Translate this page into:
Deep Circumflex Iliac Artery Pseudoaneurysm as a Complication of Paracentesis
Address for correspondence: Dr. Bhawna Satija, B1/57, First Floor, Paschim Vihar, New Delhi - 110063, India satijabhawna@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We report a case of a pseudoaneurysm arising from the deep circumflex iliac artery, in an end-stage renal disease patient with gross ascitis, presenting with an anterior abdominal wall hematoma following paracentesis. Duplex Doppler sonography confirmed the presence of the pseudoaneurysm and multidetector computed tomography angiography delineated the detailed arterial anatomy.
Keywords
Duplex Doppler sonography
deep circumflex iliac artery
multidetector computed tomography angiography
pseudoaneurysm
INTRODUCTION

A pseudoaneurysm of the Deep circumflex iliac artery (DCIA) is a recognized complication of surgery, trauma, and paracentesis. The pseudoaneurysm can develop after any event that causes partial disruption of the vessel wall. The anatomical location of the deep circumflex iliac artery, especially its ascending branch, within the anterior abdominal wall, makes this artery vulnerable to injury during abdominal wall procedures. However, this is rare and only around 11 cases have been reported in the literature. Due to its rarity, the diagnosis may be missed and potential complications, including, persistent painful swelling, development of an abscess or rupture of a pseudoaneurysm may ensue in an untreated patient. This case report emphasizes the importance of considering the diagnosis of DCIA and performing the appropriate radiological imaging, to confirm its presence.
CASE REPORT
A 35-year-old female with gross ascitis developed a painful swelling in right iliac fossa, following a diagnostic paracentesis. The patient was a case of end-stage renal disease, diagnosed with mesangioproliferative glomerulonephtitis, and was on a regular, thrice-a-week hemodialysis regime. On examination, the swelling was tender and non-pulsatile. The patient′s vitals were stable and routine investigations were unremarkable except for mildly deranged renal function. The ultrasound examination (done on IE-33, Philips medical system, Netherlands) using a 7 - 11 MHz high-frequency linear array transducer, revealed a large, mixed echogenecity mass in the anterior abdominal wall of the right iliac fossa, with a sonolucent center [Figure 1]. A color Doppler study demonstrated a hypervascular nidus, with a swirling of red and blue colors with a feeding vessel arising from the deep circumflex iliac artery [Figure 2]. The Duplex Doppler of the neck of the feeding vessel demonstrated ‘to and fro’ sign suggestive of a pseudoaneurysm[Figure 3].
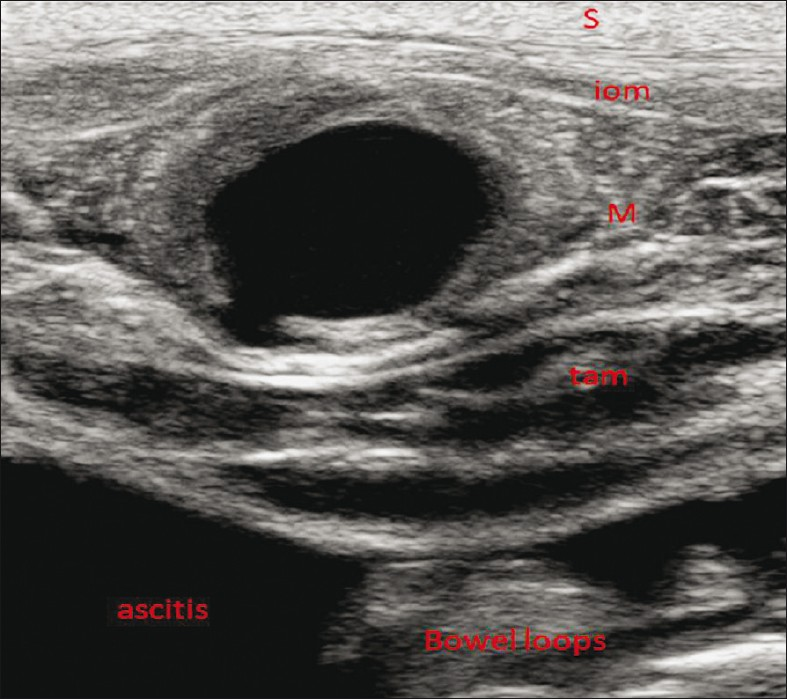
- A 35-year-old female with end-stage renal disease and ascitis with a palpable right iliac fossa mass following paracentesis. High-frequency transverse ultrasound image demonstrates a mass (m) between internal oblique muscle (iom) and transversus abdominis muscle (tam) with a central sonolucent center.

