Translate this page into:
A Rare Case of Oropharyngeal Teratoma Diagnosed Antenatally with MRI
Address for correspondence: Dr. Chandrahasa Sharabu, Department of Radiology, Manju Sudha Hospital, Hyderabad, Andhra Pradesh, India. E-mail: hasa8699@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Oropharyngeal teratomas are extremely rare congenital tumors and have an incidence rate of one in 35,000-200,000 newborn babies/neonates. Oropharyngeal teratomas may cause life threatening airway obstruction to a newborn. Early diagnosis with ultrasound and magnetic resonance imaging (MRI) is essential to plan management. Here, we present a rare case of oropharyngeal true teratoma diagnosed with MRI antenatally in a fetus at 34 weeks of gestation in a 25-year-old female who was being evaluated for polyhydraminos. We found MRI to be more helpful for antenatal diagnosis, counseling, and management than ultrasonography and computed tomography (CT).
Keywords
Diagnosed antenatally
MRI better modality
oropharyngeal teratoma
INTRODUCTION

Teratoma is a true neoplasia consisting of cells from all three germ layers. Teratomas in the head and neck account for 2–9% of all teratomas at birth and teratomas in the oropharynx are extremely rare. Here, we present a case of oropharyngeal teratoma that was diagnosed antenatally.
CASE REPORT
A 25-year-old female (gravida 2 para 1) was seen by a radiologist for evaluation of polyhydraminos. Her previous anomaly scan reports were normal. Ultrasound evaluation of the fetus revealed no significant abnormalities [Figure 1]. Fetal spine and facial structure were normal. Fetal stomach bubble was seen and was found to be relatively small in size. Placenta was normal. Amniotic fluid volume was greater than normal, amniotic fluid index (AFI) measured 45 cm. Some problem in fetal swallowing due to small stomach and polyhydraminos was suspected. A fetal magnetic resonance imaging (MRI) was done to evaluate cause of acute polyhydramnios and relatively small size of the stomach.
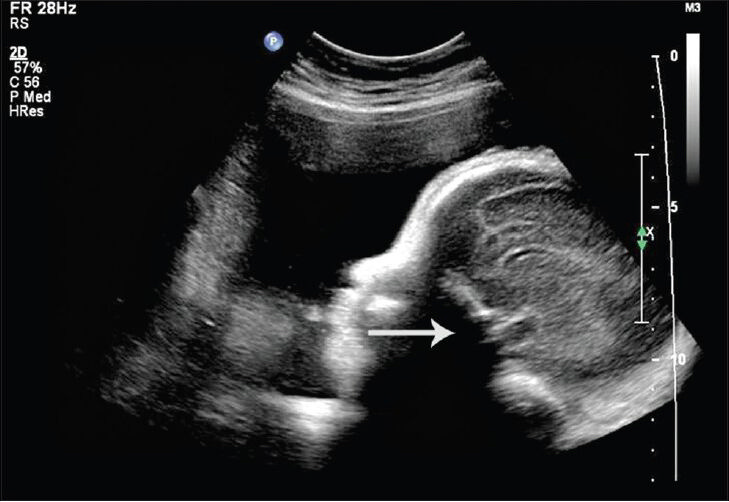
- 25-year-old female with gravida 2 para 1 evaluated for polyhydraminos. Fetus was later diagnosed with oropharyngeal teratoma. Ultrasound image of fetal face in sagittal projection shows shadow from the hard palate (arrow) obscuring the pharyngeal mass.
Fetal MRI done on 1.5 T Philips Achieva magnet with T2W turbo spin echo sequences and balanced turbo field echo sequences. Sagittal [Figure 2] and axial [Figure 3] images show well-defined mixed intensity lesion with cystic component measuring about 4.5 × 3.5 cm in the oropharyngeal region. No obvious sign of invasion of hard palate or nasopharynx was noted [Figure 2]. No other significant abnormality was noted in the fetus. No destruction of facial structure was found. Large amount of amniotic fluid was seen [Figure 2]. The lower and mid regions of the trachea were well visualized. The mandible appeared normal [Figure 2].
