Translate this page into:
Fahr's Disease Presenting with Aneurysmal Subarachnoid Hemorrhage
Address for correspondence: Dr. Hosam Al-Jehani, c/o Luisa Birri, 3801 University St., Suite 109, Montreal, QC, H3A 2B4, Canada. E-mail: hosam.aljehani@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Fahr's disease is a rare disorder of slowly progressive cognitive, psychiatric, and motor decline associated with idiopathic basal ganglia calcification (IBGC) and widespread calcification in the brain and cerebellum. Acute presentation of IBGC is most often as a seizure disorder; however, we present a case of an acute IBCG presentation in which the cause of the deterioration was an aneurysmal subarachnoid hemorrhage.
Keywords
Fahr's disease
idiopathic basal ganglia calcification
intracranial aneurysm
subarachnoid hemorrhage
INTRODUCTION

Fahr's disease is a rare disorder that was first described by Karl Theodor Fahr in 1930.[1] It usually presents with either slow progressive cognitive decline, psychiatric disturbance, or movement disorders. The radiological study shows it is bilateral with extensive calcification in the subcortical structures.[1]
Recent evidence links Fahr's disease to epilepsy as its acute presentation.[2] However, the etiology and pathophysiology of such association has yet to be elucidated. Another mode of acute presentation may be syncope.
We describe a patient with an acute deterioration in the level of consciousness and a CT scan demonstrating both subarachnoid blood and idiopathic basal ganglia calcification (IBGC). Further investigations showed a right posterior communicating artery aneurysm to be the source of the hemorrhage. We postulate that the extensive calcification in Fahr's disease negatively affects both brain parenchyma and intracranial vessels predisposing these individuals to such an acute presentation.
CASE REPORT
A 54-year-old housewife without any significant previous medical history, or any neurological problem presented with a transient loss of consciousness followed by headache and confusion. She had no history of movement or cognitive disorder prior to this event. No family history of subarachnoid hemorrhage or cognitive disability was obtained. On presentation her vital signs were stable and her blood pressure normal. She was drowsy and displayed signs of meningeal irritation. Her obtunded state was transient as she improved rapidly and soon became fully oriented. Her blood investigation, which included coagulation profile, blood cell count and serum electrolytes, was normal. Brain computerized tomography (CT) showed two major findings: first, diffuse bilateral subarachnoid hemorrhage involving the basal cisterns and both Sylvian fissures; and second, extensive calcification involving the basal ganglia, thalamus, corona radiata, and deep cerebellar nuclei [Figure 1].
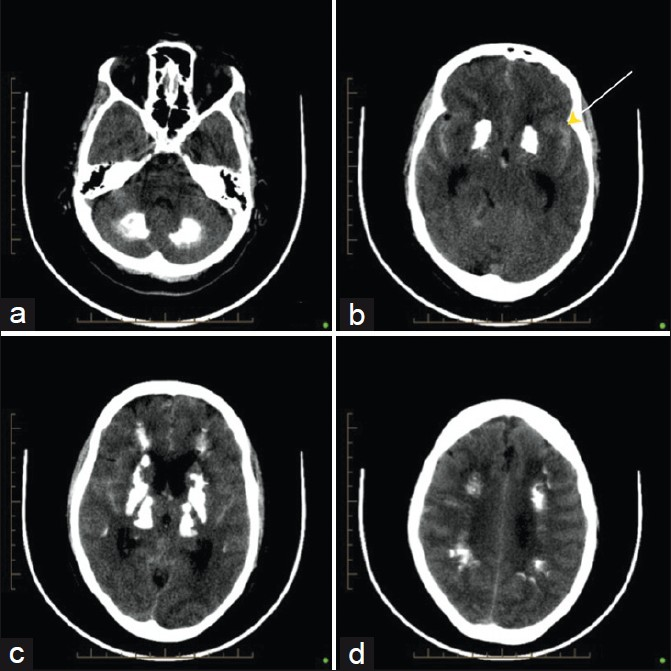
- Axial noncontrast CT scan of the brain shows extensive symmetrical calcification at the level of the (a) cerebellum, (b) basal ganglia, (yellow arrow) (c) thalamus and (d) White matter.
