Translate this page into:
Pylephlebitis with Liver Abscess Secondary to Chronic Appendicitis: A Radiological Conundrum
Address for correspondence: Dr. Divya Santosh, Department of Radiology and Diagnostic Imaging, University of Alberta Hospital, 2A2.41 204, 10745-83rd Avenue North West, Edmonton, Alberta T6E 2E5, Canada. E-mail: divyasantosh@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Septic thrombophlebitis of the portal vein and/or its intra-hepatic branches (pylephlebitis) with associated liver abscess formation is a rare and potentially fatal complication of intra-abdominal infection. We present such a case that was caused by missed chronic appendicitis. Imaging findings can be complex and mimic other diseases leading to a diagnostic conundrum. Radiologists need to be knowledgeable of this challenging condition to prevent misdiagnosis and because prompt treatment is often life-saving.
Keywords
Chronic appendicitis
liver abscess
pylephlebitis

INTRODUCTION
Pylephlebitis was first described by Waller in 1846 as the source of a liver abscess.[1] It is a rare and potentially fatal complication of intra-abdominal sepsis. Imaging appearances are often complex and can mimic malignancy. In our case, the condition was initially misdiagnosed on computed tomography (CT) as cholangiocarcinoma. Subsequently, the diagnosis of pylephlebitis with liver abscess secondary to appendicitis was made on magnetic resonance imaging (MRI). However, the absence of a convincing clinical picture for sepsis created a conundrum, and further confirmatory tests were needed.
CASE REPORT
A 47-year-old man presented with a 3-month history of pyrexia, rigors, fatigue, and weight loss. The patient had no significant past medical history and no family history of cancer. An outpatient ultrasound showed an ill-defined mixed echogenic focus in the liver and portal vein thrombosis [Figure 1]. On hospital admission, he was noted to be febrile with a temperature of 38.6°C and blood tests showed a normocytic anemia (83 g/L), leukocytosis (13.5 × 109/L), elevated serum bilirubin (22 μmol/L), and elevated serum alkaline phosphatase (312 U/L). Hepatitis virus screen and blood cultures were negative. A diagnostic colonoscopy was negative for colorectal cancer. A contrast-enhanced CT examination demonstrated multiple low attenuating lesions in the right lobe of a non-cirrhotic liver with suppurative thrombus of the portal vein [Figure 2]. The findings at that time were postulated to represent an intra-hepatic cholangiocarcinoma (IHC) with portal vein invasion. On contrast-enhanced MRI, an ill-defined multiloculated cystic lesion was noted in the liver corresponding to the CT finding, showing a “clustered” appearance denoting a conglomerate pyogenic abscess. The occluded portal vein was expanded by material that had a similar appearance to the adjacent liver abscess, representing pylephlebitis. Mild intra-hepatic biliary dilatation was also present due to mass effect from the abscess [Figure 3]. The mesenteric veins were patent. Furthermore, a distended retrocecal appendix with increased wall enhancement was noted on MRI [Figure 3]. Based on the findings on MRI, a diagnosis of pylephlebitis with hepatic abscess secondary to appendicitis was rendered.
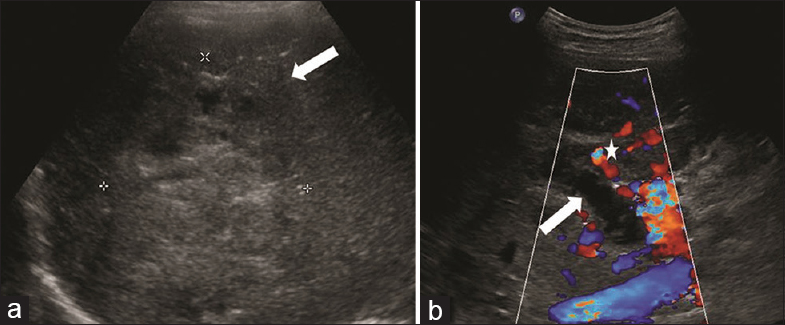
- A 47-year-old male presenting with a 3-month history of fever, rigors, and weight loss was diagnosed with pylephlebitis and hepatic abscess secondary to chronic appendicitis. Transverse ultrasound images of the right hepatic lobe demonstrate (a) an ill-defined mixed echogenic lesion (arrows) with few small cystic foci, and (b) a distended portal vein with no flow on color Doppler consistent with portal vein thrombosis (arrow). There are also associated small periportal collaterals consistent with cavernous transformation (asterisks).
