Translate this page into:
Post-traumatic Cavernosal Artery Pseudoaneurysm Presenting as Right Hip Pain: An Imaging Evaluation
Address for correspondence: Dr. Aarthi Govindarajan, Department of Radiology and Imaging Sciences, Sri Ramachandra University, Porur, Chennai, Tamil Nadu, India aarthigovind@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Pseudoaneurysm of the cavernosal artery is quite rare. Herein, we describe color Doppler findings of post-traumatic pseudoaneurysm of the right cavernosal artery in a 19-year-old adolescent boy who presented with right hip pain. Doppler showed turbulence of flow with arterial inflow and outflow from the aneurysm. Selective transarterial catheterization of the internal iliac and internal pudental artery with microcatheter and embolization of pseudoaneurysm using histocryl resulted in alleviation of symptoms.
Keywords
Cavernosal artery
embolization
priapism
pseudoaneurysm
INTRODUCTION

Traumatic pseudoaneurysm of cavernosal artery is uncommon but a recognized condition as the patient presents with high flow priapism. Continuous priapism can lead to corporal fibrosis and erectile dysfunction.[1] High flow priapism can be treated by transarterial embolization, which results in proper cure while avoiding the complications of surgery.
CASE REPORT
A 19-year-old deaf and dumb boy sustained a blunt perineal trauma during a bicycle ride. Father gave the history of the trauma and mentioned the boy's refusal to ride a bicycle after the incident. The boy was brought to the orthopedic department 2 months after the trauma with complaints of right hip pain. Physical examination was essentially normal except for the partially erect penis.
Computed tomography and magnetic resonance imaging study of the pelvis was carried out. Plain CT scan and MRI of the pelvis were done to rule out right hip septic arthritis. The right hip joint was normal on plain CT scan. Contrast CT revealed blotches of contrast filling on the right side in the shaft of the penis [Figure 1a and 1b]
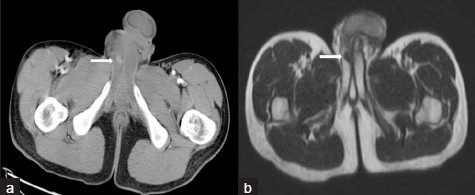
- Right cavernosal artery pseudoaneurysm in a 19-year-old boy with
right hip pain. (a) CT and (b) MRI images at the level of lower pelvis shows
blotches of contrast (white arrows) in shaft of the penis on the right side.
Penile Doppler was done and this revealed a homogenous cystic lesion measuring 2 × 1 cm in the right corpora cavernosa at the root of the penis. Color Doppler detected pseudoaneurysm originating from the right cavernosal artery [Figure 2a]. Multiple engorged venous sinusoids were seen adjacent to the pseudoaneurysm. Left cavernosal artery appeared normal. No engorged veins were seen on the left side.
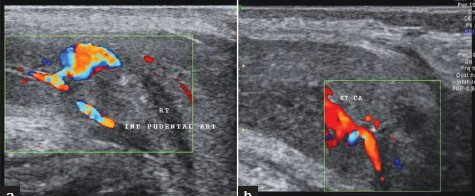
- Right cavernosal artery pseudoaneurysm. (a) Color doppler images
shows turbulence of flow in the pseudoaneurysm at the root of the penis.
(b) Postembolization color Doppler image shows complete absence of flow in
the pseudoaneurysm.
After informed consent, under general anesthesia bilateral femoral access was obtained by retrograde puncture and 5F and 6F sheath was introduced. Selective catheterization of right internal iliac and internal pudendal artery angiograms were performed, and showed a pseudoaneurysm filling through right cavernosal artery at root of the penis [Figure 3a]. The aneurysm was accessed using progreat microcatheter/wire and the aneurysm was occluded using histocryl embolization. Postembolization angiogram showed complete occlusion of the pseudoaneurysm [Figure 3b]. The patient tolerated the procedure well.
The patient was symptomatically better within 4-5 hours after the procedure. Priapism was resolved.

- (a) Right internal iliac artery angiogram shows internal pudental
artety (white arrow) with pseudoaneurysm filling through right cavernosal artery
(arrow head). (b) Postembolization microcatheter angiogram shows complete
obliteration of pseudoaneurysm.