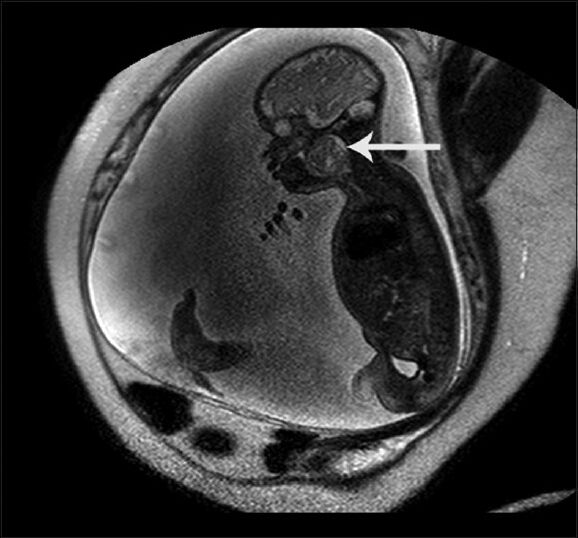
- 25-year-old female with gravida 2 para 1 evaluated for polyhydraminos. Fetus was later diagnosed with oropharyngeal teratoma. Sagittal image of Fetal MRI at 34 weeks gestation shows well-defined mixed intensity lesion with cystic component measuring about 4.5 × 3.5 cm in oropharyngeal region (arrow).

- 25-year-old female with gravida 2 para 1 evaluated for polyhydraminos. Fetus was later diagnosed with oropharyngeal teratoma. Axial image of Fetal MRI at 34 weeks of gestation shows well-defined mixed intensity lesion with cystic component measuring about 4.5 × 3.5 cm in oropharyngeal region (arrow).
Because of polyhydramnios and severe maternal discomfort, cesarean section was done at 35 weeks. After birth, the baby was found to be hypoxic with difficulty in breathing. Baby was intubated and airway was maintained. Surgery for tumor removal was planned and done on the fourth day after birth. At surgery, well-defined lobulated tumor measuring about 4.5 × 3.4 cm arising from palate was resected [Figure 4] and sent for histopathology examination. Post surgery, baby recovered well. Histopathology report proved it as immature teratoma [Figures 5 and 6]. After 4 weeks, the baby's serum alfa-feto-proteins were found to be elevated to 600 ng/ml. Parents were advised to consult a medical oncologist, who advised follow-up after 6 months. After 6 months, positron emission tomography - computed tomography [Figure 7] was done to rule any recurrence. The scan showed no signs of any recurrence or metastasis. Serum alpha-feto-protein was repeated and found to be 180 ng/ml. Medical oncologist advised chemotherapy and radiation but the parents did not agree to this treatment. Presently, the boy is 27 months old and doing well without any clinical symptoms.
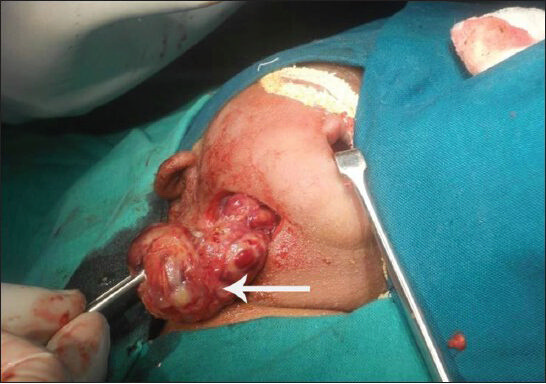
- 25-year-old female with gravida 2 para 1 evaluated for polyhydraminos. Fetus was diagnosed with oropharyngeal teratoma. Photograph during surgery shows the tumor mass (arrow).
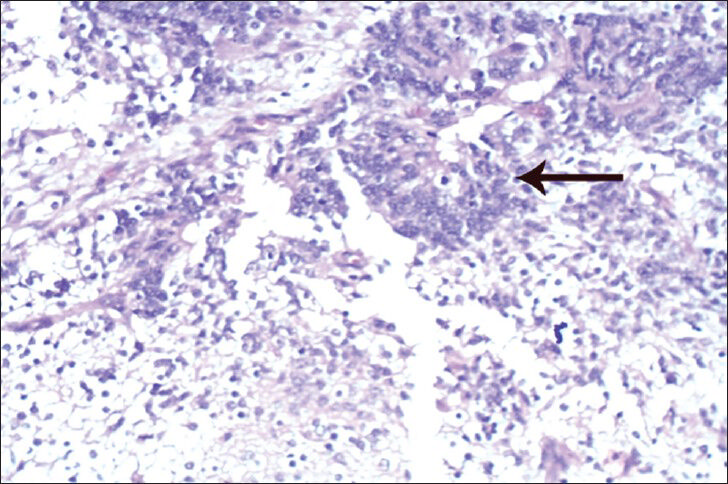
- 25-year-old female with gravida 2 para 1 evaluated for polyhydraminos. Fetus was diagnosed with oropharyngeal teratoma. Histopathology examination of the surgically removed mass shows mass composed of mature and immature elements of teratoma. Easiest immature element to identify is neuroepithelium with columnar cells forming rossettes and tubules (arrow). Tissue stained with hematoxylin and eosin, ×40.
