Radiographically Occult Latent Radiogenic Osteosarcoma Uncovered on Tc-99m Methylene-diphosphonate Bone Scintigraphy
Address for correspondence: Dr. Prashant Jolepalem, William Beaumont Hospital, 3601 W. 13 Mile Road, Royal Oak, MI 48073, USA. E-mail: pjolepalem@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We present a case of a 70-year-old male who was referred for a technetium-99m methylene-diphosphonate bone scan for mild left hip pain and an elevated alkaline phosphatase level of 770 units/L. No additional information was provided and the patient's history was limited due to a language barrier. We were able to ascertain that the patient had a remote history of prostate cancer, which had been treated with radiation. Originally, we felt the bone scan was compatible with Paget's disease; however, further work-up revealed the presence of osteosarcoma, which was potentially radiation-induced.
Keywords
Bone scan
osteosarcoma
radiogenic malignancy
secondary malignancy
INTRODUCTION

Technetium-99m (Tc-99m) in complex with methylene-diphosphonate (MDP) is a commonly used substrate in radionuclide bone imaging. Bone scans utilizing this radiotracer are very sensitive and enable nuclear medicine physicians to screen for various osseous abnormalities and pathologies. Localization of the radiotracer is accomplished through the exchange of Tc-99m MDP for phosphate compounds during active bone remodeling, and aggregation is subsequently detected using a gamma camera.[1]
Even though the utilization of Tc-99m MDP bone scintigraphy is useful for identifying various physiologic abnormalities, its overall specificity is limited primarily by the lack of anatomic detail. It is therefore important to utilize the patient's medical history, in conjunction with other forms of imaging, to aid in differentiating potential pathologies. Here, we present a case in which Tc-99m MDP bone scintigraphy was utilized to raise concern for a serious abnormality despite relatively occult findings by conventional imaging modalities.
CASE REPORT
A 70-year-old male presented with mild left hip pain and was found to have an elevated serum alkaline phosphatase (ALK) level of 770 units/L. Unfortunately, due to a language barrier, a complete medical history could not be obtained. In light of the patient's elevated ALK level, the patient was referred for a whole-body Tc-99m MDP bone scan. The planar whole body images [Figure 1a] of the Tc-99m MDP bone scan demonstrated intense diffuse uptake extending from the left femoral head to the proximal shaft of the femur. Initially, we felt this type of appearance could be compatible with early Paget's disease given the markedly elevated ALK, despite the absence of apparent structural deformities.
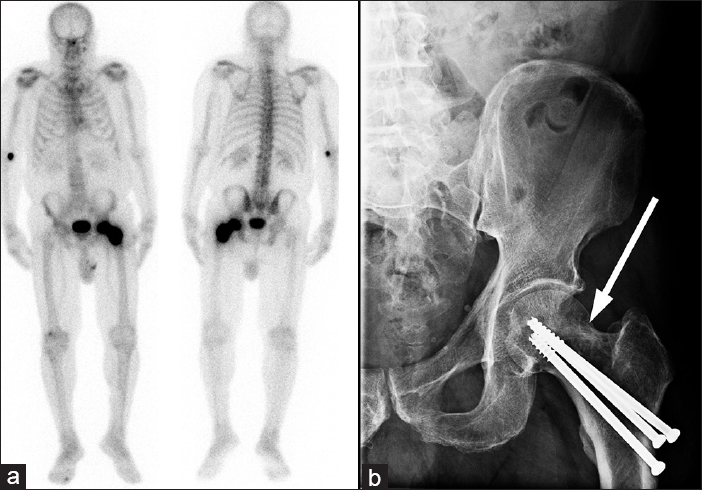
- 70-year-old male with mild left hip pain and elevated alkaline phosphatase diagnosed with radiogenic osteosarcoma. (a) The planar whole body images of the technetium-99m methylene diphosphonate bone scan demonstrates intense diffuse uptake extending from the left femoral head to the proximal shaft of the femur (double ended arrow). (b) The plain film of the left hip depicts three previously unreported fixation screws surrounded by osteopenic lesions (arrow) in the femoral neck and head.