Formal cerebral angiography revealed a right posterior communicating artery aneurysm as the probable source of the SAH. It measured 7.8 × 5.7 × 4.2 mm with a neck of 3.3 mm. An attempt at coiling this aneurysm failed because of a tortuous internal carotid artery precluding safe access to the aneurysm [Figure 2].
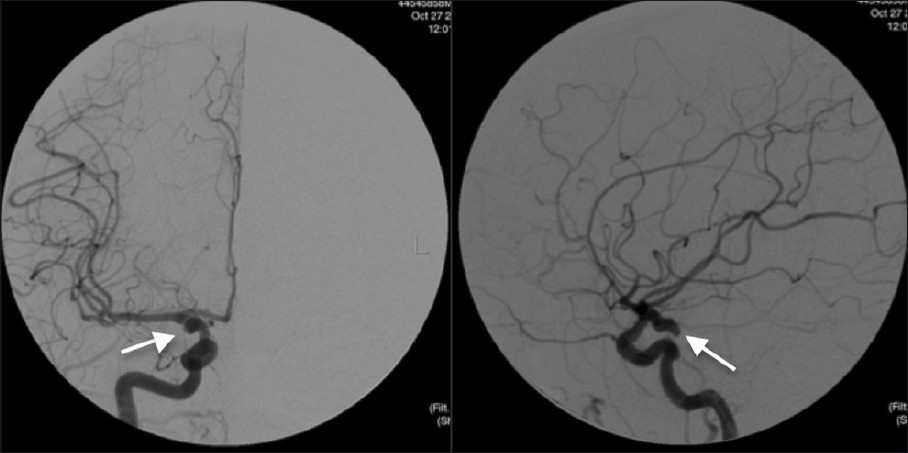
- Right internal carotid angiogram showing a multilobulated right posterior communicating artery aneurysm measuring 7.8 × 5.7 × 4.2 mm with the neck of the aneurysm measuring 3.3 mm (white arrow).
The patient was thereafter taken to the operating room where she underwent a right pterional craniotomy and clipping of the posterior communicating artery aneurysm. Her postoperative course was complicated by a right-sided upper extremity monoparesis due to a small middle cerebral artery territory ischemic infarct. However, over the following days she improved but experienced mild vasospasm that was treated medically with Euvolemia and Milrinone. She was also investigated for disorders that may cause abnormal calcium deposition which proved negative. Her serum calcium, phosphorus, and alkaline phosphatase were normal. The patient was eventually discharged from the hospital to a rehabilitation program where she showed significant improvement. The 6-month follow-up angiogram revealed no new aneurysms and no recanalization of the clipped aneurysm.
