Translate this page into:
Renal Vein Leiomyoma: A Rare Entity with Review of Literature
Address for correspondence: Dr. Santosh Kumar, Department of Urology, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, Haryana and Punjab, India. E-mail: santoshsp1967jaimatadi@yahoo.co.in
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Tumors of vascular origin are unusual. These tumors are predominantly malignant and commonly arise from the inferior vena cava. Benign smooth muscle tumors arising from renal vein are very rare. We present a case of leiomyoma of renal vein in a post-menopausal woman that clinically resembled a retroperitoneal paraganglioma.
Keywords
Rare
renal vein leiomyoma
surgery
venous tumors
INTRODUCTION

Tumors of venous origin are rare. Most common tumors that arise from veins are smooth muscle tumors and these are usually malignant. Malignant venous tumors (leiomyosarcoma) arise commonly from the inferior vena cava.[123] Benign tumors arising from renal vein (leiomyoma) are very rare. Here, we report a case of renal vein leiomyoma in a post-menopausal woman, clinically mimicking a paraganglioma.
CASE REPORT
A 61-year-old hypertensive post-menopausal woman presented with a 2-year history of dull aching intermittent left hypochondrial pain that occasionally radiated to her back with paroxysmal attacks of palpitations and sweating. On abdominal examination, mild tenderness was felt in the left hypochondrium with no obvious palpable lump. Routine investigations like hemoglobin level 12.0 gm% (normal value >10 gm%), total leukocyte count 9600/mm3 (normal range 4000-11,000/mm3), serum sodium 142 mEq/l (normal range 135-150 mEq/l), serum potassium 4.1 mEq/l (normal value 3.5-5.0 mEq/l), serum creatinine 0.9 mg/dl (normal range 0.6-1.2 mg/dl), blood urea 22 mg/dl (normal range 15-40 mg/dl), total bilirubin 0.6 mg/dl (normal value up to 0.8 mg/dl), serum glutamic oxaloacetic transaminase (SGOT) 30 IU/l, and serum glutamic pyruvic transaminase (SGPT) 34 IU/l (normal value <40 IU/l) were within normal limits.
Contrast-enhanced computed tomography (CECT) scan revealed a well-defined, lobulated, heterogeneously enhancing mass lesion in the left para-aortic region opposite to the L2 vertebra, measuring 3.6 × 3.5 cm [Figure 1a]. It showed multiple non-enhancing areas suggestive of necrosis and cystic changes. Left renal vein was splayed anteriorly and invaded by the lesion with evidence of extension of tumor into left renal vein. Left renal artery was displaced posteriorly by the mass with loss of fat planes. There was no significant retroperitoneal lymphadenopathy. Bilateral kidneys were normal.
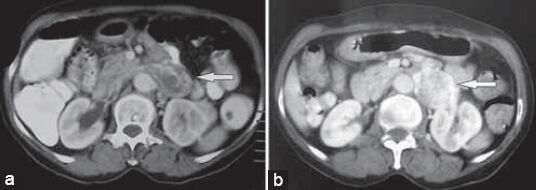
- 61-year-old hypertensive post-menopausal woman presented with a 2-year history of dull aching intermittent left hypochondrial pain that occasionally radiated to her back with paroxysmal attacks of palpitations and sweating, which was subsequently diagnosed as renal vein leiomyoma. a) Contrast-enhanced computed tomography (CECT) scan shows well-defined, lobulated, heterogeneously enhancing retroperitoneal mass of size 3.6 × 3.5 cm in the left para-aortic location, with the left renal vein being invaded by the tumor (arrow). b) Positron emission tomography computed tomography (PET CT) scan shows moderate fluorodeoxy glucose (FDG) uptake (SUV 4.7) in the tumor (arrow).
Positron emission tomography (PET) scan revealed moderate uptake [standardized uptake value (SUV) 4.7] in the retroperitoneal mass [Figure 1b]. In view of the clinical and radiological features, a provisional diagnosis of left retroperitoneal paraganglioma was made. Plasma metanephrines and urinary vanillyl mandelic acid were within normal limits. Metaiodobenzylguanidine (MIBG) scan showed no uptake in the mass and anywhere in the body.
