Translate this page into:
Superb Microvascular Imaging: Added Value and Novel Applications
Address for correspondence: Dr. Suheil Artul, Department of Radiology, Faculty of Medicine in the Galilee, EMMS Hospital Nazareth, Bar-Ilan University, Ramat Gan, Israel. E-mail: suheil_artul@hotmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Determining the presence and characteristics of vascular flow is an essential part of sonography interrogation. However, small vessels and low velocities are not always possible to depict with conventional color and power Doppler ultrasound. This can be frustrating, especially when the diagnosis depends mainly on the existence of vascular flow, the sonographic examination will be inconclusive, further imaging examinations will be required and diagnosis delayed. Superb microvascular imaging (SMI) is a novel vascular imaging mode, which provides visualization of low velocity and microvascular flow. SMI uses a clutter suppression algorithm to extract flow signals and depicts this information as a color overlay image or as a monochrome or color map of flow. By using SMI, high frame rates and high-resolution images remain maintained. With SMI, it is possible to visualize small vessels including their branches that, until now, it is possible to demonstrate only using contrast-enhanced ultrasound. Availability of this additional technology on all ultrasound machines may make some of the computed tomography scans unnecessary. In our paper, we describe six patients, aged 16–73 years, in which final diagnosis was achieved only with SMI and where conventional color and power Doppler failed. All these examinations were performed using Aplio 500 Platinum ultrasound unit (Toshiba Medical Systems, Tokyo, Japan).
Keywords
Doppler
superb microvascular imaging
ultrasound

INTRODUCTION
Vascular assessment with color Doppler is an indispensable part of most sonographic examinations and for certain clinical scenarios the presence or absence of blood flow determines treatment or need for further imaging studies. Conventional color Doppler's sensitivity to low velocities and small vessels however, is limited and may render studies inconclusive. Superb microvascular imaging (SMI) is a novel vascular imaging mode, which provides visualization of low velocity and microvascular flow. In this report, we describe its role as an adjunct tool when regular color Doppler failed.
CASE REPORTS
Case 1
A 73-year-old man presented with a two-day history of painless hematuria. His medical history was unremarkable and his physical examination was normal.
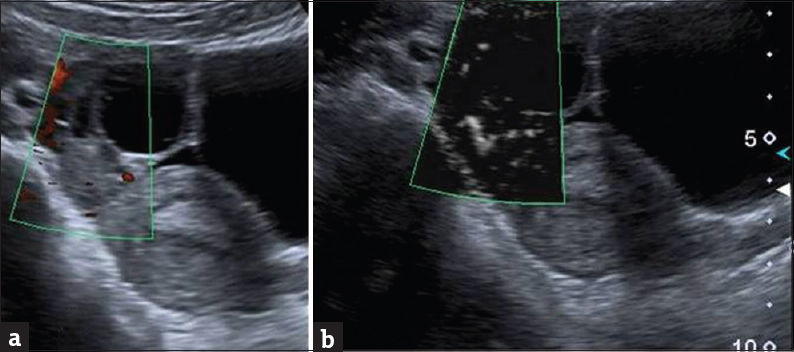
Urine tests showed that hematuria and urine culture was negative. Ultrasound revealed a 2 cm echogenic mass in the urinary bladder, avascular by both color and power Doppler [Figure 1]. The differential diagnosis included blood clot versus tumor. With superb microvascular imaging (SMI), blood flow was clearly seen in the lesion [Figure 2 and Video 1] making the diagnosis of tumor more likely. Cystoscopy and histology were positive for transitional cell carcinoma.

- A 73-year-old man presented with a 2-day history of painless hematuria, ultrasound power Doppler of a mass in the bladder that seems to be avascular.

- The same patient in Figure 1, superb microvascular imaging shows clearly the vessels in the mass (the white dots are the vessels).