DISCUSSION
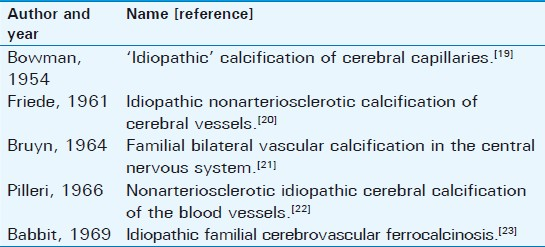
Fahr's disease, or idiopathic basal ganglia calcification is a rare syndrome that is characterized by abnormal intracranial calcification in the absence of any systemic calcium disorder. Different names have been given to abnormally excessive calcification within the brain parenchyma and cerebral vessels, reflecting the confusion regarding what causes this disorder [Table 1].[1]
Calcification has been described in the globus pallidus, caudate nucleus, putamen, thalamus, dentate nuclei, cerebellar lenticular nucleus, thalamus, the white matter of the cerebral cortex, as well as major intracranial vessels and those supplying the basal ganglia and the cerebellum.[3]
Affected individuals may remain asymptomatic. Typical presentation starts in the 4th to 5th decade of life with a slow cognitive decline, psychiatric abnormalities or movement disorders such as Parkinson's tremor, dystonia or cerebellar ataxia.[4]
Microscopic and biochemical analysis of brain deposits in Fahr's disease reveals that the stroma contains mainly calcium and protein without collagen or mucopolysaccharides. These deposits occur in vessel walls of arterioles, capillaries, veins, and in the perivascular spaces.[5] The calcium deposits are generally symmetrical and may be seen in the walls of small and medium sized vessels that could have resulted from inflammatory processes in the vessels.[6]
An acute deterioration in the level of consciousness may be the first symptom of Fahr's disease. A potential cause may be a complex-partial seizure as reported in a patient who had had a mild psychiatric disturbanceprior to a seizure episode.[7] In another case, Simone et al., described a 69- year-old patient who presented with recurrent episodes of deterioration in the level of consciousness and who was found to have classical radiological findings of Fahr's disease, in addition to pseudo-hypoparathyroidism, the correction of which improved his clinical status.[8]
Subarachnoid hemorrhage from a ruptured intracranial aneurysm has a poor prognosis with mortality rate of 50%, with 20% of survivors remaining severely disabled.[9] Histopathologically, aneurysms are associated with a loss of the media interna along with the elastic lamina as well as a thinning of the wall. There is also an associated intimal thickening in the parent artery. In larger aneurysms calcification may be seen either in the wall of the vessels or at the neck of the aneurysm.[10]
Earlier descriptions of Fahr's disease postulate a vascular pathophysiological process with calcification in both small and large vessels. Our case represents IBGC presenting with an SAH as a first presentation. Despite the heavy calcification seen on imaging she was asymptomatic before the event. We suggest that this could represent a subset of patients in whom there may be a predilection for intracerebral vessel symptomatology prior to the eventual onset of cognitive and psychiatric disturbances. The association of IBGC and an intracranial aneurysm has to date remained unreported in the literature. This case represents a first for Fahr's disease presenting with an aneurysmal subarachnoid bleeding.
CONCLUSIONS
Fahr's disease is a chronic slowly progressive neurodegenerative disorder that most commonly will present with acute deterioration in the level of consciousness, secondary to seizures. We report a case of Fahr's disease in which this acute deterioration was secondary to an aneurysmal subarachnoid hemorrhage.
This observation suggests that a brain CTA should be performed in patients with unexplained recurrent episodes of loss of consciousness, to rule out an aneurysm, even if they are known to have IBGC, so as to not attribute it to an epilepsy disorder.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/27/96542
REFERENCES
- What is and what is not ‘Fahr's disease’. Parkinsonism Relat Disord. 2005;11:73-80.
- [Google Scholar]
- Calcification of vessels in basal ganglia and cerebellum (hypoparathyroidism and Fahr syndrome), in Principles of neurology. New York: McGraw-Hill; 2001. p. :1032-3.
- [Google Scholar]
- Autosomal dominant dystonia-plus with cerebral calcifications. Neurology. 2006;67:620-5.
- [Google Scholar]
- Fahr disease: Signifi cance and predictive value of CT and MR fi ndings. Eur Radiol. 1992;2:570-5.
- [Google Scholar]
- The value of differential diagnosis of Fahr's disease by radiology. 2005. Internet J Radiol. 4:1. Available from: http://www.ispub.com/journal/the-internet-journal-of-radiology/volume-4-number-1/the-value-of-differential-diagnosis-of-fahr-s-disease-by-radiology.html
- [Google Scholar]
- Fahr's disease detected on a head CT scan in patient with “epileptic syncope” in the Emergency Department. Intern Emerg Med. 2010;5:263-5.
- [Google Scholar]
- An unusual case of transient loss of consciousness: The Fahr's syndrome. Recenti Prog Med. 2008;99:93-6.
- [Google Scholar]
- Case-fatality rates and functional outcome after subarachnoid hemorrhage: A systematic review. Stroke. 1997;28:660-4.
- [Google Scholar]