- Color flow Doppler demonstrates right iliac fossa pseudoaneurysm with Yin and Yang sign. Arrow points to the neck of the pseudoaneurysm.

- Spectral Doppler at the level of the neck of the pseudoaneurysm demonstrates “To and fro sign”.
The patient underwent computed tomography abdominal angiography, on a 64-slice multidetector row computed tomography scanner (Brilliance-64, Philips medical system, Netherlands) using the following parameters: 120 KVp, 335 mAs / rotation, rotation time 0.75 seconds, pitch 1.1, 64 – 0.625 mm collimation. Non-ionic iodinated contrast (Iopromide 370, Bayer, Germany) of 100 ml was administered intravenously followed by 20 ml normal saline, using a pressure injector (Mallinckrodt, Tyco healthcare, Cincinnati), by the bolus tracking technique, after a plain scan and the arterial and delayed phase acquisitions were obtained. The data were transferred to the workstation and a three-dimensional (3-D) volume was rendered (VR) and maximum intensity projection (MIP) reconstructions were made interactively.
The unenhanced images showed a hyperdense mass within the anterior abdominal wall of the right iliac fossa [Figure 4]. The arterial phase demonstrated a small nodular enhancement, approximately 4 mm in size, in the course of the ascending branch of the deep circumflex iliac artery, confirming the pseudoaneurysm [Figure 5]. There was no associated hemoperitoneum.
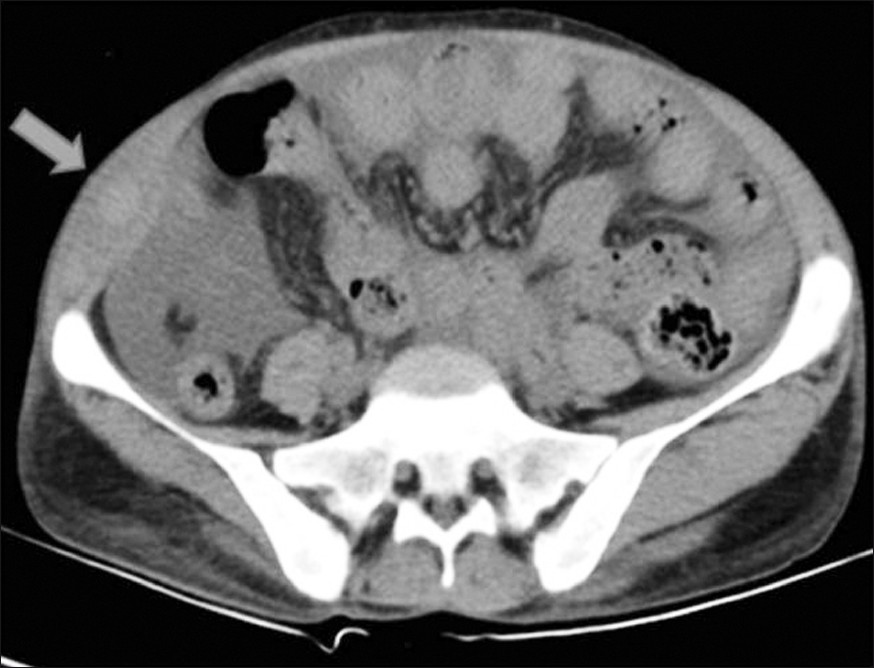
- Axial unenhanced CT scan of the abdomen demonstrates a hyperdense lesion in the right anterior abdominal wall (arrow).
