Translate this page into:
Gastropericardial Fistula as a Late Complication of Laparoscopic Gastric Banding
Address for correspondence: Dr. Adam A Rudd, Department of Radiological Sciences, 101 The City Drive South, Route 140, Orange, CA 92868, USA. E-mail: arudd@uci.edu
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Laparoscopic adjustable gastric banding (LAGB) is a bariatric procedure that is being performed with increasing frequency as an alternative management option for morbid obesity. Several common complications have been reported including gastric band slippage and associated pouch dilatation, intragastric erosion of the band, gastric wall perforation, and abscess formation. We present a case of gastropericardial fistula occurring nine years after an LAGB. There have been no previous documented cases of the complication after this procedure.
Keywords
Complications
gastropericardial fistula
laparoscopic adjustable gastric band

Introduction
Laparoscopic adjustable gastric banding (LAGB) is widely used in the management of morbid obesity. Common complications include gastric band slippage with associated pouch dilatation, intragastric erosion of the band, gastric wall perforation, and abscess formation.[1]
Gastropericardial fistulas are a rare and extremely life-threatening clinical entity. Case reports have documented it to occur secondary to a variety of conditions including recurrent diaphragmatic hernia,[2] gastric tube ulceration,[3] benign gastric ulcer erosion,[4] complications from laparoscopic Nissen fundoplication,[5] and Roux-en-Y gastric bypass.[6]
We present a case of gastropericardial fistula occurring nine years after an LAGB. There have been no previous documented cases of this complication after a laparoscopic band procedure.
Case Report
A 65-year-old woman with a history of morbid obesity status post-LAGB nine years before admission presented to the emergency department with shortness of breath for one week and acute onset of pleuritic chest pain for one day. She was afebrile but tachycardiac and had an elevated white count of 20,600 white blood cell/mcL. The patient was transferred from an outside hospital after computed tomography (CT) scan demonstrated a pericardial effusion, pneumoperitoneum, pneumopericardium, pulmonary embolism, and a dilated esophagus [Figure 1].
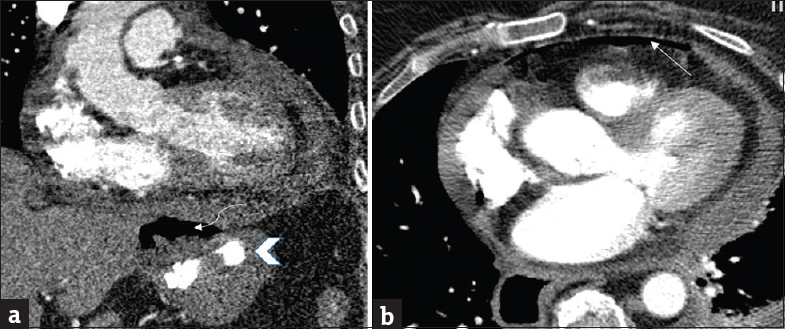
- 65-year-old female presents with chest pain and shortness of breath 9 years after placement of a laparoscopic gastric band and was transferred to our institution for higher level of care following the results of a computed tomography. (a) Coronal contrast-enhanced computed tomography of the chest in the mediastinal window from an outside hospital shows a laparoscopic gastric band (arrow head) and partial visualization of an abscess adjacent to the gastric band (curved arrow). No direct communication with the pericardium was initially seen. (b) Axial image demonstrates pneumopericardium (arrow) and small pericardial effusion.
The patient underwent gastric band decompression in the emergency room, was admitted to the intensive care unit, and was started on antibiotics. An upper gastrointestinal (UGI) examination performed at our hospital demonstrated an increased phi angle concerning for gastric band slippage but no definitive evidence of leak, perforation, or fistula [Figure 2]. The phi angle is defined as the superior angle formed by the longitudinal axis of the gastric band and the spinal column. A normal phi angle is 4–58°. Any angulation greater than 58° is consistent with gastric band slippage and will result in eccentric gastric pouch dilation.[1]
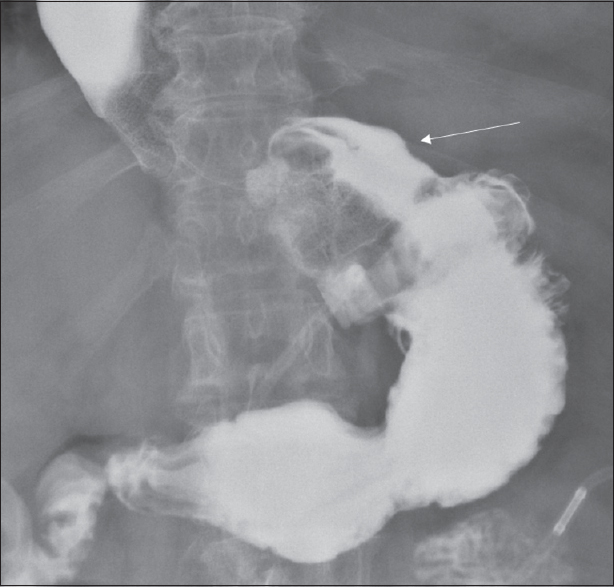
- Single contrast upper gastrointestinal examination in the supine anteroposterior view shows increased phi angle and prominent gastric pouch (arrow) concerning for mild lap band slippage.