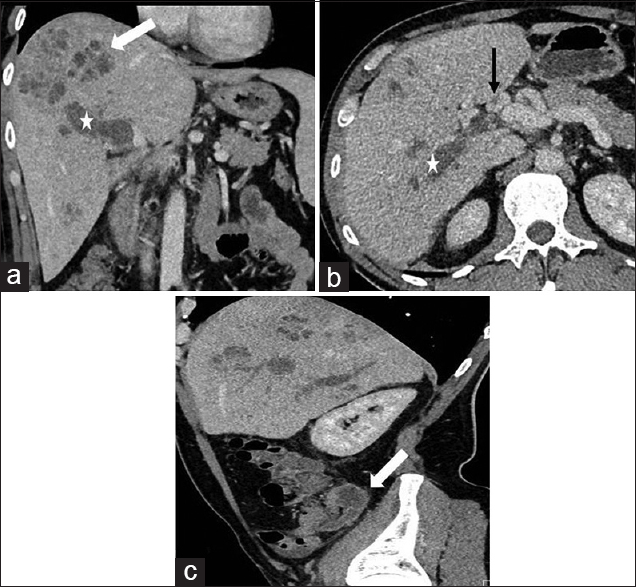
- A 47-year-old male presenting with a 3-month history of fever, rigors, and weight loss was diagnosed with pylephlebitis and hepatic abscess secondary to chronic appendicitis. (a) Coronal, (b) axial, and (c) sagittal contrast-enhanced computed tomography images of the abdomen. (a and b) Show occlusion of the intra-hepatic portal vein with expansile hypodense material (asterisks) consistent with pylephlebitis, periportal collaterals (black arrow) consistent with cavernous transformation and an ill-defined pyogenic abscess (white arrow) with a “clustered” appearance, (c) demonstrates a dilated appendix (white arrow) with only minimal wall irregularity in the right lower quadrant as well as pylephlebitis (asterisks) within the liver.
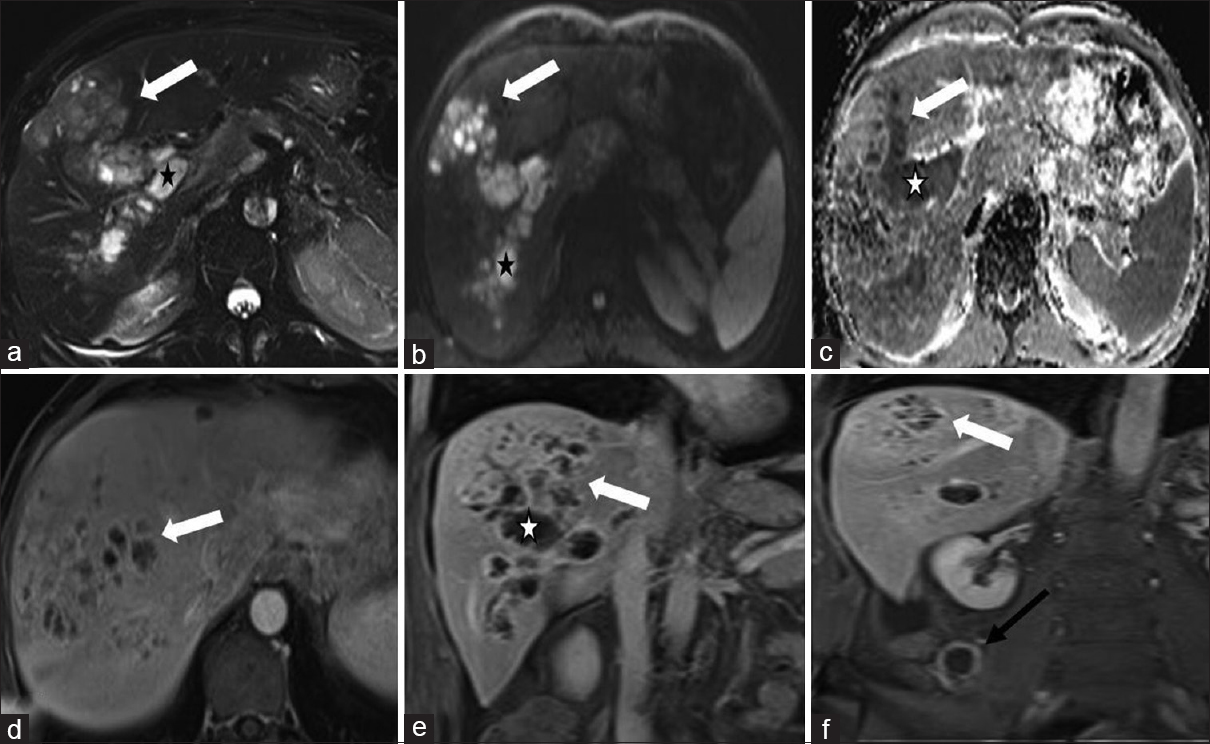
- A 47-year-old male presenting with 3 months history of fever, rigors, and weight loss was diagnosed with pylephlebitis and hepatic abscess secondary to chronic appendicitis. (a) Axial T2-weighted fat-suppressed magnetic resonance image: Expansion and occlusion of intra-hepatic portal vein by heterogeneous T2 hyperintense material - pylephlebitis (asterisk) which is contiguous with hepatic abscess (arrow), (b and c) axial diffusion-weighted magnetic resonance and apparent diffusion coefficient map: Restricted diffusion in pylephlebitis and hepatic abscess, (d) axial, and (e) coronal gadolinium-enhanced T1-weighted images: Hepatic abscess and pylephlebitis share a peripheral enhancement pattern with foci of linear internal vascularity, (f) coronal enhanced T1-weighted image shows a dilated appendix (black arrow) with mural hypervascularity.