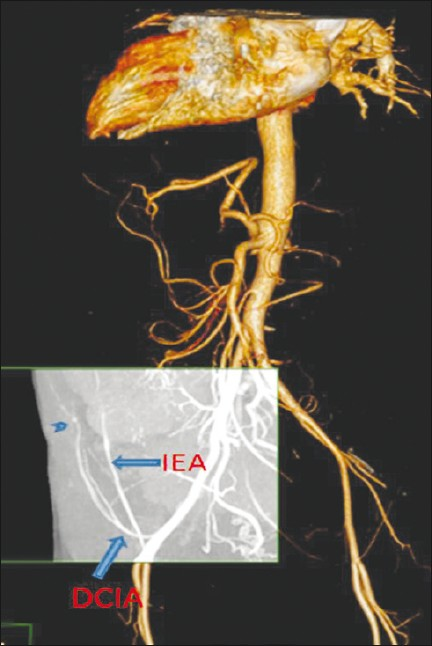
- Three-dimensional (3-D) computed tomography angiography image in arterial phase, volume rendered (VR) with maximum intensity projection (MIP) shows a small pseudoaneurysm arising from the distal part of the ascending branch of the right deep circumflex iliac artery (DCIA) (arrowhead). Inferior epigastric artery (IEA) is seen medial to it.
As the pseudoaneurysm was small in size and the patient was hemodynamically stable, no active intervention, either surgical or radiological, was considered. The patient was kept on conservative management with close monitoring. On a subsequent follow-up, there was significant reduction in the size of the pseudoaneurysm and the associated hematoma at one week, with complete resolution at about three weeks [Figure 6], as observed on the ultrasound / color Doppler studies.

- Follow-up ultrasound after three weeks. (a) High resolution gray scale and (b) color Doppler, images of right iliac fossa show normal DCIA (arrow) with complete resolution of the pseudoaneurysm and the associated hematoma.
DISCUSSION
The major trunk of the DCIA originates from the external iliac or femoral artery in the region of inguinal canal, just deep and superior to the inguinal ligament. Then it courses laterally and upward toward the medial aspect of the anterior superior iliac spine (ASIS). As it approaches the ASIS, it gives off a large ascending branch, which pierces the transversus abdominis muscle and lies between it and the internal oblique muscle. The artery then leaves the inguinal floor, pierces the transversalis fascia and enters a fibro-osseous tunnel formed by the line of attachment of the transversalis fascia and the iliacus fascia.[1]
The pseudoaneurysm of the DCIA is uncommon and a systematic review of literature revealed only around 11 such case reports. These occurred following liposuction,[2] surgical drain placement,[3] guidewire injury during femoral artery catheterization,[4] blunt abdominal wall trauma,[56] laparoscopic port placement,[7] anterior iliac bone graft harvesting,[1] and post renal allograft biopsy. [8] Among the causes mentioned earlier, no case has been reported following paracentesis.
It is difficult to diagnose a deep circumflex iliac artery pseudoaneurysm clinically, as the patient presents with a diffuse, tender mass, which is non-pulsatile and an audible bruit is usually absent. It is therefore difficult to differentiate it from a simple hematoma.
Paracentesis is a common procedure that is performed for diagnostic or therapeutic purposes. The preferred site for large-volume paracentesis is chosen in the dependent position, such as right or left lower quadrants. The site of puncture is chosen usually lateral to the rectus muscle to avoid the accidental puncture of the inferior epigastric artery. The inferior epigastric artery normally travels at the junction of the medial two thirds and lateral one third of the rectus or approximately 5 cm laterally from the midline. Injury to epigastric artery is one of the common complication of paracentesis.[9] DCIA travels far lateral to epigastric artery. Our case is unusual in that the patient presented with DCIA pseudoaneurysm which was more likely secondary to selecting a wrong site for paracentesis. This complication of injuring an artery can be usually avoided by initially perfoming a color Doppler ultrasound of the puncture site to make sure that there is no vessel in the path of the needle insertion.