Echocardiogram showed a pericardial effusion and evidence of impending tamponade with a preserved ejection fraction. The patient subsequently had a pericardiocentesis. Approximately, 340 mL of serous fluid was removed and a drain was placed. On day three, the patient underwent an esophagogastroduodenoscopy that showed erosion of the gastric band into the stomach just distal to the lower esophageal sphincter [Figure 3].
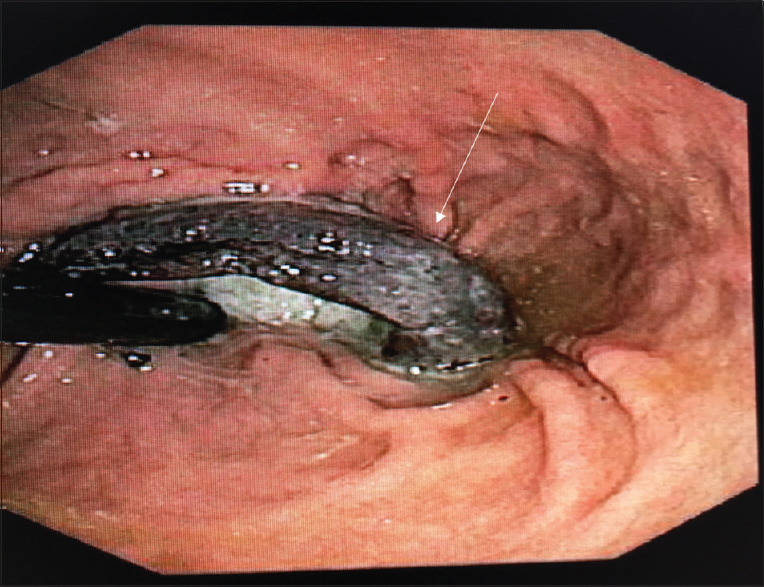
- Endoscopic image demonstrates an erosion of the lap band through the gastric wall (arrow).
On day four, patient went to the operating room for a laparoscopic gastric band removal. A large abscess was noted adjacent to the lap band which was drained intraoperatively. An omental patch was used to close off the abscess cavity and gastrostomy site. Postoperatively, the patient continued to complain of the left upper quadrant pain, left pleuritic chest pain, and shortness of breath. At this time, she was noted to have muddy brown output from her pericardial drain. A CT chest and abdomen were performed. This demonstrated a fistulous connection between a perigastric collection that was contiguous with the gastric body and the pericardium. Oral contrast was noted layering in the pericardium [Figure 4].
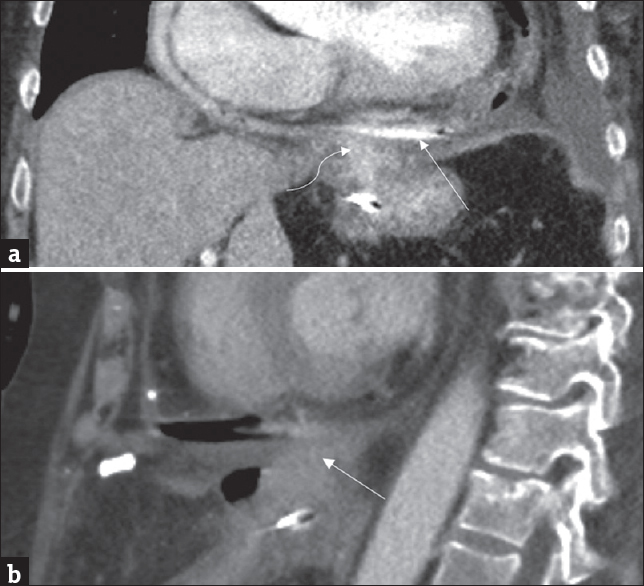
- (a) Coronal contrast-enhanced computed tomography shows collection of oral contrast within the pericardial sac (arrow). Communication between the inferior pericardial sac and a contrast-filled perigastric fluid collection is also seen (curved arrow). (b) Sagittal contrast-enhanced computed tomography showing fistulous tract between the perigastric fluid collection and the pericardial sac (arrow).
A left pleural drain was placed for a persistent left pleural effusion associated with shortness of breath. This provided symptomatic relief, improved oxygen saturation, and decreased the patients oxygen requirements. An additional UGI was performed to confirm a gastropericardial fistula [Figure 5]. Fistula was confirmed and managed nonoperatively. Pericardial drain output was monitored as diet was slowly advanced until output was minimal and the pericardial drain was removed. The patient was discharged on the 37th hospital day to a long-term acute care facility.