However, the patient's clinical team felt that the radiologic findings were not entirely concordant with the clinical suspicion, which was not typical for an infectious process or appendicitis (the patient was only mildly tender in the right lower quadrant) and malignancy remained a diagnostic consideration. Additional tests including a nuclear medicine white cell scan and liver biopsy were requested. The white cell scan did not show an extrahepatic source of infection [Figure 4].
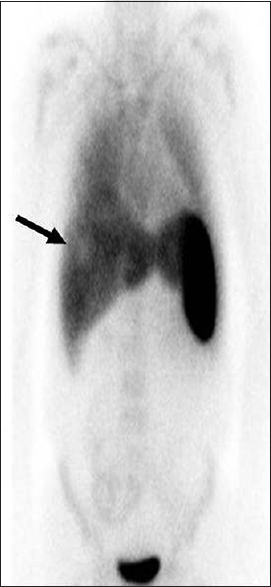
- A 47-year-old male presenting with a 3 months history of fever, rigors and weight loss was diagnosed with pylephlebitis and hepatic abscess secondary to chronic appendicitis. On the nuclear medicine white cell study with whole body coronal images performed at 24 h, a focus of photopenia (arrow) within the right lobe of the liver is noted corresponding to the hepatic abscess. No abnormal extrahepatic tracer accumulation was visualized to suggest an extrahepatic source for the sepsis.
However, the liver biopsy confirmed the diagnosis of abscess although cultures failed to identify the specific microorganism(s) involved.
The patient was treated with broad-spectrum antibiotics and anticoagulation. A follow-up CT at 6 weeks demonstrated significant interval resolution of the pylephlebitis and hepatic abscess [Figure 5]. Subsequently, an elective appendectomy was performed, and histology revealed chronic fibrous obliterative appendicitis.

- A 47-year-old male presenting with a 3-month history of fever, rigors, and weight loss was diagnosed with pylephlebitis and hepatic abscess secondary to chronic appendicitis. Axial (a) and coronal, (b) contrast-enhanced computed tomography images performed after treatment with antibiotics and anticoagulation at 6-weeks show interval improvement with a decrease in the size of the hepatic abscess (black arrow) and pylephlebitis (white arrow).