As the nature of the lesion was not revealed by any of the investigations, decision for explorative laparotomy and excision of mass through left subcostal incision was made. A 3 × 4 cm soft tissue lobulated mass at the left renal hilum with extensive feeding vessels was identified. The mass was seen arising from the left renal vein and the renal artery was found to be adherent to the tumor. In view of the complex location of the mass in the renal hilum and the need for excision of the lesion with negative margins, left nephrectomy with complete en bloc excision of the mass was done [Figure 2a]. Histological findings showed whorled (fascicular) pattern of smooth muscle bundles separated by well-vascularized connective tissue. Smooth muscle cells were elongated with eosinophilic or occasional fibrillar cytoplasm and distinct cell membranes. There were few mitotic figures with no atypia. These features were consistent with renal vein leiomyoma [Figure 2b]. Postoperative course was uneventful and the patient was free of her symptoms when examined during the 6-month follow-up.
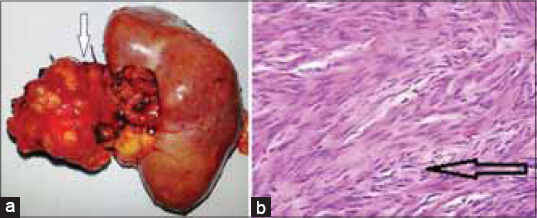
- 61-year-old hypertensive post-menopausal woman presented with a 2-year history of dull aching intermittent left hypochondrial pain that occasionally radiated to her back with paroxysmal attacks of palpitations and sweating, which was subsequently diagnosed as renal vein leiomyoma. a) Gross specimen shows the en bloc resected specimen with well-defined, lobulated tumor in relation to the left renal hilum. b) Histopathology slide with hematoxylin and eosin staining shows smooth muscle bundles separated by well-vascularized connective tissue with no atypia, suggestive of leiomyoma (arrow).
DISCUSSION
Primary tumors of vascular origin are rare and usually present as smooth muscle tumors. They commonly arise from veins, like endotheliomas from intima, fibrosarcoma from connective tissues, and leiomyosarcoma from smooth muscle of media.[45] Tumors of vascular origin are predominantly malignant. Benign variants as leiomyomas are very rare.[6] Inferior vena cava is the commonest site of origin of venous tumors, followed by long saphenous vein, femoral vein, internal jugular vein, iliac vein and, very rarely, renal vein. According to the literature, renal vein leiomyomas are found in women over 50 years of age and are predominantly left sided as was seen in our case. Presenting symptoms are abdominal pain, backache, and a palpable lump.
Preoperatively it is difficult to differentiate benign venous tumors from malignant venous tumors even on CECT scan, unless the tumors demonstrate local or distant spread. Chura et al., reported that PET scan–positive smooth muscle tumors are not necessarily malignant. Even benign tumors like leiomyomas can show increased fluorodeoxy glucose (FDG) avidity due to increased vascularity.[7] Total surgical excision of the tumor with a segment of renal vein with or without nephrectomy is the treatment of choice. Tumors arising from renal vein are commonly leiomyosarcomas[8] and frequently require nephrectomy in view of their complex location. Resection of the tumor with reconstruction of the renal vein is only possible in rare circumstances.
Douma et al.,[9] reported a 43-year-old woman with left renal vein leiomyosarcoma with paroxysmal attacks of hypertension accompanied by dizziness and sweating, resembling a paraganglioma. Similarly, our patient also clinically and radiologically presented as a case of paraganglioma. To our surprise, the mass was found to be arising from the left renal vein and histopathology revealed a diagnosis of renal vein leiomyoma.
CONCLUSION
We report a rare case with unusual presentation of renal vein leiomyoma mimicking a paraganglioma. To the best of our knowledge, only three cases of renal vein leiomyoma have been reported so far and none of them had such an unusual presentation.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/1/42/137836
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Primary smooth muscle tumors of the inferior vena cava. Ann Surg. 1971;174:1009-18.
- [Google Scholar]
- Leiomyosarcoma of veins. Report of 2 cases and review of the literature. Cancer. 1960;13:96-101.
- [Google Scholar]
- Leiomyosarcoma of the inferior vena cava: Report of a case and review of the literature. Ann Surg. 1976;184:169-73.
- [Google Scholar]
- Leiomyosarcoma of the inferior vena cava. Diagnosis and surgical management. Arch Surg. 1976;111:1081-5.
- [Google Scholar]
- Positron emission tomography and leiomyomas: Clinicopathologic analysis of 3 cases of PET scan-positive leiomyomas and literature review. Gynecol Oncol. 2007;104:247-52.
- [Google Scholar]
- Leiomyosarcoma of the renal vein: Case report and review of the literature. Urol Oncol. 2005;23:22-6.
- [Google Scholar]
- Leiomyosarcoma of renal vein, initially resembling pheochromocytoma. Clin Exp Hypertens. 2012;34:429-31.
- [Google Scholar]