Real time sonography provides a simple, reliable, and inexpensive assessment of such patients. The Color Doppler study with a duplex Doppler is the imaging modality of choice, allowing non-invasive evaluation of such masses and obviating the need for angiography. The hematoma exhibits variable echogenicity on the ultrasound, completely devoid of internal vascularity. In contrast, a pseudoaneurysm is easily demonstrated as an extravasation of blood flow outside the lumen. The typical Doppler findings include Yin and Yang sign in the body of the pseudoaneurysm and to and fro sign in the neck of the psuuedoaneurysm.[10]
If the diagnosis of pseudoaneurysm is in doubt, it can further be evaluated with computed tomography angiography. Multidetector row computed tomography (MDCT) angiography has many advantages. It is minimally invasive, with much better patient compliance, as compared to conventional angiography, so far considered the gold standard. It confirms the presence of a pseudoaneurysm and provides a detailed arterial anatomy. The exact site and size of the pseudoaneurysm is demonstrated. It also rules out the presence of any associated complications like hemoperitoneum.
The treatment of the pseudoaneurysm varies from conservative to open surgery, depending upon the size and the complications associated with it. Conservative management, with close monitoring, can be considered in patients who are hemodynamically stable. Spontaneous resolution of a pseudoaneurysm may occur as a result of spontaneous thrombosis.[11] The treatment options include simple ligation and excision, transcatheter embolization with gelfoam, coil or N-butyl-cyanoacrylate (NBCA), and ultrasound-guided thrombin injection or ultrasound-guided compression.[8]
In conclusion, it is very important to select an appropriate site for paracentesis and to use color Doppler guidance before performing paracentesis to avoid injury to epigastric artery or DCIA.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/10/94022
REFERENCES
- Pseudoaneurysm of the deep circumflex iliac artery:A rare complication at an anterior iliac bone graft donor site treated by coil embolization. Chang Gung Med J. 2002;25:480-4.
- [Google Scholar]
- Rupture of a deep circumflex iliac artery after abdominal liposuction: Treatment with selective arterial transcatheter embolization. Cardiovasc Intervent Radiol. 2009;32:1288-90.
- [Google Scholar]
- Deep circumflex iliac artery-related hemoperitoneum formation after surgical drain placement: Successful transcatheter embolization. Cardiovasc Intervent Radiol. 2010;33:402-5.
- [Google Scholar]
- Hematoma of the abdominal wall.A case report: Pitfall of Seldinger method via femoral artery. No Shinkei Geka. 2009;37:167-71.
- [Google Scholar]
- An unusual case of noncavitary hemorrhage revealed by intravenous contrast-enhanced computed tomography. J Emerg Med. 2002;22:21-5.
- [Google Scholar]
- Diagnosis and treatment of expanding haematoma of the lateral abdominal wall after blunt abdominal trauma. Eur Radiol. 1999;9:1553-5.
- [Google Scholar]
- Implications for port placement of deep circumflex iliac artery damage at laparoscopy. J Am Assoc Gynecol Laparosc. 1999;6:221-3.
- [Google Scholar]
- An unusual case of abdominal wall bleeding after renal allograft biopsy. Indian J Nephrol. 2012;21:62-5.
- [Google Scholar]
- The “to-and-fro” sign: Duplex Doppler evidence of femoral artery pseudoaneurysm. AJR Am J Roentgenol. 1988;150:632-4.
- [Google Scholar]
- Sontaneous resolution of posttraumatic middlemeningeal artery pseudoaneurysm. AJNR Am J Neuroradiol. 2006;27:882-3.
- [Google Scholar]






