior cerebellar artery (SCA). (c) Postprocedure angiogram reveals complete exclusion (arrow) of the aneurysm and (d) control angiogram shows stable occlusion (arrow) of the aneurysm.
Case 3
A 64-year-old man, who had a history of hypertension, presented with headache and vomiting. CT scan showed SAH in the superior cerebellar cisterns [Figure 3a]. DSA done revealed a fusiform aneurysm of the distal SCA, predominantly involving the branch of the cortical segment [Figures 3b and c]. Standard heparin protocol was followed and an activated clotting time greater than 250 s was maintained during the procedure. 5F Envoy (cordis) guiding catheter was inserted in the distal vertebral artery. The aneurysm was accessed with a combination of micro-catheter (echelon-10) and micro-wire (traxcess12). Meticulous pre-shaping of the micro-catheter according to the shape of the target aneurysm aided in proper positioning of the micro-catheter in the aneurysm which was subsequently packed densely with the platinum micro-coils. Post-procedure angiogram showed complete exclusion of the aneurysm along with the branch of the cortical segment and preservation of the flow in the superior cerebellar artery (SCA) [Figure 3d]. There were no untoward events in the post-procedure hospital stay and patient was discharged after 1 week. No neurological deficit was seen during the clinical follow-up after 1 month. Control angiogram carried out after 1 year showed stable occlusion of the aneurysm with preservation of the ante-grade flow in the SCA [Figure 3e].
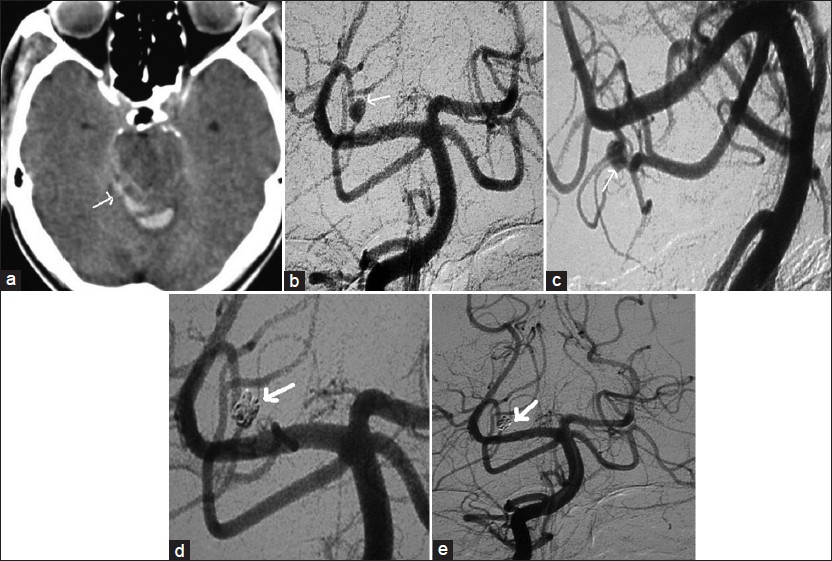
- (a) Computer tomography scan shows acute subarachnoid hemorrhage in the superior cerebellar cisterns. (b, c) Digital subtraction angiograms (DSA) show the aneurysm from the distal superior cerebella artery (SCA) (d) DSA shows the aneurysm completely occluded with coils. (e) Control angiogram demonstrates stable occlusion of the aneurysm.
DISCUSSION
Superior cerebellar arteries (SCA) are rare and account for 1.7% of all the intracranial aneurysms.[1] Distal SCA aneurysms represent only 0.2% of all the intracranial aneurysms.[23] Fusiform aneurysms are even rarer and only ten cases are reported in the literature.[4] In our present series, we report three cases of fusiform SCA aneurysms treated successfully by endovascular coiling technique. Presence of SAH predominantly in the perimesencephalic and superior cerebellar cisterns should raise a suspicion of the probability of SCA aneurysm and careful angiographic evaluation is needed for the diagnosis of these aneurysms. Two of our patients (Case 1 and Case 3) presented with perimesencephalic and superior cerebellar cisterns SAH, whereas 1 patient (Case 2) presented with right cerebellar bleed.