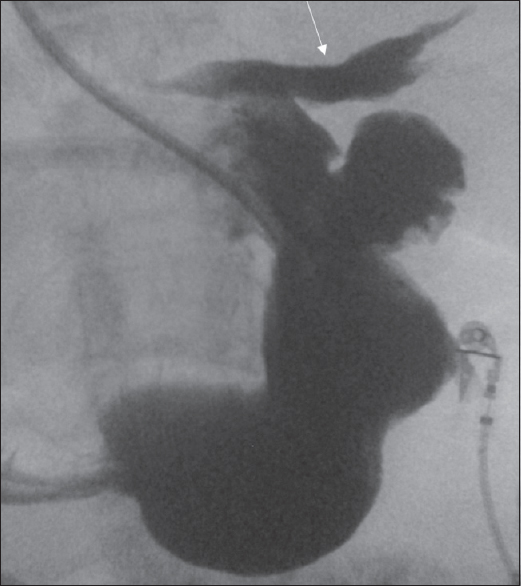
- Single contrast upper gastrointestinal in the anteroposterior view shows contrast extravasation into and layering along the inferior pericardial sac (arrow).
Discussion
Gastropericardial fistulas are extremely rare. However, given the significant morbidity and approximately 50% mortality associated with this condition, prompt diagnosis and intervention are pivotal to successful outcomes. Clinically, gastropericardial fistulas can present in a variety of ways but the classic presentation is referred pain to the left shoulder due to diaphragmatic or pericardial irritation. Advanced cases can present with the evidence of cardiac tamponade and/or shock.[7]
Pneumopericardium or hydropneumopericardium are common radiological findings that can be seen on both plain radiographs and chest CT. The differential diagnosis of pneumopericardium is vast and can be subdivided into two categories: traumatic and non-traumatic. Trauma is the most common etiology. In the absence of a history of trauma or recent procedure to suggest iatrogenic causes (i.e., endoscopy, intrathoracic procedure), the radiologist should consider infections from gas producing organisms and evaluate for potential abscesses and fistulous connections to the pericardial sac from etiologies such as liver abscesses, peptic ulcers, or gastric carcinomas.[2]
Definitive diagnosis of gastropericardial fistula can often be made on UGI fluoroscopic examination with water soluble contrast and a CT with oral contrast. Pneumopericardium, pericardial effusion and layering oral contrast can be seen within the pericardial sac. A fistulous connection may also be appreciated. Scanning patients in a prone position is often helpful when the diagnosis is suspected as this allows the enteric contrast to more readily communicate with the pericardial sac. Fluoroscopic examination has the additional benefit of identifying mucosal lesions, such as ulcerations/perforations that are often concomitantly seen with fistulous tracts.[7]
Treatment consists of either conservative management with pericardiocentesis and antibiotics or surgery. Surgery is considered the mainstay of treatment and consists of fistulectomy and surgical repair of the underlying pathology of the stomach that resulted in the fistula.[7] There have been only two reported cases of survival with conservative management.[89]
Conclusion
Essentially, any erosion through the stomach wall can lead to a gastropericardial fistula given their close anatomic proximity. Although there have been no documented cases of lap band gastropericardial fistulas, gastric ulceration, and perforation are well-documented complications. These can easily lead to fistulous connections with surrounding organs. Given the high morbidity, mortality, and the rarity, radiologists should have a high index of suspicion for the possibility of underlying gastropericardial fistula when pneumopericardium is noted.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2017/7/1/3/199053.
References
- Laparoscopic adjustable gastric banding: What radiologists need to know. Radiographics. 2012;32:1161-78.
- [Google Scholar]
- Gastropericardial fistula: A case report and review of literature. Emerg Med J. 2004;21:644-5.
- [Google Scholar]
- A case of gastropericardial fistula of a gastric tube after esophagectomy: A case report and review. World J Emerg Surg. 2010;5:20.
- [Google Scholar]
- Case report: Benign gastric ulcer erosion leading to a gastropericardial fistula in a patient with no known risk factors. Clin Imaging. 2014;38:547-9.
- [Google Scholar]
- Gastropericardial fistula after laparoscopic surgery for reflux disease. N Engl J Med. 2002;346:328-32.
- [Google Scholar]
- Gastropericardial fistula after Roux-en-Y gastric bypass: A case report. Surg Obes Relat Dis. 2006;2:533-5.
- [Google Scholar]
- Pneumopericardium due to gastropericardial fistula: A delayed, rare complication of gastric bypass surgery. Emerg Radiol. 2013;20:333-5.
- [Google Scholar]
- Pneumopericardium caused by giant gastric ulcer. AJR Am J Roentgenol. 1998;171:1669-70.
- [Google Scholar]
- Penetration of the pericardium by a gastric ulcer – Survival after pericardiocentesis. J Am Board Fam Pract. 1990;3:289-91.
- [Google Scholar]






