Translate this page into:
Ovarian Artery Embolization in a Case of Refractory Obstetric Hemorrhage

*Corresponding author: Vikash Jain, Department of Radiology, N M Virani Wockhardt Hospital, Kalawad Road, Rajkot - 360 001, Gujarat, India. vikashrjain007@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jain V. Ovarian artery embolization in a case of refractory obstetric hemorrhage. J Clin Imaging Sci 2019;9:30.
Abstract
Transcatheteric pelvic artery embolization (PAE) has now become accepted treatment for obstetric hemorrhage providing us the opportunity to control bleeding and avoiding surgical morbidity, preserving uterus, and subsequent fertility. There is little we can offer to the patient if bleeding persists after obstetric hysterectomy and embolization of bilateral uterine and hypogastric arteries. Here in, we present a case of refractory post obstetric hysterectomy hemorrhage where uterine and internal iliac artery embolization failed to control the bleeding. Aortic angiogram showed active contrast extravasation from the ovarian artery, which was successfully embolized with good clinical outcome.
Keywords
Ovarian artery embolization
Obstetric hemorrhage
Uterine artery embolization
INTRODUCTION
Obstetric hemorrhage is the leading cause of maternal mortality in the world, accounting for 25% of maternal deaths.[1] Primarily postpartum hemorrhage (PPH) can be tackled with conservative measures involving uterine packing, uterotonic agents, repair of genital lacerations, and balloon tamponade. Surgery in the form of hysterectomy and hypogastric artery ligation is reserved for refractory cases.
Ever since it was first described in 1979, uterine artery embolization (UAE) has a very high reported technical and clinical success rate.[2] However, in a few cases, bleeding may be refractory to PAE and even hysterectomy where the source of hemorrhage may be an extrauterine site or through collaterals.
CASE REPORT
A 38-year-old primipara got pregnancy with twin gestation after in vitro fertilization following 14 years of married life. She had pregnancy induced hypertension and also required Os tightening surgery at 7th month of amenorrhea. Elective cesarean section (CS) was done in an outside hospital; however, after CS, she had massive PPH. Conservative measures failed, and after 5 h, obstetric hysterectomy was done for her. As there was increase drain output post-procedure with tachycardia and hypotension, the patient was referred to our hospital for further management. Total 7 units of whole blood and 2 units of fresh frozen plasma were given to her during transfer. On admission to our hospital, her hemoglobin was 7.4 gm/dl, TLC 17,300/cc, platelets 0.58 lakh/cc, INR 1.52, and Fibrinogen 225mg/dl. Considering increasing drain output and developing disseminated intravascular coagulation (DIC), 10 units of cryoprecipitate, 6 units of platelet concentrate, and 6 units of FFP was transfused overnight. Next morning there was persistent increasing drain output, fall in hemoglobin (4.5 gm%), tachycardia, and hypotension. Ultrasound abdomen showed moderate hemoperitoneum and left-sided intra-abdominal hematoma extending from perisplenic region to left iliac fossa. Intervention radiology team was consulted and pelvic artery embolization was planned.
Angiogram revealed she ligated bilateral uterine arteries in its ascending segment with no active leak [Figure 1a and b]. Empirically remaining stump of uterine arteries was embolized with PVA particles. Considering left sided hematoma, anterior division of the left internal iliac artery was empirically embolized with coils [Figure 1c]. The right anterior division of internal iliac artery was left alone. Despite embolization, the patient had increased drain output, persistent tachycardia, and hypotension, developed respiratory acidosis and had to be intubated.
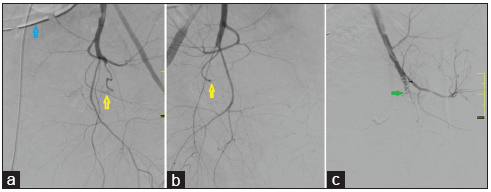
- A 38 year primipara presented with refractory post partum haemorrhage despite obstetric hysterectomy. Angiogram revealed (a,b) ligated bilateral uterine arteries (yellow arrows). Note surgical drain placed in pelvis (blue arrows). (c) Anterior division of left internal iliac artery embolized with coils (green arrows).
Repeat angiogram after 9 h of 1st embolization procedure showed occluded left internal iliac artery with no leak. An abdominal aortic angiogram was taken from L1-L2 vertebral level, which showed active contrast leak from hypertrophied left ovarian artery [Figure 2a and b]. The right ovarian artery was not delineated. The left ovarian artery was engaged with Sim-1 catheter (Cook, Bloomington, USA) and selectively cannulated with microcatheter (2.7 F, Progreat, Terumo Corporation, Tokyo, Japan) up to its mid-segment and embolized with 20% N-Butyl cyanacrylate (NBCA) + Lipiodol suspension (Guerbet, Villepinte, France). Post-embolization angiogram revealed complete occlusion of the left ovarian artery [Figure 2c].