Aneurysms arising from the basilar–SCA junction were reported as SCA aneurysms,[1] which were not uncommon. These are latero-basillar aneurysms are not strictly aneurysms of SCA.[5] The fusiform aneuryms described in our series are true SCA aneurysms involving the cisternal and cortical segments of the SCA. Limited reports are available about the history of these aneurysms because of their rarity. Usually 90% of these aneurysms in this location present with subarachnoid hemorrhage (SAH).[6] Exact incidence of re-bleeding of these aneuryms is not known, but re-bleeding has been reported in the literature.[5] Re-bleeding necessitate the treatment of these aneurysms in the acute phase. These aneurysms can also present with ischemic symptoms as reported by Danet et al.[7]
All the three patients in our series presented with SAH and were treated in the acute phase to prevent the occurrence of untoward effects like re-bleed, vasospasm, and convulsions that may occur if there is delay in the treatment of these aneurysms.
Surgical treatment of these aneurysms is associated with good results, but requires an invasive route such as craniotomy via the pterional or inhemispheric approach for clipping of the aneurysm. Surgical options described for the treatment of these fusiform aneurysms include parent artery occlusion, trapping or body clipping, and wrapping.[8] Care must be taken to prevent injury to the third and fourth cranial nerves during surgery owing to the proximity of these nerves to the SCA. Occlusion of the SCA (either surgical or endovascular) is well tolerated because of the presence of the good collaterals between the SCA and both anterior inferior cerebellar artery and posterior inferior cerebellar artery through vermian arcade and also with the paramendian branches and perforators of the basilar artery.
Being minimally invasive, endovascular transarterial embolization with coils is a good therapeutic option for the treatment of these aneurysms. Cognard et al.,[9] described intra-aneurysmal injection of glue via the flow guiding catheter for the occlusion of the distal cerebellar aneurysms. In all our three cases we were able to successfully negotiate the pre-shaped microcatheter to the target site of the aneurysm and completely occlude the aneurysm with platinum coils, achieving complete exclusion of the aneurysm from the circulation.
Gotoh et al., in 2004 reported two cases of fusiform SCA aneurysms treated successfully by endovascular parent artery occlusion.[10] Our present report also describes the successful outcome in three patients with fusiform SCA aneurysms treated with the endovascular coiling method.
CONCLUSION
Fusiform SCA aneurysms are rare and usually present with SAH. Early intervention of this entity is required to prevent further complications. The treatment strategy should be based on the decision of a multidisciplinary team of neurosurgeon, neurophysician, and neuroradiologist. Endovascular treatment of these aneurysms is a feasible option that has acceptable risks when performed by experienced surgeons. A larger study has to be undertaken to prove the safety and efficacy of the treatment procedure and its long term implications.
Source(s) of Support: Nil
Conflict of Interest (If present, give more details): None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/47/99181
REFERENCES
- Superior cerebellar artery aneurysms: Incidence, clinical presentation and midterm outcome of endovascular treatment. Neuroradiology. 2007;49:747-51.
- [Google Scholar]
- Aneurysm arising from the medial branch of the superior cerebellar artery. Neurosurgery. 1986;18:350-2.
- [Google Scholar]
- CT localization of posterior fossa bleeding sites in subarachnoid hemorrhage. Surg Neurol. 1981;16:211-7.
- [Google Scholar]
- Fusiform aneurysm of the superior cerebellar artery: Short review article. Acta Neurochir (Wien). 2007;149:291-4.
- [Google Scholar]
- Endovascular therapeutic approach to peripheral aneurysms of the superior cerebellar artery. AJNR Am J Neuroradiol. 1996;17:1338-42.
- [Google Scholar]
- Aneurysm arising from the medial branch of the superior cerebellar artery. Acta Neurochir (Wien). 1996;138:1013-4.
- [Google Scholar]
- Distal superior cerebellar artery aneurysm presenting with cerebellar infarction: Report of two cases. AJNR Am J Neuroradiol. 2001;22:717-20.
- [Google Scholar]
- Postpartum dissecting aneurysm of the superior cerebellar artery case report. Neurol Med Chir (Tokyo). 1999;39:852-7.
- [Google Scholar]
- Treatment of distal aneurysms of the cerebellar arteries by intraaneurysmal injection of glue. AJNR Am J Neuroradiol. 1999;20:780-4.
- [Google Scholar]
- Dissection of the superior cerebellar artery: A report of two casesand review of the literature. J Clin Neurosci. 2004;11:196-9.
- [Google Scholar]