To confirm the initial diagnosis, the patient was sent directly for an X-ray [Figure 1b]. However, the pattern of multifocal sclerosis (cotton wool appearance) that would be expected of Paget's disease was not present.[2] Instead, the radiograph demonstrated three previously unreported fixation screws, used to repair a femoral neck fracture (later discovered to have occurred 1 year ago). Surrounding the screws were poorly defined osteopenic, potentially lytic lesions in the femoral neck and femoral head [Figure 1b]. Correlation of the Tc-99m MDP bone scan with the X-ray changed the initial diagnosis from suspected Paget's disease to a differential of malignancy/metastasis, reparative phase of osteonecrosis, osteomyelitis, or reactive osteolysis to the fixation screws. Though simple loosening of the fixation screws could have explained the patient's mild hip pain, the activity demonstrated by the bone scan was much too diffuse and intense to support this diagnosis.[3]
To evaluate for metastatic disease, a computed tomography scan of the chest, abdomen, and pelvis was ordered the following day. Evaluation of the scan of the left hip was limited due to streak artifact from the screws; however, it was still possible to appreciate some mixed lytic/sclerotic changes in the native bone [Figure 2a and b]. Even though these changes raised the suspicion of osseous malignancy or metastasis, they were not pathognomonic, as hardware loosening, osteopenia, and degenerative changes could have a similar appearance.[4] However these findings in combination with the bone scan findings, provided enough suspicion of a pathology sinister enough to refer the patient for surgical hardware revision with potential biopsy.[56]
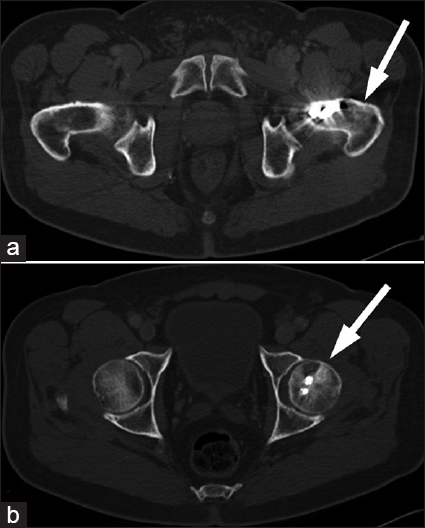
- 70-year-old male with mild left hip pain and elevated alkaline phosphatase diagnosed with radiogenic osteosarcoma. (a and b) Computed tomography of the pelvis reveal mixed lytic/sclerotic lesions (arrows) within the native bone, although evaluation of the left hip was limited due to streak artifact as seen on the two axial slices in Figure 1.
Surgical exploration of the left hip revealed a grossly abnormal appearance of the left proximal femur with areas of hemorrhagic bone surrounding lytic lesions. The fixation screws were removed and curettage of the suspicious lesion was performed. Histologic study of the biopsy [Figure 3] demonstrated sarcomatous, spindle shaped cells with adjacent tumor osteoid production; represented by eosinophilic, amorphous, fibrillary deposits between individual or small aggregates of tumor cells. These histological findings were diagnostic of osteosarcoma.[7]
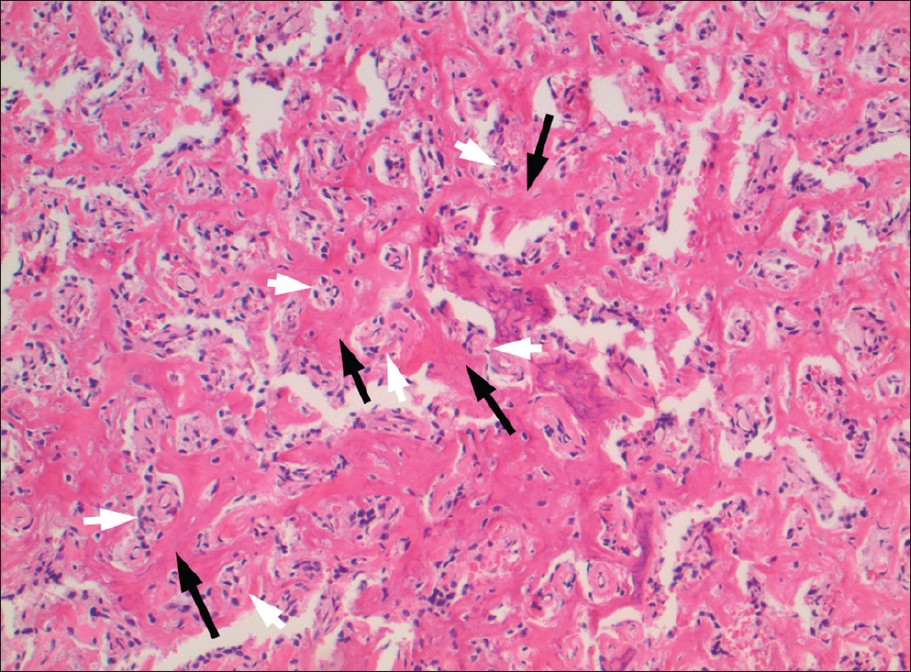
- 70-year-old male with mild left hip pain and elevated alkaline phosphatase diagnosed with radiogenic osteosarcoma. Histologic examination of the curettage (using Hematoxylin and Eosin stain, ×10) reveals sarcomatous, spindle shaped cells (white arrows) with adjacent tumor osteoid production (black arrows); represented by eosinophilic, amorphous, fibrillary deposits (white arrows) between individual or small aggregates of tumor cells (black arrows).