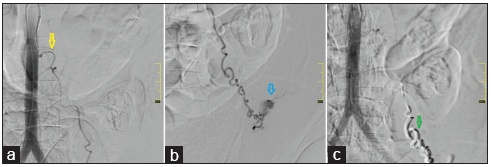
- A 38 year primipara presented with refractory post partum haemorrhage. Aortic angiogram showed (a) Left ovarian artery (yellow arrow) arising from anterolateral aspect of aorta at L2 vertebral level. (b) Selective catheterization of left ovarian artery with progreat microcatheter demonstrating active contrast leak (blue arrow). (c) Left distal ovarian artery completely embolized by NBCA + Lipiodol (green arrow).
After the ovarian artery embolization, the patient rapidly stabilized. Total leukoreduced red cell concentrate – 15, platelet concentrate – 10, fresh frozen plasma – 12, cryoprecipitate – 10, and one single donor platelet were transfused to her in the hospital. Serial ultrasonography was done which showed resolving left-sided intraperitoneal hematoma. The patient was discharged to home after 10 days of admission and doing well at 2 years telephonic follow-up.
DISCUSSION
Transcatheter PAE now plays an important role in the treatment of intractable PPH.[3] Embolization of the uterine arteries is effective in most cases; however, few require embolization of anterior-division branches of the internal iliac arteries. Despite this, there are few odd cases like ours who continue to bleed. Collateral source of blood supply to the uterus may play an important in them. The ovarian artery is one such natural collateral to the uterus.[4]
During an obstetric hysterectomy, the ovarian arteries are ligated in the broad ligament or the infundibulopelvic ligament during salpingo-oophorectomy. However, there are cases reported in the medical literature of active hemorrhage from ovarian artery post-hysterectomy, which were managed successfully by percutaneous ovarian artery embolization.[5,6]
Wang et al. in a series of eight patients presenting with massive persistent PPH after bilateral hypogastric – UAE demonstrated ovarian source of bleeding by selective ovarian artery angiogram. Ovarian arteries were then successfully embolized, leading to good clinical outcome in all eight patients.[4] In this scenario, CT angiography may play a pivotal role in identifying the bleeder simplifying subsequent embolization procedure.
Flush aortogram performed at the level of the L1–L2 vertebral level often demonstrates the pelvic bleeding vessels and depict the origin of the ovarian arteries.[7] Ovarian artery embolization is technically challenging as it is difficult to cannulate and distally navigate microcatheter into the ovarian artery. Furthermore, there is no consensus regarding the embolizing agent and various agents such as PVA, Gelfoam pledget, and coils have been used for ovarian artery embolization.[4-6] Considering that the patient was going into DIC, NBCA was preferred in this case. To the best of our knowledge, this is the 1st reported case in which NBCA has been used for embolization.
There is the concern of ovarian failure post ovarian artery embolization; however, in our case, it was done as a desperate life-saving measure. Moreover, hysterectomy was already done for her, so fertility was not of any concern and other ovary was preserved in case of ipsilateral ovarian failure.
CONCLUSION
In all such cases of intractable pelvic hemorrhage ovarian arteries should be evaluated particularly when there is persistent bleed despite uterine artery embolization or ligation or hysterectomy. A check aortic angiogram after UAE embolization to look for ovarian source may be considered as a routine protocol. Although bleeding from ovarian artery is rare, it may be a life-threatening cause of postoperative pelvic hemorrhage, and transcatheter embolization is the highly recommended in such cases.
Declaration of patient consent
The author certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Prevalence and risk factors of severe obstetric haemorrhage. BJOG. 2008;115:1265-72.
- [CrossRef] [PubMed] [Google Scholar]
- Uterine artery embolization in the treatment of postpartum uterine hemorrhage. J Vasc Interv Radiol. 2011;22:169-76.
- [CrossRef] [PubMed] [Google Scholar]
- The Role of Emergency and Elective Interventional Radiology in Postpartum Hemorrhage. 2007. Royal College of Obstetricians and Gynaecologists Good Practice Guideline. No. 6. Royal College of Obstetricians and Gynaecologists, London: Published; Available from: http://www.rcog.org.uk/womens-health/clinical-guidance/roleemergency-and-electiveinterventional-radiology-postpartum-haem (accessed )
- [Google Scholar]
- Ovarian artery embolization supplementing hypogastric-uterine artery embolization for control of severe postpartum hemorrhage: Report of eight cases. J Vasc Interv Radiol. 2009;20:971-6.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous embolization of the ovarian artery in the treatment of pelvic hemorrhage. AJR Am J Roentgenol. 1988;150:1337-8.
- [CrossRef] [PubMed] [Google Scholar]
- Successful embolization of an ovarian artery pseudoaneurysm complicating obstetric hysterectomy. Cardiovasc Intervent Radiol. 2005;28:113-6.
- [CrossRef] [PubMed] [Google Scholar]
- Utility of nonselective abdominal aortography in demonstrating ovarian artery collaterals in patients undergoing uterine artery embolization for fibroids. J Vasc Interv Radiol. 2001;12:841-5.
- [CrossRef] [Google Scholar]