DISCUSSION
Pylephlebitis is described as septic thrombophlebitis of the portal vein and/or its intra-hepatic divisions. It begins with thrombophlebitis of small veins draining an area of infection. The extension of thrombophlebitis into larger veins leads to pylephlebitis, which can extend further to involve the mesenteric veins.
The true incidence of pylephlebitis is unclear but has been estimated at 2.7/1,00,000 person-years.[2] A review article reported 51 cases of pylephlebitis between 2001 and 2009 compared with 49 cases between 1971 and 2000.[3] The apparent higher incidence of pylephlebitis in recent years is probably artificial and reflects greater detectability of the disease due to improved access to high-quality cross-sectional imaging and a lower clinical threshold for performing imaging for investigating abnormalities. In a study of 100 cases of pylephlebitis, the mean age was 42 years (range 20 days to 77 years), and males (68%) were more affected than females.[3] Fever and abdominal pain are reported in over 80%, but patients may also complain of vague constitutional symptoms such as fatigue, anorexia, nausea and vomiting, and diarrhea.[23] Jaundice, while rare, may suggest the presence of a liver abscess. Blood cultures are positive in <80% and are polymicrobial in 50%.[24]
On cross-sectional imaging, pylephlebitis manifests as enlargement and occlusion of the portal vein and/or its branches with intravascular thrombus. That shows heterogeneous consistency on CT, signal alteration on T1- and T2-weighted MR sequences and heterogeneous enhancement following contrast administration distended portal vein with intravascular thrombus of variable echogenicity and no venous Doppler signals on ultrasound. Periportal collaterals (cavernous transformation) may develop as rapidly as within 20 days of portal venous occlusion.[5] Up to 37% of cases of pylephlebitis are complicated by a pyogenic liver abscess.[3] Typically, the pyogenic abscess is located in continuity with the pylephlebitis, and both share similar imaging appearances in terms of CT attenuation, signal intensities on T1- and T2-weighted MR sequences and postcontrast enhancement. A pyogenic liver abscess characteristically manifests as a cluster of small foci that show progressive coalescence on repeat imaging into a discrete larger collection. Pyogenic liver abscess occurs secondary to hematogenous spread, therefore, are multifocal as opposed amoebic or other abscess. During the early evolutionary stage, the abscess exhibits ill-defined margins with small cystic non-enhancing areas, and there is a heterogeneous enhancement in the surrounding inflamed liver parenchyma. Over time, the abscess becomes more organized and develops a well-circumscribed outline with a thick peripherally enhancing rim and internal fluid and debris.[6]
The main differential diagnosis for pylephlebitis with a pyogenic liver abscess is a primary liver malignancy such as hepatocellular carcinoma (HCC) or mass-forming IHC with portal vein involvement.[7] HCC mostly occurs in a cirrhotic liver in a patient with predisposing factors (hepatitis B and C, etc.) although rarely may occur de-novo in normal liver. It characteristically shows arterial hyperenhancement followed by portal or delayed phase washout and has the propensity to invade the portal vein.[7] The incidence of portal vein tumor thrombosis (PVTT) involving the portal vein or branches in advanced HCC at the time of diagnosis is 40-90%.[8] In Zhong et al., systematic review the frequency of microscopic PVTT ranges from 0% to 75%. The expansile tumor thrombus shows similar CT density, MR signal intensity, and enhancement as the primary HCC.[7] The incidence of intra-hepatic cholangiocarcinoma (IHC) has increased overtime. Of all the cholangiocarcinoma cases in Singal et al., study, the incidence of IHC increased from 49% during 1998-2003 to more than 60% during 2003–2007. IHC typically shows peripheral arterial enhancement followed by progressive delayed centripetal hyperenhancement.[9] The delayed hyperenhancement in IHC is attributed to the presence of dense fibrous stroma in the tumor.[9] Unlike a pyogenic liver abscess, cystic change is rare in IHC. A clinical picture favoring sepsis such as the presence of fever, chills, and leukocytosis is helpful in differentiating a pyogenic abscess from malignancy. Ancillary features that favor a diagnosis of IHC include capsular retraction of the liver, biliary obstruction, and evidence of metastases.[9] IHC generally causes extrinsic narrowing or occlusion of the adjacent portal vein, but frank vessel invasion is rare.