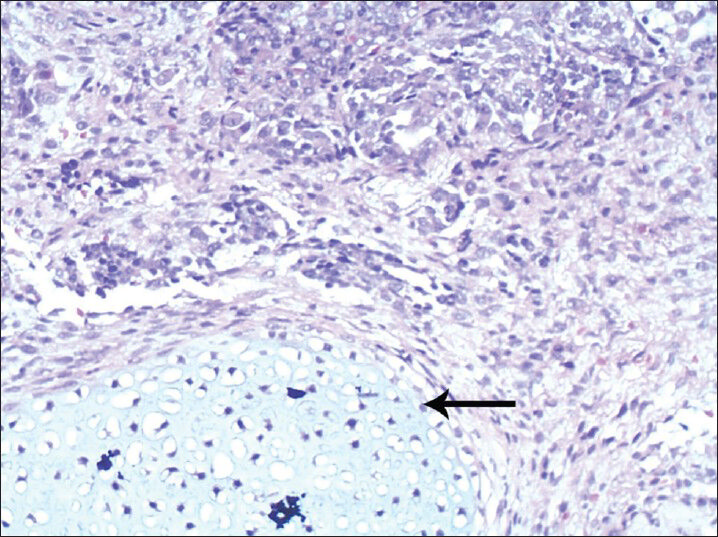
- 25-year-old female with gravida 2 para 1 evaluated for polyhydraminos. Fetus was diagnosed with oropharyngeal teratoma. Surgically removed mass stained with hematoxylin and eosin at ×45 shows mature cartilaginous tissue (arrow).
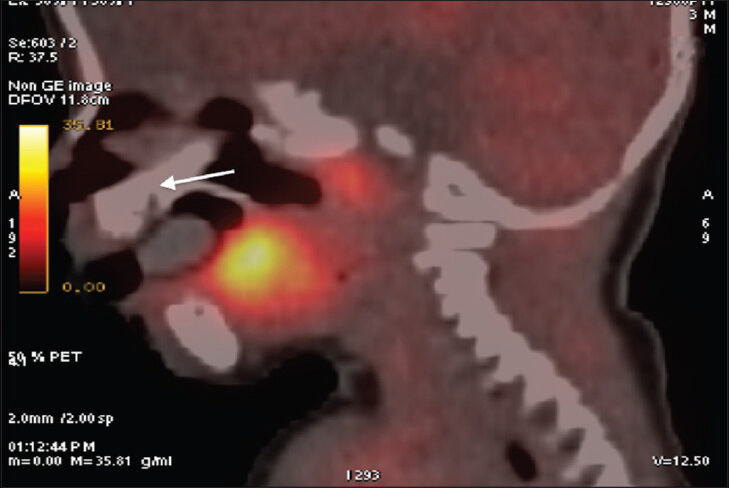
- 25-year-old female with gravida 2 para 1 evaluated for polyhydraminos. Fetus was later diagnosed with oropharyngeal teratoma. PET CT image of the child, 6-months posttreatment shows metabolic activity in the tongue and adenoids are physiological. Soft palate (arrow), where the original tumor was resected is normal indicating no recurrence of tumor.