In context, the presence of osteosarcoma was highly unlikely as there have been no case reports of primary osteosarcomas occurring in a site of a fracture that was surgically repaired 1 year prior. Additionally, the distal femur would be a far more likely site for a primary osteogenic sarcoma to occur.[8] However, upon further interrogation of the patient's past medical history, it was discovered that the patient had prostate cancer 11 years ago. Given the standard of care at that time, one could surmise that he was treated with 60-70 Gy of targeted external beam radiation to the prostate.[9] The dose that he received and the time frame since receiving his radiation would be compatible with radiogenic osteosarcoma as there is a latency period of about 10 years.[10] The repaired stress fracture 1 year prior was potentially pathologic from the malignancy, but was most likely missed due to the slightly atypical radiographic appearance on the plain film X-ray performed in the surgeon's office.
DISCUSSION
Tc-99m MDP bone scans are very sensitive tests for detecting a wide array of abnormalities within the bone. Despite its comprehensive applicability, it is limited in identifying specific diseases and pathologies; often relying on the addition of other investigative modalities to reach a final diagnosis.[16] Here, a Tc-99m MDP bone scan was used to identify the presence of abnormal bone remodeling, which led to further imaging work-up and confirmatory biopsy.
Osteosarcomas are particularly sensitive to Tc-99m MDP bone scans as their pathology involves active bone remodeling. However, its presence here was unexpected due to the atypical location on the bone scan and the limited available medical history (due to a language barrier). When paired with the patient's medical history of radiation treatment and recent fracture, the diagnosis of radiogenic osteosarcoma became more likely. The femur would have been exposed to scatter and Bremsstrahlung radiation from its proximity to the treatment field. Additionally, the 10-year latency period to developing malignancy is typical for post-external beam radiation therapy induced malignancies.[10] The Tc-99m MDP bone scan demonstrated its value by raising the suspicion for a more sinister process in the left hip than was seen in radiographic appearance on plain film.
CONCLUSION
This case demonstrated the value of Tc-99m MDP bone scintigraphy as an initial detector of bone abnormalities. Its sensitivity prevents it from identifying specific pathologies without the aid other investigative methods as depicted in this case. This case also underscores the importance of considering the bone scan findings in conjunction with the patient's clinical history and anatomic imaging. By using all this information in combination, we were able to sift through the differential and refer the patient for appropriate management.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2013/3/1/46/120786
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- From the archives of the AFIP. Radiologic spectrum of Paget disease of bone and its complications with pathologic correlation. Radiographics. 2002;22:1191-216.
- [Google Scholar]
- Nuclear medicine and the infected joint replacement. Semin Nucl Med. 2009;39:66-78.
- [Google Scholar]
- Three-phase bone scintigraphy pattern of loosening in uncemented hip prostheses. Eur J Nucl Med. 1995;22:299-301.
- [Google Scholar]
- FDG-PET for detection of osseous metastases from malignant primary bone tumours: Comparison with bone scintigraphy. Eur J Nucl Med. 2000;27:1305-11.
- [Google Scholar]
- Differential Diagnosis in Surgical Pathology. (2nd ed). Philadelphia: Elsevier; 2009.
- [Google Scholar]
- Impact of concurrent androgen deprivation on fiducial marker migration in external-beam radiation therapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2012;84:e7-12.
- [Google Scholar]
- Second malignancies in prostate carcinoma patients after radiotherapy compared with surgery. Cancer. 2000;88:398-406.
- [Google Scholar]