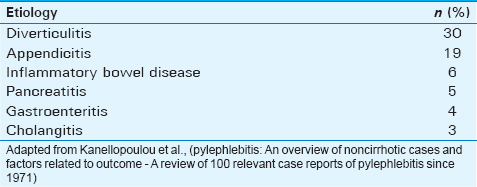
Pylephlebitis is caused by hematogenous dissemination of sepsis from sources of intra-abdominal infection located in regions drained by the portal and splanchnic systems.[234] The most common inciting etiologies for portal pylephlebitis are diverticulitis, acute appendicitis, inflammatory bowel disease, pancreatitis, and gastroenteritis [Table 1].[23] In our case, the pylephlebitis and pyogenic liver abscess were secondary to chronic appendicitis. There is controversy regarding the usage of term “chronic appendicitis” versus “recurrent appendicitis.” The exact pathogenesis of this condition is unknown, but it is postulated to be due to persistent partial appendiceal obstruction.[10] Nonetheless, chronic appendicitis is a rare cause of appendicitis, and is typically associated with vague symptoms and may be clinically occult. As such, it is commonly a delayed or missed diagnosis and one that is reliant on histology. Unlike acute appendicitis, chronic appendicitis is not regarded as a surgical emergency and appendectomy is often performed electively.
The combination of improved diagnosis by high-quality multimodality imaging and treatment with powerful broad-spectrum antibiotics has dramatically decreased the 100% preantibiotic era fatality rate of pylephlebitis to 19–32%. Nonetheless, the mortality rate remains high due to delays in diagnosis and treatment. Death is most commonly due to sepsis or peritonitis while thrombus propagation into the superior and inferior mesenteric veins may result in bowel ischemia and infarction.[2] The percentage of thrombus extension to the superior mesenteric vein and splenic vein is 42% and 12%, respectively.[3] In Harnik et al., review the percentage of isolated mesenteric vein thrombosis secondary to intra-abdominal causes ranges from 16% to 96%.
The use of anticoagulation to reverse or prevent thrombus propagation is reported to be beneficial but has not been universally adopted.[2] A course of anticoagulation over 3 months led to almost complete resolution of the portal venous thrombosis in our case.
CONCLUSION
Pylephlebitis with a pyogenic liver abscess secondary to subclinical intra-abdominal infection from chronic appendicitis is a rare condition associated with a high mortality rate if not treated promptly. The clinical presentation can be nonspecific, and the imaging findings are often complex resulting in delayed diagnosis and management. Radiologists need to be familiar with this condition including the imaging manifestation of the disease.
Financial support and sponsorships
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2016/6/1/37/190894
REFERENCES
- Pylephlebitis: An overview of non-cirrhotic cases and factors related to outcome. Scand J Infect Dis. 2010;42:804-11.
- [Google Scholar]
- Septic thrombophlebitis of the portal vein (pylephlebitis): Diagnosis and management in the modern era. Clin Infect Dis. 1995;21:1114-20.
- [Google Scholar]
- Cavernous transformation of the portal vein: Patterns of intrahepatic and splanchnic collateral circulation detected with Doppler sonography. AJR Am J Roentgenol. 1995;165:1151-5.
- [Google Scholar]
- Nonneoplastic liver disease: Evaluation with CT and MR imaging. Radiographics. 1998;18:827-48.
- [Google Scholar]
- Pylephlebitis and liver abscess mimicking hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int. 2003;2:221-5.
- [Google Scholar]
- A new classification for hepatocellular carcinoma with portal vein tumor thrombus. J Hepatobiliary Pancreat Sci. 2011;18:74-80.
- [Google Scholar]
- Varying appearances of cholangiocarcinoma: Radiologic-pathologic correlation. Radiographics. 2009;29:683-700.
- [Google Scholar]
- Chronic and recurrent appendicitis are uncommon entities often misdiagnosed. J Am Coll Surg. 1994;178:385-9.
- [Google Scholar]