DISCUSSION
Teratoma is a true neoplasia containing cells of all the three germ lines and represent 25-30% of all neonatal tumors. Most of the teratomas at birth are benign. Teratomas can occur in any part of the body but are most common in the sacro coccygeal region.[12] Teratomas of head and neck region are extremely rare and are most common in the cervical region followed by the oropharyngeal region. Incidence of oropharyngeal teratomas is one in 35,000-200,000 live births.[3]
Oropharyngeal teratomas appear as heterogenous masses with solid and cystic components and are believed to be result of migration and entrapment of mesoderm and endoderm with ectoderm during embryogenesis.[4]
The patient presented with polyhydraminos.[5] We found MRI more useful than ultrasound in the diagnosis and management. Sometimes the mass cannot be appreciated in USG due to the presence of shadows. In our case, ultrasound did not reveal any fetal abnormalities. Fetal MRI was helpful in diagnosing and revealing the extent of oropharyngeal involvement, defining tracheal anatomy, and excluding intracranial involvement. MRI is more useful to delineate soft tissues and can give a near accurate assessment of oropharyngeal extension.[678]
CT is rarely indicated for assessment of fetal anomalies. CT predicts calcifications and bony involvement that could change surgical management.[9] CT was not done antenatally in our case as the tumor was well-defined and limited to oropharynx and also to minimize radiation exposure to our patient. PET CT was done on the baby at 6 months of age to look for recurrence or metastasis.
Oropharyngeal teratoma can encroach airway and cause respiratory distress, progressive dysphagia, and aspiration pneumonia due to impaired swallowing mechanism.
Antenatal diagnoses of oropharyngeal teratoma is essential as it can radically change the treatment and allows the medical team to plan for ex utero intrapartum treatment (EXIT) or management during early neonatal period with surgery.
EXIT is a technique designed to allow partial fetal delivery via cesarean section while a safe fetal airway is established. Upon delivery of the fetal head, neck, and one or both upper limbs, a stepwise, sequential attempt to secure the neonates airway is performed via laryngoscopy, bronchoscopy, tracheostomy, or even resection of the obstructing mass. The placenta remains in utero to maintain feto-placental circulation and subsequently the continuance of fetal oxygenation. Once the newborn's airway is secured, the umbilical cord is clamped and delivery of the infant completed. This technique was first described in 1990 by Zerella and Finberg[10] to improve the survival of fetuses with head and neck teratomas and also by Levine et al., for treatment of epignathus.[10] The use of EXIT has also proven to be effective for the management of fetal airway obstruction due to a variety of other causes including congenital high airway obstruction syndrome (CHAOS), intrathoracic masses, and congenital diaphragmatic hernias.
CONCLUSION
This case describes use of MRI in prenatal diagnosis of oropharyngeal teratoma. MRI proved superior to ultrasound in diagnosing and delineating exact tumor location, size, extension, and was crucial in determining timing and mode of delivery. This information was also essential to counsel parents. The neonate had fetal distress. Surgical removal of the tumor removed the respiratory discomfort and the neonate progressed well. Oro-pharyngeal teratoma because of its potential to cause airway obstruction, though rare, should be considered while investigating polyhydramnios. Early antenatal diagnosis allows the medical team to plan mode of delivery, management through EXIT procedure or surgery during the early neonatal period and ultimately leads to better outcome.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/1/15/129261
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Neonatal cancer: A clinical perspective. J Obstet Gynecol Neonatal Nurs. 2000;29:423-31.
- [Google Scholar]
- Neonatal neoplasia. In: Campbell A, McIntosh N, eds. Forfar and Arneil's Text book of Pediatrics (5th ed). London: Churchill Livingstone; 1998. p. :290-1.
- [Google Scholar]
- Oral teratoma (epiganthus) with intracranial extension: A report of two cases. Prenat Diagn. 1993;13:945-52.
- [Google Scholar]
- Prenatal diagnosis of an epiganthus: A case report. J Ultrasound Obstet Gynecol. 2001;18:178-81.
- [Google Scholar]
- Prenatal magnetic resonance imaging of a cervical lymphangioma for assessment of the upper airway. Ann Otol Rhinol Laryngol. 202;;11:464-5.
- [Google Scholar]
- MRI imaging of fetal neck masses with airway compromise: Utility in delivery planning. Pediatr Radiol. 2001;31:727-31.
- [Google Scholar]
- MRI for assessment of the malformed fetus. Baillieres Best Pract Res Clin Obstet Gynecol. 2000;14:629-50.
- [Google Scholar]
- The ex utero intrapartum treatment procedure: Looking back at the EXIT. J Pediatr Surg. 2004;39:375-80.
- [Google Scholar]