- The same patient in Figure 1, superb microvascular imaging shows clearly the flow of the vessels in the mass.
Case 2
A 16-year-old previously healthy girl presented with right lower abdominal pain and vomiting for 10 h duration. On admission, she appeared ill and her right lower abdomen was tender on palpation. Blood count revealed mild leukocytosis (13,000 cells/mcL). Transabdominal ultrasound performed by the gynecology team showed a 2.5 cm cyst of the right ovary with no flow in the ovary by color and power Doppler, findings suspicious for ovarian torsion [Figure 3a]. The gynecologic team asked us to confirm the diagnosis using SMI in our department. With using SMI, flow was easily depicted in the ovary, and torsion was ruled out [Figure 3b]. Extending the ultrasound examination to the right abdomen, we found a thickened appendix consistent with appendicitis that confirmed at surgery.
- A 16-year-old previously healthy girl presented with right lower abdominal pain and vomiting of 10 h duration. (a) Power Doppler of ovary shows no flow and (b) using Doppler superb microvascular imaging the flow is clearly seen rolling out torsion of ovary.
Case 3
A 17-year-old girl presented with right lower quadrant pain and vomiting which began the day before. Her medical history was unremarkable. She appeared ill and her right lower abdomen was tender on palpation. She had no fever, and blood cell count was normal. Transabdominal ultrasound, performed by the gynecology team showed a 3 cm cyst of right ovary with no flow in the ovary by color and power Doppler, findings suspicious for ovarian torsion. The patient was referred to transabdominal SMI to confirm the diagnosis. We found a normal appendix and no flow in the ovary by both power Doppler and SMI, supporting the diagnosis of ovarian torsion [Figure 4]. Surgery revealed a 360° torsed ovary. The ovary was successfully detorsed, and the patient had an uneventful recovery.
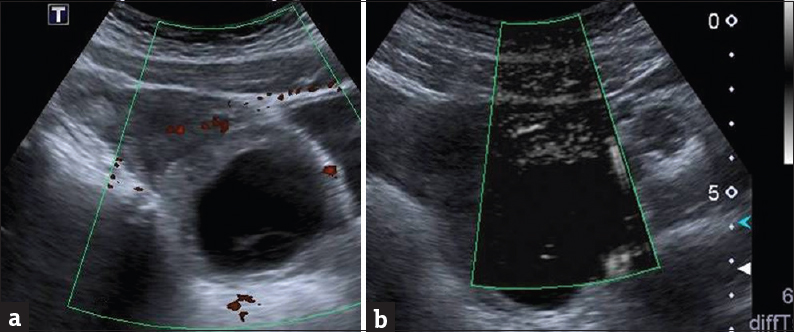
- A 17-year-old girl presented with right lower quadrant pain and vomiting which began the day before. (a) Power color failed to show flow in ovary mass that is adjacent to ovary mass and (b) superb microvascular imaging also failed to show flow that encouraged us to do the diagnosis of ovary torsion which was confirmed surgically.
Case 5
A 25-year-old pregnant woman was referred to ultrasound due to proteinuria. She was 13 weeks pregnant and feeling well. Ultrasound showed a 2.5 cm mass in the lower pole of the left kidney [Figure 7a]. Color and Power Doppler were inconclusive regarding vasculature. The differential diagnosis included tumor and dromedary hump and the patient was scheduled for renal magnetic resonance imaging (MRI). One week later, still before the MRI examination, it became possible for us to rescan with SMI. With SMI, the mass lesion showed normal-cortical vasculature [Figure 7b], confirming the diagnosis of dromedary hump.