Postembolization Doppler examination that was performed the next day showed normal-sized cavernosal arteries on both sides. No demonstrable flow was seen in the pseudoaneurysm on the right side [Figure 2b]. No engorged venous collaterals were seen.
DISCUSSION
Priapism is a state of prolonged erection of the penis that is not associated with sexual desire or stimulation. It can be of two types: high flow or low flow depending on the penile arterial blood flow.[2] The more common type, low flow priapism is due to diminished venous outflow from the cavernosa.
The high flow priapism is due to increased arterial inflow caused by trauma to the cavernosal artery in which the corporal artery is compressed against the pubic bone.[3] Few instances of idiopathic etiology are reported. This results in formation of arteriocavernosal fistula with or without a pseudoaneurysm. The erection can occur up to 8 hours after the traumatic event. Since arterial inflow is good, there is no ischemia. However untreated cases will proceed to permanent impotence. Selective transcatheter arterial embolization is the current treatment of choice in cases of high flow priapism.[4]
It is very important to differentiate between these two entities. Color Doppler scan and internal pudental angiography will confirm the findings. Color Doppler US is currently considered the imaging modality of choice for diagnosis of high flow priapism because it is sensitive, noninvasive, and widely available. It can assess the arterial inflow, venous leakage, and the spectral pattern of the cavernosal arteries.[5] High pulsatile flow with diastolic reversal, similar to findings seen in Papaverine-induced examination. The probable cause for this spectral pattern is secondary to the high pressure in the cavernous sinusoids.
Bilateral internal pudendal angiography is the gold standard in diagnosis of this condition but it is commonly accepted that color Doppler US is as sensitive as angiography for diagnosis of arterial priapism.[6]
Selective arterial embolization is the current therapy of choice in experienced hands. Microcoil embolization is associated with higher detumescence and lower postprocedure erectile dysfunction rates.[4] It can be performed by any of these embolizing materials: autologous blood clot, gel-foam, PVA, coils, and NBCA.[7]
NBCA is a permanent embolizing agent that quickly polymerizes when in contact with an ionic medium such as blood, resulting in immediate vascular occlusion. In our case, we used histocryl (glue) as the embolizing agent. However, sufficient experience, care, and caution are needed to use this agent as the embolization material.
Multiple choices of surgical procedures are available including proximal ligation of the internal pudendal artery, shunting procedures, penile exploration including incision, irrigation, and drainage of corporeal sinuses and percutaneous aspiration of the corpus cavernosum. Surgical procedures are associated with postoperative complications and subsequent erectile dysfunction.
After successful treatment with arterial embolization, postprocedural penile Doppler US evaluation is recommended to assess recanalization of the embolized cavernosal artery.[8] We performed postembolization Doppler the next day and it showed complete obliteration of pseudoaneurysm. The venous engorgement seen adjacent to the pseudoaneurysm was reduced.
CONCLUSION
Arterial priapism is uncommon, but significant sequel to penile or perineal trauma. Patients often do not present immediately as their erection is not painful. Active treatment is given once diagnosed.
Selective arterial embolization is a well-established technique for treating high flow priapism. It can reverse to normal prolonged priapism of several weeks.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/15/94232
REFERENCES
- Angiographic diagnosis of high-flow priapism with superselective transcatheter embolization and hematofibrinolytic therapy. Chin J Radiol. 2001;26:169-72.
- [Google Scholar]
- Post-traumatic arterial priapism: Colour Doppler examination and superselective arterial embolization. Clin Radiol. 1998;53:830-4.
- [Google Scholar]
- Changing diagnostic and therapeutic concepts in high-flow priapism. Int J Impot Res. 2005;17:109-13.
- [Google Scholar]
- Evolving concepts in the diagnosis and treatment of arterial high flow priapism. J Urol. 1996;155:541-8.
- [Google Scholar]
- Endovascular therapy for priapism secondary to perineal trauma. J Trauma. 2001;50:581-4.
- [Google Scholar]
- Arterial priapism: Diagnosis, treatment, and long-term followup. J Urol. 1994;151:1231-7.
- [Google Scholar]