- A 25-year-old pregnant woman was referred to ultrasound due to proteinuria. She was 13 weeks pregnant and feeling well. (a) Power color shows a mass in the lower pole of kidney with nonspecific vessel on it and (b) using superb microvascular imaging, it was possible to show normal cortical vessels leading with certainly to the diagnosis of dromedary hump.
Case 6
A 45-year-old man with a history of large B-cell lymphoma was referred to ultrasound for surveillance of a known hepatic hemangioma. SMI ultrasound showed a 1.5 cm echogenic lesion in the left lobe, with peripheral feeding vessels, typical of hemangioma [Figure 8].
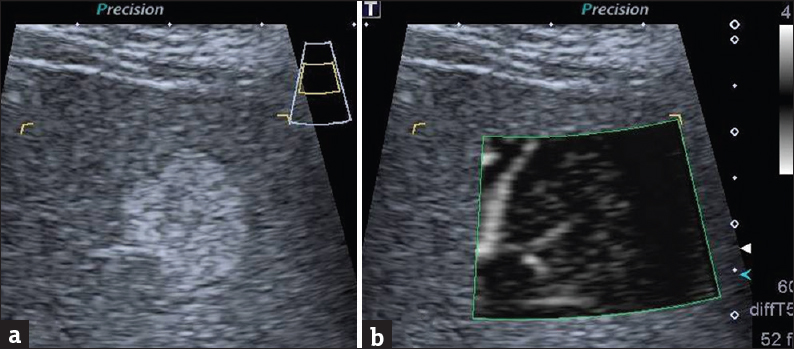
- A 45-year-old man with a history of large B-cell lymphoma was referred to ultrasound for surveillance of a known hepatic hemangioma. (a) Ultrasound B-mode shows a rounded echogenic mass in the liver and (b) superb microvascular imaging shows clearly the peripheral feeding vessel typical of hemangioma.
DISCUSSION
In this report, we describe six cases in which superb vascular imaging was crucial in achieving the final sonographic diagnosis.
Ultrasound is a first-line diagnostic tool for patients with painless macroscopic hematuria. In conventional ultrasound, the differentiation of blood clot from tumor within the bladder is often based on mobility and blood flow.[12] Clots are separate from the bladder wall, and tumors are attached. Clots may adhere to the bladder wall, and in these cases, evidence of flow within the mass is diagnostic for tumor. Nondemonstration of blood vessels, however, may be due to Doppler settings or low velocity flow, and may result in false negative results and delay patient treatment. In case number 1, the conventional ultrasound study was in fact false negative and SMI helped in detection of a bladder neoplasm, avoiding additional cross-sectional imaging.
Ovarian torsion is the twisting of an ovary that can result in compromised blood supply, ischemia, and necrosis. Early detection is essential to avoid irreversible ovarian damage. Diagnosis of ovarian torsion can be challenging; both clinical and ultrasound signs are not specific, and it is often difficult to demonstrate blood vessels by transabdominal ultrasound. Conversely, up to 60% of torsed ovaries exhibit blood vessels on color Doppler.[34] In case 2, by applying SMI, the full arborization of the ovarian vasculature was demonstrated. This prompted us to seek another cause for the patient's symptoms and made us confident that the ovary was not torsed. In contrast, not one vessel was demonstrated by SMI in case 3, raising our confidence to diagnose ovarian torsion. It is by no means our intention to proclaim that SMI should be the method of choice to rule in or rule out ovarian torsion and do admit to the gross lack of statistical evidence. Instead, what we would like to convey is that SMI is novel application with the potential to change the Doppler interrogation in cases of suspected torsion of ovaries.
In many rheumatic diseases, the response to treatment is generally clinically but also it depends in imaging improvement.[5] In case number 4, SMI was superb in visualization of the hyperemia, which is a sign, of active inflammation, that means failure of the current treatment and the urgent need to change therapy.
Normal variants can simulate disease and are a cause for misinterpretation, additional unnecessary diagnostic examinations, and patient anxiety. The dromedary hump of the kidney is a typical example. Color-Doppler evidence of normal cortical vascular arborization throughout the hump is used to rule out tumor, but may be equivocal due to patient size and position and increased respiratory rate.[67] In the case presented herein SMI confirmed the presence of normal vessels when conventional color-Doppler failed.
The vascular behavior of hepatic lesions is the basis for accurate diagnosis by MRI, computed tomography (CT), and contrast-enhanced ultrasound (CEUS).[8] MRI and CEUS are expensive and not widely available, and multiphase CT involves ionizing radiation. These drawbacks are magnified when patients require follow-up studies. Conventional duplex ultrasound is usually inconclusive regarding the vascularity of hepatic lesions and therefore used primarily for screening. In the liver case described above, SMI showed increased vascularity surrounding the lesion most likely representing peripheral feeding vessels typical of hemangioma.[9] These vessels are not easily demonstrated with conventional color or power Doppler.
CONCLUSIONS
We have demonstrated the value of SMI. Although our experience is very preliminary, we found that SMI is a promising tool with potential benefit for diverse clinical scenarios. Further studies are needed to confirm our findings.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2017/7/1/45/221871
REFERENCES
- Color Doppler sonographic findings in patients with transitional cell carcinoma of the bladder and renal pelvis. J Ultrasound Med. 1995;14:129-33.
- [Google Scholar]
- Radiologic evaluation of hematuria: Guidelines from the American College of Radiology's appropriateness criteria. Am Fam Physician. 2008;78:347-52.
- [Google Scholar]
- Pack of ice: Grey scale sign of testicular torsion. BMJ Case Rep 2014 pii: bcr2013202734
- [Google Scholar]
- Reversal of diastolic plateau in partial testicular torsion. J Clin Ultrasound. 2001;29:105-8.
- [Google Scholar]
- Detection of power Doppler ultrasound signals in rheumatic diseases using superb microvascular imaging (SMI): Comparison with conventional power Doppler ultrasound. Arthritis Rheumatol. 2015;67(Suppl 10):10.
- [Google Scholar]
- Evaluation of renal masses with contrast-enhanced ultrasound: Initial experience. AJR Am J Roentgenol. 2011;197:897-906.
- [Google Scholar]
- Superb micro-vascular imaging (SMI): Seeing the contrast in ultrasound without really using it. Austin J Radiol. 2015;2:1023.
- [Google Scholar]
- Spoke-wheel sign of focal nodular hyperplasia revealed by superb micro-vascular ultrasound imaging. QJM. 2015;108:669-70.
- [Google Scholar]
- Clinical utility of color Doppler sonography in the differentiation of hepatocellular carcinoma from metastases and hemangioma. J Ultrasound Med. 1997;16:51-8.
- [Google Scholar]






